Abstract
Background/objectives
Abnormal retinal neovascularization caused by ischemic retinal vein occlusion (RVO) is a frequent cause of visually significant vitreous hemorrhage. The early detection of new vessels may be challenging and often requires the use of invasive tests such as fundus fluorescein angiography (FA). We demonstrate the use of wide-field optical coherence tomography angiography (WF-OCTA) in the detection and characterization of neovascularization secondary to ischemic RVO.
Subjects/methods
We conducted a retrospective observational case series of patients diagnosed with ischemic RVO between August 2018 and March 2019, who underwent WF-SS-OCTA imaging (PLEX Elite 9000, Carl Zeiss Meditec). We performed real-life montage imaging, covering the involved area and compared the findings of WF-SS-OCTA to standard clinical examination and when available, ultrawide-field fluorescein angiography (UWF-FA, Optos 200TX).
Results
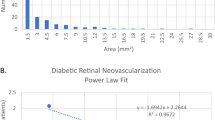
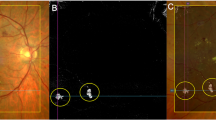
In the included 39 eyes with ischemic RVO, neovascularization elsewhere (NVE) was encountered in 16 of 39 eyes (41%) on WF-OCTA and were characterized as sea-fan type vessels and nodular type vessels, based on their appearance and localization. NVE was identified in 4/39 eyes on standard clinical examination, equating to a detection rate of 10.3%. All were of a sea-fan morphology. In one case, NVE found on WF-OCTA was not observed on UWF-FA, which was a nodular type. Neovascularization of the disc (NVD) was detected in one eye.
Conclusions
WF-OCTA may become a useful noninvasive tool in the detection of neovascularization in patients with ischemic RVO. Furthermore, the characterization of different morphologies of neovascularization detected by WF-OCTA could be of clinical relevance
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology. 2010;117:313–9.e1.
Hayreh SS, Klugman MR, Beri M, Kimura AE, Podhajsky P. Differentiation of ischemic from non-ischemic central retinal vein occlusion during the early acute phase. Graefe’s Arch Clin Exp Ophthalmol. 1990;228:201–17. https://doi.org/10.1007/bf00920022.
Keane PA, Sadda SR. Retinal imaging in the twenty-first century. Ophthalmology. 2014;121:2489–2500. https://doi.org/10.1016/j.ophtha.2014.07.054.
Gao SS, Jia Y, Zhang M, Su JP, Liu G, Hwang TS. et al. Optical coherence tomography angiography. Investigative Opthalmol Vis Sci. 2016;57:OCT27–36. https://doi.org/10.1167/iovs.15-19043.
Cardoso JN, Keane PA, Sim DA, Bradley P, Agrawal R, Addison PK. et al. Systematic evaluation of optical coherence tomography angiography in retinal vein occlusion. Am J Ophthalmol. 2016;163:93–107.e6. https://doi.org/10.1016/j.ajo.2015.11.025.
Shiraki A, Sakimoto S, Tsuboi K, Wakabayashi T, Hara C, Fukushima Y, et al. Evaluation of retinal nonperfusion in branch retinal vein occlusion using wide-field optical coherence tomography angiography. Acta Ophthalmol. 2019;97:e913–8.
Hirano T, Kakihara S, Toriyama Y, Nittala MG, Murata T, Sadda S. Wide-field en face swept-source optical coherence tomography angiography using extended field imaging in diabetic retinopathy. Br J Ophthalmol. 2018;102:1199–203.
Sawada O, Ichiyama Y, Obata S, Ito Y, Kakinoki M, Sawada T, et al. Comparison between wide-angle OCT angiography and ultra-wide field fluorescein angiography for detecting non-perfusion areas and retinal neovascularization in eyes with diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2018;256:1275–80.
Yannuzzi LA, Rohrer KT, Tindel LJ, Sobel RS, Costanza MA, Shields W. et al. Fluorescein angiography complication survey. Ophthalmology. 1986;93:611–7. https://doi.org/10.1016/s0161-6420(86)33697-2.
The Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous hemorrhage in branch vein occlusion. Arch Ophthalmol. 1986; 104:34. https://doi.org/10.1001/archopht.1986.01050130044017.
Laatikainen L, Kohner EM, Khoury D, Blach RK. Panretinal photocoagulation in central retinal vein occlusion: a randomised controlled clinical study. Br J Ophthalmol. 1977;61:741–53. https://doi.org/10.1136/bjo.61.12.741.
Arsene S, Vierron E, Le Lez ML, Herault B, Gruel Y, Pisella PJ, et al. Conversion from nonischemic to ischemic retinal vein occlusion: prediction by venous velocity on color Doppler imaging. Eur J Ophthalmol. 2009;19:1009–16.
Minturn J, Brown GC. Progression of nonischemic central retinal vein obstruction to the ischemic variant. Ophthalmology. 1986;93:1158–62.
Royal College of Ophthalmology. RCOphth Retinal Vein Occlusion Guidelines. 2015. https://www.rcophth.ac.uk/wp-content/uploads/2015/07/Retinal-Vein-Occlusion-RVO-Guidelines-July-2015.pdf. Accessed April 2019.
The Central Vein Occlusion Study Group. A randomized clinical trial of early panretinal photocoagulation for ischermic central vein occlusion. Ophthalmology. 1995;102:1434–44. https://doi.org/10.1016/s0161-6420(95)30848-2.
Schwartz R, Khalid H, Sivaprasad S, Nicholson L, Anikina E, Sullivan P, et al. Objective Evaluation of Proliferative Diabetic Retinopathy Using OCT. Ophthalmol Retina. 2019. https://doi.org/10.1016/j.oret.2019.09.004.
Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ. 1992;304:1491–4.
de Carlo TE, Bonini Filho MA, Baumal CR, Reichel E, Rogers A, Witkin AJ, et al. Evaluation of preretinal neovascularization in proliferative diabetic retinopathy using optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retina 2016;47:115–9.
Jia Y, Bailey ST, Hwang TS, McClintic SM, Gao SS, Pennesi ME, et al. Quantitative optical coherence tomography angiography of vascular abnormalities in the living human eye. Proc Natl Acad Sci USA. 2015;112:E2395–402.
Finkelstein D, Clarkson J, Diddie K, Hillis A, Kimball A, Orth D, et al. Branch vein occlusion. Retinal neovascularization outside the involved segment. Ophthalmology. 1982;89:1357–61.
Shilling JS, Kohner EM. New vessel formation in retinal branch vein occlusion. Br J Ophthalmol. 1976;60:810–5. https://doi.org/10.1136/bjo.60.12.810.
Hayreh SS, Zimmerman MB. Fundus changes in branch retinal vein occlusion. Retina. 2015;35:1016–27.
Magargal LE, Brown GC, Augsburger JJ, Parrish RK 2nd. Neovascular glaucoma following central retinal vein obstruction. Ophthalmology. 1981;88:1095–101.
Zegarra H, Gutman FA, Conforto J. The natural course of central retinal vein occlusion. Ophthalmology. 1979;86:1931–9. https://doi.org/10.1016/s0161-6420(79)35327-1.
Hayreh SS, Rubenstein L, Podhajsky P. Argon laser scatter photocoagulation in treatment of branch retinal vein occlusion. Ophthalmologica. 1993;206:1–14. https://doi.org/10.1159/000310354.
Hayreh SS, Bridget Zimmerman M, Podhajsky P. Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol.1994;117:429–41. https://doi.org/10.1016/s0002-9394(14)70001-7.
Chan CK, Ip MS, VanVeldhuisen PC, Oden NL, Scott IU, Tolentino MJ, et al. SCORE study report #11. Ophthalmology. 2011. https://doi.org/10.1016/j.ophtha.2010.11.020.
Mendis KR, Balaratnasingam C, Yu P, Barry CJ, McAllister IL, Cringle SJ, et al. Correlation of histologic and clinical images to determine the diagnostic value of fluorescein angiography for studying retinal capillary detail. Invest Ophthalmol Vis Sci. 2010;51:5864–9.
Spaide RF, Klancnik JM, Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:45. https://doi.org/10.1001/jamaophthalmol.2014.3616.
Nicholson L, Vazquez-Alfageme C, Patrao NV, Triantafyllopolou I, Bainbridge JW, Hykin PG, et al. Retinal nonperfusion in the posterior pole is associated with increased risk of neovascularization in central retinal vein occlusion. Am J Ophthalmol. 2017;182:118–25.
Acknowledgements
Presented at: the 19th EURETINA 2019 Congress, Paris, France, September 5-8, 2019. Acknowledgments to the NIHR Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, London, UK, for supporting the research.
Funding
HK is supported by a scholarship from Egyptian mission sector, Ministry of Higher Education, Egypt. RR has received speaker fees from Carl Zeiss Meditec AG. PAK has received speaker fees from Heidelberg Engineering, Topcon, Carl Zeiss Meditec AG, Haag-Streit, Allergan, Novartis, and Bayer. He has served on advisory boards for Novartis and Bayer and has been an external consultant for DeepMind and Optos. PAK is supported by a United Kingdom (UK) National Institute for Health Research (NIHR) Clinician Scientist Award (NIHR-CS--2014-12-023). Other authors have no financial disclosures. The sponsor had no rule in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huemer, J., Khalid, H., Wagner, S.K. et al. Phenotyping of retinal neovascularization in ischemic retinal vein occlusion using wide field OCT angiography. Eye 35, 2812–2819 (2021). https://doi.org/10.1038/s41433-020-01317-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-01317-9
This article is cited by
-
Enhanced therapeutic effect of PEDF-loaded mesenchymal stem cell-derived small extracellular vesicles against oxygen-induced retinopathy through increased stability and penetrability of PEDF
Journal of Nanobiotechnology (2023)
-
Deep-learning-based AI for evaluating estimated nonperfusion areas requiring further examination in ultra-widefield fundus images
Scientific Reports (2022)