Abstract
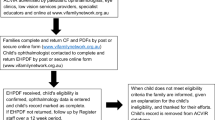
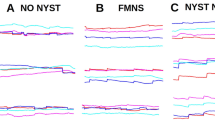
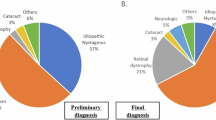
Nystagmus is an eye movement disorder characterised by abnormal, involuntary rhythmic oscillations of one or both eyes, initiated by a slow phase. It is not uncommon in the UK and regularly seen in paediatric ophthalmology and adult general/strabismus clinics. In some cases, it occurs in isolation, and in others, it occurs as part of a multisystem disorder, severe visual impairment or neurological disorder. Similarly, in some cases, visual acuity can be normal and in others can be severely degraded. Furthermore, the impact on vision goes well beyond static acuity alone, is rarely measured and may vary on a minute-to-minute, day-to-day or month-to-month basis. For these reasons, management of children with nystagmus in the UK is varied, and patients report hugely different experiences and investigations. In this review, we hope to shine a light on the current management of children with nystagmus across five specialist centres in the UK in order to present, for the first time, a consensus on investigation and clinical management.
摘要
眼球震颤是一种眼球运动障碍以单眼或双眼异常的、不自主的节律性摆动为特征, 其发病缓慢。在英国的发病率不低, 通常就诊于小儿眼科和成人普通/斜视门诊。眼球震颤在某些情况下单发, 也可伴发多系统疾病、严重视力损害或神经系统疾病。同样, 在一些病例中, 患者视力正常, 另一些病例中, 患者视力严重下降。而且其对视力的影响远超过对静态视敏度的影响, 几乎检测不到, 而且可能在每分钟、每天或每月的基础上不断变化。基于以上原因, 在英国, 针对儿童眼球震颤的管理是多样的, 而且患者的症状与调查报告也有很大的差别。我们希望本文能从英国五个专科中心的眼球震颤儿童的现行的管理有所启发, 以便首次达成调查与临床管理共识。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
09 February 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41433-020-0797-0
References
Sarvananthan N, Surendran M, Roberts EO, Jain S, Thomas S, Shah N, et al. The prevalence of nystagmus: the Leicestershire nystagmus survey. Investig Ophthalmol Vis Sci. 2009;50:5201–6.
Gottlob I, Zubcov A, Catalano RA, Reinecke RD, Koller HP, Calhoun JH, et al. Signs distinguishing spasmus nutans (with and without central nervous system lesions) from infantile nystagmus. Ophthalmology. 1990;97:1166–75.
Leigh RJ, Zee DS. The neurology of eye movements. New York: Oxford University Press; 2006.
Casteels I, Harris CM, Shawkat F, Taylor D. Nystagmus in infancy. Br J Ophthalmol. 1992;76:434–7.
Osborne D, Theodorou M, Lee H, Ranger M, Hedley-Lewis M, Shawkat F, et al. Supranuclear eye movements and nystagmus in children: a review of the literature and guide to clinical examination, interpretation of findings and age-appropriate norms. Eye. 2019;33:261–73.
Brodsky MC, Fray KJ. The prevalence of strabismus in congenital nystagmus: the influence of anterior visual pathway disease. JAAPOS. 1997;1:16–9.
Dell'Osso LF. Congenital, latent and manifest latent nystagmus-similarities, differences and relation to strabismus. Jpn J Ophthalmol. 1985;29:351–68.
Abadi RV, Dickinson CM. Waveform characteristics in congenital nystagmus. Doc Ophthalmol. 1986;64:153–67.
Dell'Osso LF, Flynn JT, Daroff RB. Hereditary congenital nystagmus. An intrafamilial study. Arch Ophthalmol. 1974;92:366–74.
Brodsky MC, Fray KJ. Positive angle kappa: a sign of albinism in patients with congenital nystagmus. Am J Ophthalmol. 2004;137:625–9.
Hove MN, Kilic-Biyik KZ, Trotter A, Grønskov K, Sander B, Larsen M, et al. Clinical characteristics, mutation spectrum, and prevalence of Åland eye disease/incomplete congenital stationary night blindness in Denmark. Investig Ophthalmol Vis Sci. 2016;57:6861–9.
Benouaich X, Mahieu L, Matonti F, Soler V. Persistence of foveal capillary plexi in a case of fovea plana evident on OCT angiography. J Fr Ophtalmol. 2017;40:4–7.
Bowl W, Andrassi-Darida M, Holve K, Schweinfurth S, Knobloch R, Lorenz B. [Handheld optical coherence tomography in paediatric ophthalmology: experience of the Department of Ophthalmology in Giessen]. Klin Monbl Augenheilkd. 2016;233:1142–8.
Sánchez-Vicente JL, Contreras-Díaz M, Llerena-Manzorro L, Rueda T, López-Herrero F, Molina-Socola FE, et al. Foveal hypoplasia: diagnosis using optical coherence tomography angiography. Retin Cases Brief Rep. 2018;12:122–6.
Langlo CS, Patterson EJ, Higgins BP, Summerfelt P, Razeen MM, Erker LR, et al. Residual foveal cone structure in CNGB3-associated achromatopsia. Investig Ophthalmol Vis Sci. 2016;57:3984–95.
Lee H, Proudlock FA, Gottlob I. Pediatric optical coherence tomography in clinical practice-recent progress. Investig Ophthalmol Vis Sci. 2016;57:69–79.
Kumar V, Molla K, Chandra P, Kumar A. Dome-shaped macula in oculocutaneous albinism. BMJ Case Rep. 2016;2016. https://doi.org/10.1136/bcr-2016-215368.
Al Oreany AA, Al Hadlaq A, Schatz P. Congenital stationary night blindness with hypoplastic discs, negative electroretinogram and thinning of the inner nuclear layer. Graefes Arch Clin Exp Ophthalmol. 2016;254:1951–6.
Bouraoui R, Bouladi M, Nefaa F, Limaiem R, El Matri L. Role of SD-OCT in the diagnosis and prognosis of macular hypoplasia in nystagmus patients. J Fr Ophtalmol. 2016;39:272–6.
Matalia J, Rajput VK, Chillal GJ, Shetty BK. Upbeat nystagmus in a 3.5-year-old boy. J Aapos. 2016;20:88–90.
Hull S, Arno G, Holder GE, Plagnol V, Gomez K, Liesner R, et al. The ophthalmic presentation of Hermansky-Pudlak syndrome 6. Br J Ophthalmol. 2016;100:1521–4.
Mallipatna A, Vinekar A, Jayadev C, Dabir S, Sivakumar M, Krishnan N, et al. The use of handheld spectral domain optical coherence tomography in pediatric ophthalmology practice: our experience of 975 infants and children. Indian J Ophthalmol. 2015;63:586–93.
Mohammad S, Gottlob I, Sheth V, Pilat A, Lee H, Pollheimer E, et al. Characterization of Abnormal optic nerve head morphology in albinism using optical coherence tomography. Investig Ophthalmol Vis Sci. 2015;56:4611–8.
Han R, Wang X, Wang D, Wang L, Yuan Z, Ying M, et al. GPR143 gene mutations in five Chinese families with X-linked congenital nystagmus. Sci Rep. 2015;5:12031.
McCafferty BK, Wilk MA, McAllister JT, Stepien KE, Dubis AM, Brilliant MH, et al. Clinical insights into foveal morphology in albinism. J Pediatr Ophthalmol Strabismus. 2015;52:167–72.
Putnam CM, Bland PJ. Macular pigment optical density spatial distribution measured in a subject with oculocutaneous albinism. J Optom. 2014;7:241–5.
Cornish KS, Reddy AR, McBain VA. Concentric macular rings sign in patients with foveal hypoplasia. JAMA Ophthalmol. 2014;132:1084–8.
Cai CY, Zhu H, Shi W, Su L, Shi O, Cai CQ, et al. A novel splicing site mutation of the GPR143 gene in a Chinese X-linked ocular albinism pedigree. Genet Mol Res. 2013;12:5673–9.
Thomas S, Thomas MG, Andrews C, Chan WM, Proudlock FA, McLean RJ, et al. Autosomal-dominant nystagmus, foveal hypoplasia and presenile cataract associated with a novel PAX6 mutation. Eur J Hum Genet. 2014;22:344–9.
Lee H, Purohit R, Sheth V, McLean RJ, Kohl S, Leroy BP, et al. Retinal development in infants and young children with achromatopsia. Ophthalmology. 2015;122:2145–7.
Lee H, Sheth V, Bibi M, Maconachie G, Patel A, McLean RJ, et al. Potential of handheld optical coherence tomography to determine cause of infantile nystagmus in children by using foveal morphology. Ophthalmology. 2013;120:2714–24.
Lee H, Proudlock F, Gottlob I. Is handheld optical coherence tomography reliable in infants and young children with and without nystagmus? Investig Ophthalmol Vis Sci. 2013;54:8152–9.
Thomas MG, Kumar A, Mohammad S, Proudlock FA, Engle EC, Andrews C, et al. Structural grading of foveal hypoplasia using spectral-domain optical coherence tomography a predictor of visual acuity? Ophthalmology. 2011;118:1653–60.
Clark R, Blundell J, Dunn MJ, Erichsen JT, Giardini ME, Gottlob I, et al. The potential and value of objective eye tracking in the ophthalmology clinic. Eye. 2019;33:1200–2.
Dell'Osso L, Gauthier G, Liberman G, Stark L. Eye movement recordings as a diagnostic tool in a case of congenital nystagmus. Am J Optom Arch Am Acad Optom. 1972;49:3–13.
Ramat S, Leigh RJ, Zee DS, Shaikh AG, Optican LM. Applying saccade models to account for oscillations. Prog Brain Res. 2008;171:123–30.
Kriss A, Russell-Eggitt I. Electrophysiological assessment of visual pathway function in infants. Eye. 1992;6:145–53.
McCulloch DL, Marmor MF, Brigell MG, Hamilton R, Holder GE, Tzekov R, et al. Erratum to: ISCEV standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol. 2015;131:81–3.
Shawkat FS, Kriss A, Thompson D, Russell-Eggitt I, Taylor D, Harris C. Vertical or asymmetric nystagmus need not imply neurological disease. Br J Ophthalmol. 2000;84:175–80.
O'Gorman L, Norman CS, Michaels L, Newall T, Crosby AH, Mattocks C, et al. A small gene sequencing panel realises a high diagnostic rate in patients with congenital nystagmus following basic phenotyping. Sci Rep. 2019;9:13229.
Thomas MG, Maconachie G, Sheth V, McLean RJ, Gottlob I. Development and clinical utility of a novel diagnostic nystagmus gene panel using targeted next-generation sequencing. Eur J Hum Genet. 2017;25:725–34.
Norman CS, O'Gorman L, Gibson J, Pengelly RJ, Baralle D, Ratnayaka JA, et al. Identification of a functionally significant tri-allelic genotype in the Tyrosinase gene (TYR) causing hypomorphic oculocutaneous albinism (OCA1B). Sci Rep. 2017;7:4415.
Jayaramachandran P, Proudlock FA, Odedra N, Gottlob I, McLean RJ. A randomized controlled trial comparing soft contact lens and rigid gas-permeable lens wearing in infantile nystagmus. Ophthalmology. 2014;121:1827–36.
Theodorou M, Quartilho A, Xing W, Bunce C, Rubin G, Adams G, et al. Soft contact lenses to optimize vision in adults with idiopathic infantile nystagmus: a pilot parallel randomized controlled trial. Strabismus. 2018;26:11–21.
Mehta AR, Kennard C. The pharmacological treatment of acquired nystagmus. Pr Neurol. 2012;12:147–53.
Kalla R, Strupp M. Aminopyridines and acetyl-DL-leucine: new therapies in cerebellar disorders. Curr Neuropharmacol. 2019;17:7–13.
McLean RJ, Gottlob I. The pharmacological treatment of nystagmus: a review. Expert Opin Pharmacother. 2009;10:1805–16.
McLean R, Proudlock F, Thomas S, Degg C, Gottlob I. Congenital nystagmus: randomized, controlled, double-masked trial of memantine/gabapentin. Ann Neurol. 2007;61:130–8.
ANDERSON JR. Causes and treatment of congenital eccentric nystagmus. Br J Ophthalmol. 1953;37:267–81.
Goto N. A study opt nystagmus electro-oculogram. 1954;58:851–65.
Kestenbaum A. Novell operation du nystagmus. 1954;2:851–65.
Parks MM. Symposium: nystagmus. Congenital nystagmus surgery. Am Orthopt J. 1973;23:35–9.
Nelson LB, Ervin-Mulvey LD, Calhoun JH, Harley RD, Keisler MS. Surgical management for abnormal head position in nystagmus: the augmented modified Kestenbaum procedure. Br J Ophthalmol. 1984;68:796–800.
Calhoun JH, Harley RD. Surgery for abnormal head position in congenital nystagmus. Trans Am Ophthalmol Soc. 1973;71:70–83. Discussion 4–7.
Kang NY, Isenberg SJ. Kestenbaum procedure with posterior fixation suture for anomalous head posture in infantile nystagmus. Graefes Arch Clin Exp Ophthalmol. 2009;247:981–7.
Lee IS, Lee JB, Kim HS, Lew H, Han SH. Modified Kestenbaum surgery for correction of abnormal head posture in infantile nystagmus: outcome in 63 patients with graded augmentaton. Binocul Vis Strabismus Q. 2000;15:53–8.
Taylor JN, Jesse K. Surgical management of congenital nystagmus. Aust N Z J Ophthalmol. 1987;15:25–34.
Scott WE, Kraft SP. Surgical treatment of compensatory head position in congenital nystagmus. J Pediatr Ophthalmol Strabismus. 1984;21:85–95.
Schild AM, Thoenes J, Fricke J, Neugebauer A. Kestenbaum procedure with combined muscle resection and tucking for nystagmus-related head turn. Graefes Arch Clin Exp Ophthalmol. 2013;251:2803–9.
Kommerell G. Surgical management of altered head posture in patients with congenital nystagmus (author's transl). Klinische Monatsblatter fur Augenheilkd. 1974;164:172–91.
Pratt-Johnson JA. Results of surgery to modify the null-zone position in congenital nystagmus. Can J Ophthalmol. 1991;26:219–23.
Sandall GS. Surgical treatment of congenital nystagmus in patients with singular binocular vision. Ann Ophthalmol. 1976;8:227–38.
Kraft SP, O'Donoghue EP, Roarty JD. Improvement of compensatory head postures after strabismus surgery. Ophthalmology. 1992;99:1301–8.
Chang YH, Chang JH, Han SH, Lee JB. Outcome study of two standard and graduated augmented modified Kestenbaum surgery protocols for abnormal head postures in infantile nystagmus. Binocul Vis strabismus Q. 2007;22:235–41.
Biglan AW, Hiles DA, Ying-Fen Z, Kortvelesy JS, Pettapiece MC
Spielmann A. Clinical rationale for manifest congenital nystagmus surgery. J Aapos. 2000;4:67–74.
Kumar A, Shetty S, Vijayalakshmi P, Hertle RW. Improvement in visual acuity following surgery for correction of head posture in infantile nystagmus syndrome. J Pediatr Ophthalmol Strabismus. 2011;48:341–6.
ElKamshoushy A, Shawky D, ElMassry A, ElBaha S, Abdel Wahab MM, Sprunger D. Improved visual acuity and recognition time in nystagmus patients following four-muscle recession or Kestenbaum-Anderson procedures. J Aapos. 2012;16:36–40.
Biglan AW, Hiles DA, Ying-Fen Z, Kortvelesy JS, Pettapiece MC. Results after surgery for null point nystagmus with abnormal head position. Am Orthop J. 1989;39:134–42.
Lee J. Surgical management of nystagmus. J R Soc Med. 2002;95:238–41.
Kushner BJ. The usefulness of the cervical range of motion device in the ocular motility examination. Arch Ophthalmol. 2000;118:946–50.
Mitchell PR, Wheeler MB, Parks MM. Kestenbaum surgical procedure for torticollis secondary to congenital nystagmus. J Pediatr Ophthalmol Strabismus. 1987;24:87–93.
Tyedmers M, Roper-Hall G. The harms tangent screen test. Am Orthopt J. 2006;56:175–9.
Harms H. Ueber die Untersuchung der Augenmuskellahmungen. Graefes Arch Ophthalmol. 1941;144:129.
Pourahmadi MR, Bagheri R, Taghipour M, Takamjani IE, Sarrafzadeh J, Mohseni-Bandpei MA. A new iPhone application for measuring active craniocervical range of motion in patients with non-specific neck pain: a reliability and validity study. Spine J. 2018;18:447–57.
Dell'Osso LF, Flynn JT. Congenital nystagmus surgery. A quantitative evaluation of the effects. Arch Ophthalmol. 1979;97:462–9.
von Noorden GK, Avilla C, Sidikaro Y, LaRoche R. Latent nystagmus and strabismic amblyopia. Am J Ophthalmol. 1987;103:87–9.
Thurtell MJ, Leigh RJ. Therapy for nystagmus. J Neuroophthalmol. 2010;30:361–71.
Bjerre A, Arblaster GE, Nye A, Griffiths HJ. The provision of patient information about nystagmus. Br Ir Orthopt J. 2018;14:25–9.
McLean RJ, Windridge KC, Gottlob I. Living with nystagmus: a qualitative study. Br J Ophthalmol. 2012;96:981–6.
Gräf M, Droutsas K, Kaufmann H. Congenital nystagmus: indication, results and dosage of Kestenbaum surgery in 34 patients. Klinische Monatsblatter fur Augenheilkd. 2000;217:334–9.
Wang P, Lou L, Song L. Design and efficacy of surgery for horizontal idiopathic nystagmus with abnormal head posture and strabismus. J Huazhong Univ Sci Technol Med Sci. 2011;31:678–81.
von Noorden GK, Sprunger DT. Large rectus muscle recessions for the treatment of congenital nystagmus. Arch Ophthalmol. 1991;109:221–4.
Arruga A. Posterior fixation of recti in nystagmus with retinal detachment. Mod Probl Ophthalmol. 1975;15:304–6.
Mühlendyck H, Linnen HJ. The operative treatment of nystagmus-caused variable squint angles with Cüppers "Fadenoperation" (author's transl). Klinische Monatsblatter fur Augenheilkd. 1975;167:273–90.
Nystagmus UK Eye research group (NUKE)
G. E. Arblaster10, A . Bjerre10, M. J. Dunn3, J. T. Erichsen3, I . Gottlob4, H. J. Griffiths5, C. Harris6, H. Lee1,2, L. McIlreavy3, J. Owen6, J. Sanders7, J. E. Self1,2, F. Shawkat1, M. Theodorou8,9, J. P. Whittle10, D. Osborne1,2, M. Ranger1,2, C. Norman2, K. MacKenzie8, N. Venturi8, TailorV8, Frank Proudlock4, Rebecca McLean4, Mervyn Thomas4, Viral Sheth4, Perry Carter1
Author information
Authors and Affiliations
Author notes
Members of the Nystagmus UK Eye research group (NUKE) are listed at the end of the paper.
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Self, J.E., Dunn, M.J., Erichsen, J.T. et al. Management of nystagmus in children: a review of the literature and current practice in UK specialist services. Eye 34, 1515–1534 (2020). https://doi.org/10.1038/s41433-019-0741-3
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0741-3
This article is cited by
-
Pharmacovigilance study of drug-induced eye movement disorder based on FDA adverse event reports from 2004 to 2024
Scientific Reports (2025)
-
Nystagmus in infancy: causes, characteristics and main tools for diagnosis
Eye (2025)
-
Impaired vision in children prenatally exposed to methadone: an observational cohort study
Eye (2024)
-
Crossed VEP asymmetry in a patient with AHR-linked infantile nystagmus and foveal hypoplasia
Documenta Ophthalmologica (2024)
-
Analysis of Fibroblast Growth Factor 14 (FGF14) structural variants reveals the genetic basis of the early onset nystagmus locus NYS4 and variable ataxia
European Journal of Human Genetics (2023)