Abstract
Objective
The objective of this study is to characterise the natural history of conjunctival naevi in a paediatric and adolescent population.
Methods
All children and adolescents referred to Moorfields Ocular Oncology Service for evaluation between January 2015 and 2020 were included. Exclusion criteria included age >20 years old and lack of anterior segment photographs. A total of 77 patients were included with a mean age of 12 years (standard deviation: 3.9; range, 4–20). The main outcome measures were: number of conjunctival naevi that grew, changed in pigmentation, required excisional biopsy, or were histologically malignant. If there was growth, the percentage increase in size was measured.
Results
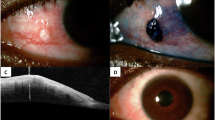
At their first visit, 13% of patients (10/77) were discharged to local follow-up and 10% (8/77) proceeded to excisional biopsy, four further patients underwent excisional biopsy after a period of follow-up. On histopathological assessment, 92% (11/12) of lesions were benign conjunctival naevi. One patient, who had suspicious clinical features at presentation, had conjunctival melanoma. Fifty-nine patients were followed over a median of 1.1 years (interquartile range: 1.54; range, 3 months to 4 years). Eight per cent (5/59) of conjunctival naevi enlarged in diameter by a mean percentage increase in size of 2%, whereas 5% (3/59) showed increased pigmentation and 8.5% (5/59) showed decreased pigmentation.
Conclusions
Growth of conjunctival naevi in children is infrequent (8%) and the large majority of those excised are benign. Because of a lack of evidence, these patients are often followed for years in ophthalmic practice. This series demonstrates that prolonged follow-up may not be necessary.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Shields CL, Sioufi K, Alset AE. Clinical features differentiating benign from malignant conjunctival tumors in children. JAMA Ophthalmol. 2017;135:215–24.
Shields CL, Fasiuddin AF, Mashayekhi A, Shields JA. Conjunctival nevi: clinical features and natural course in 410 consecutive patients. Arch Ophthalmol. 2004;122:167–75.
Levecq L, De Potter P, Jamart J. Conjunctival nevi clinical features and therapeutic outcomes. Ophthalmology. 2010;117:35–40.
Shields CL, Shields JA, Gündüz K, Cater J, Mercado GV, Gross N, et al. Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis and death in 150 consecutive patients. Arch Ophthalmol. 2000;118:1497–507.
McDonnell JM, Carpenter JD, Jacobs P, Wan WL, Gilmore JE. Conjunctival melanocytic lesions in children. Ophthalmology. 1989;96:986–93.
Gerner N, Nørregaard JC, Jensen OA, Prause JU. Conjunctival naevi in Denmark 1960-1980. A 21-year follow-up study. Acta Ophthalmol Scand. 1996;74:334–7.
Zamir E, Mechoulam H, Micera A, Levi-Schaffer F, Pe’er J. Inflamed juvenile con-junctival nevus: clinicopathological characterization. Br J Ophthalmol. 2002;86:28–30.
Shields CL, Belinsky I, Romanelli-Gobbi M, Guzman J, Mazzuca Jr D, Green WR, et al. Anterior segment optical coherence tomography of conjunctival nevus. Ophthalmology. 2011;118:915–9.
Funding
The research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Negretti, G.S., Roelofs, K.A., Damato, B. et al. The natural history of conjunctival naevi in children and adolescents. Eye 35, 2579–2584 (2021). https://doi.org/10.1038/s41433-020-01273-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-01273-4
This article is cited by
-
Bindehauttumoren bei Kindern
Die Ophthalmologie (2023)