Abstract
Purpose
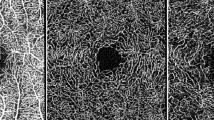
In this pilot study we reported variation of superficial (SCP) and deep (DCP) capillary plexuses flow in macular and near/mid periphery regions in healthy subjects using widefield swept source-optical coherence tomography angiography (SS-OCTA).
Methods
In this prospective, cross-sectional study, enroled subjects were imaged with an SS-OCTA system (PLEX Elite 9000, Carl Zeiss Meditec Inc., Dublin, CA, USA). OCTA scans were taken in primary and extremes of gaze and a montage was automatically created. Quantitative analysis was performed in the macular and peripheral regions. In addition, SCP and DCP variables were further investigated in distinct fields within these three different regions.
Results
Fifty-five young healthy subjects (55 eyes) were enroled. The retinal periphery displayed a higher SCP perfusion density (39.6 ± 1.7% and 40.7 ± 1.4%, P < 0.0001) and SCP vessel diameter index (3.5 ± 0.2 and 3.6 ± 0.2, P < 0.0001), in comparison with the macular region. At the DCP level, the retinal periphery was characterized by a lower perfusion density (41.6 ± 3.7% and 37.9 ± 2.9%, P < 0.0001) and vessel length density (14.6 ± 6.0% and 9.9 ± 2.6%, P < 0.0001). In the analysis investigating the DCP in the retinal periphery, the temporal sector was characterized by a reduction in perfusion density, vessel length density, and vessel diameter index. In univariate analysis, the retinal thickness was found to have a significant direct relationship with DCP perfusion density (P < 0.0001), but not with SCP perfusion density (P = 0.712).
Conclusions
We report quantitative mapping of the SCP and DCP in healthy individuals. The DCP perfusion appears to have a wide topographical variation, which is strictly dependent on the retinal thickness.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Savastano MC, Lumbroso B, Rispoli M. In vivo characterization of retinal vascularization morphology using optical coherence tomography angiography. Retina. 2015. https://doi.org/10.1097/IAE.0000000000000635.
Park JJ, Soetikno BT, Fawzi AA. Characterization of the middle capillary plexus using optical coherence tomography angiography in healthy and diabetic eyes. Retina. 2016;36:2039–50. https://doi.org/10.1097/IAE.0000000000001077.
Yu D-Y, Yu PK, Cringle SJ, Kang MH, Su E-N. Functional and morphological characteristics of the retinal and choroidal vasculature. Prog Retin Eye Res. 2014;40:53–93. https://doi.org/10.1016/j.preteyeres.2014.02.001.
Borrelli E, Sadda SR, Uji A, Querques G. Pearls and pitfalls of optical coherence tomography angiography imaging: a review. Ophthalmol Ther. 2019. https://doi.org/10.1007/s40123-019-0178-6.
Nesper PL, Fawzi AA. Human parafoveal capillary vascular anatomy and connectivity revealed by optical coherence tomography angiography. Investig Ophthalmol Vis Sci. 2018. https://doi.org/10.1167/iovs.18-24710.
Spaide R, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. 2017. https://doi.org/10.1016/j.preteyeres.2017.11.003.
Liu G, Yang J, Wang J, et al. Extended axial imaging range, widefield swept source optical coherence tomography angiography. J Biophotonics. 2017;10:1464–72. https://doi.org/10.1002/jbio.201600325.
Sawada O, Ichiyama Y, Obata S, et al. Comparison between wide-angle OCT angiography and ultra-wide field fluorescein angiography for detecting non-perfusion areas and retinal neovascularization in eyes with diabetic retinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:1275–80. https://doi.org/10.1007/s00417-018-3992-y.
Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR. Impact of multiple en face image averaging on quantitative assessment from optical coherence tomography angiography images. Ophthalmology. 2017. https://doi.org/10.1016/j.ophtha.2017.02.006.
Borrelli E, Lonngi M, Balasubramanian S, et al. Macular microvascular networks in healthy pediatric subjects. Retina. 2018. https://doi.org/10.1097/IAE.0000000000002123.
Borrelli E, Balasubramanian S, Triolo G, Barboni P, Sadda SR, Sadun AA. Topographic macular microvascular changes and correlation with visual loss in chronic leber hereditary optic neuropathy. Am J Ophthalmol. 2018;192:217–28. https://doi.org/10.1016/j.ajo.2018.05.029.
Durbin MK, An L, Shemonski ND. et al. Quantification of retinal microvascular density in optical coherence tomographic angiography images in diabetic retinopathy. JAMA Ophthalmol. 2017;135:370.
Forrester JV, Dick AD, McMenamin PG, Roberts F, Pearlman E. The eye: basic sciences in practice. Elsevier. 2008. p. 568. https://doi.org/10.1038/nrg1202.J.
Toto L, Borrelli E, Di Antonio L, Carpineto P, Mastropasqua R. Retinal vascular plexuses’ changes in dry age-related by means of optical coherence. Retina. https://doi.org/10.1097/IAE.0000000000000962.
Iafe NA, Phasukkijwatana N, Chen X, Sarraf D. Retinal capillary density and foveal avascular zone area are age-dependent: quantitative analysis using optical coherence tomography angiography. Investig Opthalmology Vis Sci. 2016;57:5780. https://doi.org/10.1167/iovs.16-20045.
Al-Sheikh M, Phasukkijwatana N, Dolz-Marco R, et al. Quantitative OCT angiography of the retinal microvasculature and the choriocapillaris in myopic eyes. Investig Ophthalmol Vis Sci. 2017;58:2063–9. https://doi.org/10.1167/iovs.16-21289.
Schachat AP, Sadda SR, Hinton DR, Wilkinson CP, Wiedemann P, editors. Ryan’s. Retina. 6th ed. New York: Elsevier; 2018.
Jia Y, Simonett JM, Wang J, et al. Wide-field OCT angiography investigation of the relationship between radial peripapillary capillary plexus density and nerve fiber layer thickness. Investig Ophthalmol Vis Sci. 2017. https://doi.org/10.1167/iovs.17-22593.
Provis JM, Penfold PL, Cornish EE, Sandercoe TM, Madigan MC. Anatomy and development of the macula: specialisation and the vulnerability to macular degeneration. Clin Exp Optom. 2005;88:269–81. http://www.ncbi.nlm.nih.gov/pubmed/16255686.
Yu DY, Cringle SJ, Su EN. Intraretinal oxygen distribution in the monkey retina and the response to systemic hyperoxia. Investig Ophthalmol Vis Sci. 2005. https://doi.org/10.1167/iovs.05-0694.
Yu DY, Cringle SJ, Yu PK, Su EN. Intraretinal oxygen distribution and consumption during retinal artery occlusion and graded hyperoxic ventilation in the rat. Investig Ophthalmol Vis Sci. 2007. https://doi.org/10.1167/iovs.06-1197.
Cringle SJ, Yu DY, Yu PK, Su EN. Intraretinal oxygen consumption in the rat in vivo. Investig Ophthalmol Vis Sci. 2002.
Yu DY, Cringle SJ, Alder V, Su EN. Intraretinal oxygen distribution in the rat with graded systemic hyperoxia and hypercapnia. Investig Ophthalmol Vis Sci. 1999.
Yu DY, Cringle SJ, Alder VA, Su EN. Intraretinal oxygen distribution in rats as a function of systemic blood pressure. Am J Physiol. 1994. https://doi.org/10.1152/ajpheart.1994.267.6.H2498.
Provis JM. Development of the primate retinal vasculature. Prog Retin Eye Res. 2001. https://doi.org/10.1016/S1350-9462(01)00012-X.
Borrelli E, Viggiano P, Evangelista F, Toto L, Mastropasqua R. Eyelashes artifact in ultra-widefield optical coherence tomography angiography. Ophthalmic Surg Lasers Imaging Retin. 2019.
Borrelli E, Uji A, Toto L, Viggiano P, Evangelista F, Mastropasqua R. In vivo mapping of the choriocapillaris in healthy eyes: a widefield swept source optical coherence tomography angiography study. Ophthalmol Retina. 2019;3:979–84. https://doi.org/10.1016/j.oret.2019.05.026.
Lei J, Durbin MK, Shi Y, et al. Repeatability and reproducibility of superficial macular retinal vessel density measurements using optical coherence tomography angiography en face images. JAMA Ophthalmol. 2017;135:1092–8. https://doi.org/10.1001/jamaophthalmol.2017.3431.
Al-Sheikh M, Tepelus TC, Nazikyan T, Sadda SVR. Repeatability of automated vessel density measurements using optical coherence tomography angiography. Br J Ophthalmol. 2017. https://doi.org/10.1136/bjophthalmol-2016-308764.
Author information
Authors and Affiliations
Contributions
Study concept and design: BE and MR; Acquisition, analysis, or interpretation of data: all authors. Drafting of the paper: BE and VP. Critical revision of the paper for important intellectual content: all authors. Statistical analysis: BE. Study supervision: BE and MR.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borrelli, E., Toto, L., Viggiano, P. et al. Widefield topographical analysis of the retinal perfusion and neuroretinal thickness in healthy eyes: a pilot study. Eye 34, 2264–2270 (2020). https://doi.org/10.1038/s41433-020-0804-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0804-5
This article is cited by
-
Hyperreflective choroidal foci may predict pachychoroid macular atrophy development in central serous chorioretinopathy
Eye (2026)
-
Photobiomodulation-induced choriocapillaris perfusion enhancement and outer retinal remodelling in intermediate age-related macular degeneration: a promising therapeutic approach with short-term results
Eye (2025)
-
Distinct Pathogenic Mechanisms of Neurodegeneration in Pachychoroid Pigment Epitheliopathy Versus Intermediate Age-Related Macular Degeneration
Ophthalmology and Therapy (2025)
-
Wide-field swept-source OCT angiography (23 × 20 mm) for detecting retinal neovascularization in eyes with proliferative diabetic retinopathy
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Wide-field swept-source OCTA in the assessment of retinal microvasculature in early-stage diabetic retinopathy
BMC Ophthalmology (2022)