Abstract
Purpose
To determine clinical characteristics and identify factors associated with better visual outcomes in patients who had vitrectomy for vitreous haemorrhage (VH) associated with Terson syndrome (TS).
Methods
The records of 48 patients (54 corresponding eyes) who underwent vitrectomy for VH associated with TS from January 2008 to December 2017 were retrospectively reviewed. The main outcome measure was the final postoperative visual acuity.
Results
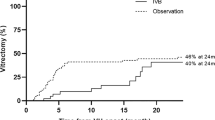
At the last visit, 34 eyes (63.0%) achieved a BCVA of 0.3 or better. Eyes associated with traumatic brain injury had a better visual outcome than those with primary intracerebral haemorrhage (P = 0.042). In the primary intracerebral haemorrhage group, patients with hypertension-induced intracranial haemorrhage (IH) showed poorer final visual acuities than the ruptured intracranial aneurysm group (P = 0.023). In the delayed vitrectomy group, epiretinal membrane and peripheral retina changes were more common (P < 0.05). However, the difference in final visual acuity between the early and delayed vitrectomy groups was not significant (P = 0.69).
Conclusion
Most of the patients obtained visual recovery after vitrectomy for TS. VH associated with ruptured intracranial aneurysm or traumatic brain injury or eyes without retinal haemorrhage are predictive of better prognosis. Although the timing of vitrectomy was not related to the final postoperative visual outcome, early vitrectomy by three months seems to suggest less epiretinal membrane formation, retinal tears, and retinal detachments.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Terson A. De l’hemorrhagie dans le corps vitre au cours de l’hemorrhagie cerebrale. Clin Ophthalmol. 1900;6:312.
Fountas KN, Kapsalaki EZ, Lee GP, Machinis TG, Grigorian AA, Robinson JS, et al. Terson hemorrhage in patients suffering aneurysmal subarachnoid hemorrhage: predisposing factors and prognostic significance. J Neurosurg. 2008;109:439–44.
Stienen MN, Lucke S, Gautschi OP, Harders A. Terson haemorrhage in patients suffering aneurysmal subarachnoid haemorrhage: a prospective analysis of 60 consecutive patients. Clin Neurol Neurosurg. 2012;114:535–8.
Garfinkle AM, Danys IR, Nicolle DA, Colohan AR, Brem S. Terson’s syndrome: a reversible cause of blindness following subarachnoid hemorrhage. J Neurosurg. 1992;76:766–71.
Ness T, Janknecht P, Berghorn C. Frequency of ocular hemorrhages in patients with subarachnoidal hemorrhage. Graefes Arch Clin Exp Ophthalmol. 2005;243:859–62.
Ogawa T, Kitaoka T, Dake Y, Amemiya T. Terson syndrome: a case report suggesting the mechanism of vitreous hemorrhage. Ophthalmology. 2001;108:1654–6.
Sakamoto M, Nakamura K, Shibata M, Yokoyama K, Matsuki M, Ikeda T. Magnetic resonance imaging findings of Terson’s syndrome suggesting a possible vitreous hemorrhage mechanism. Jpn J Ophthalmol. 2010;54:135–9.
Medele RJ, Stummer W, Mueller AJ, Steiger HJ, Reulen HJ. Terson’s syndrome in subarachnoid hemorrhage and severe brain injury accompanied by acutely raised intracranial pressure. J Neurosurg. 1998;88:851–4.
Joswig H, Epprecht L, Valmaggia C, Leschka S, Hildebrandt G, Fournier JY, et al. Terson syndrome in aneurysmal subarachnoid hemorrhage-its relation to intracranial pressure, admission factors, and clinical outcome. Acta Neurochir. 2016;158:1027–36.
Kuhn F, Morris R, Witherspoon CD, Mester V. Terson syndrome. Results of vitrectomy and the significance of vitreous hemorrhage in patients with subarachnoid hemorrhage. Ophthalmology. 1998;105:472–7.
Ritland JS, Syrdalen P, Eide N, Vatne HO, Overgaard R. Outcome of vitrectomy in patients with Terson syndrome. Acta Ophthalmol Scand. 2002;80:172–5.
Garweg JG, Koerner F. Outcome indicators for vitrectomy in Terson syndrome. Acta Ophthalmol. 2009;87:222–6.
Narayanan R, Taylor SC, Nayaka A, Deshpande R, St Aubin D, Hrisomalos FN, et al. Visual outcomes after vitrectomy for Terson syndrome secondary to traumatic brain injury. Ophthalmology. 2017;124:118–22.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Investig Ophthalmol Vis Sci. 2006;47:1236–40.
Moisseiev E, Goldstein M, Waisbourd M, Barak A, Loewenstein A. Long-term evaluation of patients treated with dexamethasone intravitreal implant for macular edema due to retinal vein occlusion. Eye. 2013;27:65–71.
Hoving EW, Rahmani M, Los LI, Renardel, de Lavalette VW. Bilateral retinal hemorrhage after endoscopic third ventriculostomy: iatrogenic Terson syndrome. J Neurosurg. 2009;110:858–60.
He T, Wu LN, Chen B, Xing YQ. Incidence and relative factors of Terson syndrome in patients with aneurysmal subarachnoid hemorrhage. Zhonghua Yan Ke Za Zhi. 2011;47:1096–101.
Srinivasan S, Kyle G. Subinternal limiting membrane and subhyaloid haemorrhage in Terson syndrome: the macular ‘double ring’ sign. Eye. 2006;20:1099–101.
Gnanaraj L, Tyagi AK, Cottrell DG, Fetherston TJ, Richardson J, Stannard KP, et al. Referral delay and ocular surgical outcome in Terson syndrome. Retina. 2000;20:374–7.
Sayman Muslubas I, Karacorlu M, Hocaoglu M, Ersoz MG, Arf S. Anatomical and functional outcomes following vitrectomy for dense vitreous hemorrhage related to Terson syndrome in children. Graefes Arch Clin Exp Ophthalmol. 2018;256:503–10.
Yokoi M, Kase M, Hyodo T, Horimoto M, Kitagawa F, Nagata R. Epiretinal membrane formation in Terson syndrome. Jpn J Ophthalmol. 1997;41:168–73.
Mao X, You Z. 25G compared with 20G vitrectomy under Resight non-contact wide-angle lenses for Terson syndrome. Exp Ther Med. 2017;14:1193–7.
Schultz PN, Sobol WM, Weingeist TA. Long-term visual outcome in Terson syndrome. Ophthalmology. 1991;98:1814–9.
Sharma T, Gopal L, Biswas J, Shanmugam MP, Bhende PS, Agrawal R, et al. Results of vitrectomy in Terson syndrome. Ophthalmic Surg Lasers. 2002;33:195–9.
Roux FX, Panthier JN, Tanghe YM, Gallina P, Oswald AM, Merienne L, et al. Terson’s syndrome and intraocular complications in meningeal hemorrhages (26 cases). Neurochir. 1991;37:106–10.
Velikay M, Datlinger P, Stolba U, Wedrich A, Binder S, Hausmann N. Retinal detachment with severe proliferative vitreoretinopathy in Terson syndrome. Ophthalmology. 1994;101:35–7.
Nacef L, Zghal-Mokni I, Allagui I, Haba B, Daghfous F, Gaigi S, et al. Indications and results of vitrectomy in Terson syndrome. La Tunis Med. 2004;82:461–4.
Augsten R, Konigsdorffer E, Strobel J. Surgical approach in terson syndrome: vitreous and retinal findings. Eur J Ophthalmol. 2000;10:293–6.
Daus W, Kasmann B, Alexandridis E. Terson syndrome. Complicated clinical course. Der Ophthalmol. 1992;89:77–81.
Shaw HE Jr., Landers MB 3rd. Vitreous hemorrhage after intracranial hemorrhage. Am J Ophthalmol. 1975;80:207–13.
Czorlich P, Skevas C, Knospe V, Vettorazzi E, Richard G, Wagenfeld L, et al. Terson syndrome in subarachnoid hemorrhage, intracerebral hemorrhage, and traumatic brain injury. Neurosurg Rev. 2015;38:129–36.
Acknowledgements
We thank Prof. Miao Li of the China–Japan Union Hospital, Jilin University for help with the neurological diagnosis and classification and Dr Shanshan Xu for the statistical consultation. This work was supported by the International Cooperation Foundation of Jilin Provincial Science and Technology Department (grant no. 20170414048GH) and the Natural Science Foundation of Jilin Province (grant no. 20180520118JH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Liu, X., Yang, L., Cai, W. et al. Clinical features and visual prognostic indicators after vitrectomy for Terson syndrome. Eye 34, 650–656 (2020). https://doi.org/10.1038/s41433-019-0547-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0547-3
This article is cited by
-
Factors affecting anatomical and visual outcomes in Terson syndrome managed by surgery or observation
Eye (2024)
-
An explanation for Terson syndrome at last: the glymphatic reflux theory
Journal of Neurology (2022)
-
Clinical observations and considerations in the treatment of Terson syndrome using 23G vitrectomy
International Ophthalmology (2020)