Abstract
The eye is said to be the window into the brain. Alzheimer’s disease (AD) and glaucoma both being diseases of the elderly, have several epidemiological and histological overlaps in pathogenesis. Both these diseases are neurodegenerative conditions. Over the years, a consensus has developed that both may be two ends of a singular spectrum of diseases. Epidemiological studies have shown that more Alzheimer’s patients may be suffering from glaucoma than general healthy population. Retinal ganglion cell damage is a characteristic of both diseases, along with discovery of amyloid-β and tau protein deposition in the retina and aqueous humor of eye. The latter two proteins are known to be pathognomonic of AD. Other pathways such as the insulin receptor pathway also seem to be affected in both diseases similarly. In spite of these overlaps, there are few missing links which still need more evidence, namely, intraocular pressure mechanisms, cerebrospinal fluid pressure and trans-lamina cribrosa pressure gradients, vascular autoregulation factors, etc. Several factors point towards a common pathogenesis at some level for both diseases and prospective studies are necessary to study the natural course of both diseases.
摘要
眼睛是通往大脑的窗户。阿尔兹海默症 (Alzheimer’s disease, AD) 与青光眼均为老年性疾病, 在发病机制、流行病学以及组织病理学上有相同之处, 另外它们都是神经退行性疾病。多年来, 已经达成共识, 即这两者可能属于同一疾病谱。流行病学研究表明阿尔兹海默症患者青光眼的发病人数比一般健康人群多。视网膜神经节细胞损伤是这两种疾病的共同特征, 另外在视网膜和房水中发现β-淀粉样蛋白和tau蛋白沉积物, 后两种蛋白被认为是AD的病理学特征。其他通路如胰岛素受体通路在这两种疾病中均相似地受到影响。尽管两种疾病存在以上交叉, 但在球内压力机制、脑脊液压力和跨筛板压力梯度、血管自动调节因子等方面仍缺乏需要更多证据支持的关联。一些因素在一些程度上已经阐释了这两种疾病的共同发病机制, 前瞻性研究需要研究这两种疾病的自然病程.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Guerreiro R, Bras J. The age factor in Alzheimer’s disease. Genome Med. 2015;7:106.
Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J, et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology. 1992;99:1499–504.
Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, Javitt J. Racial variations in the prevalence of primary open-angle glaucoma. The Baltimore Eye Survey. J Am Med Assoc. 1991;266:369–74.
Bayer AU, Ferrari F, Erb C. High occurrence rate of glaucoma among patients with Alzheimer’s disease. Eur Neurol. 2002;47:165–8.
Tamura H, Kawakami H, Kanamoto T, Kato T, Yokoyama T, Sasaki K, et al. High frequency of open-angle glaucoma in Japanese patients with Alzheimer’s disease. J Neurol Sci. 2006;246:79–83.
Pelletier AA, Théorět MÈ, Boutin T, Kergoat MJ, Massoud F, Latour J, et al. Prevalence of glaucoma in hospitalized older adults with Alzheimer’s disease. Can J Neurol Sci. 2014;41:206–9.
Yochim BP, Mueller AE, Kane KD, Kahook MY. Prevalence of cognitive impairment, depression, and anxiety symptoms among older adults with glaucoma. J Glaucoma. 2012;21:250–4.
Kessing LV, Lopez AG, Andersen PK, Kessing SV. No increased risk of developing Alzheimer disease in patients with glaucoma. J Glaucoma. 2007;16:47–51.
Lin IC, Wang YH, Wang TJ, Wang IJ, Shen YD, Chi NF, et al. Glaucoma, Alzheimer’s disease, and Parkinson’s disease: an 8-year population-based follow-up study. PLoS ONE 2014;9:e108938.
Lai SW, Lin CL, Liao KF. Glaucoma may be a non-memory manifestation of Alzheimer’s disease in older people. Int Psychogeriatr. 2017;29:1–7.
Ou Y, Grossman DS, Lee PP, Sloan FA. Glaucoma, Alzheimer’s disease and other dementia: a longitudinal analysis. Ophthalmic Epidemiol. 2012;19:285–9.
Moon JY, Kim HJ, Park YH, Park TK, Park EC, Kim CY, et al. Association between Open-Angle Glaucoma and the Risks of Alzheimer’s and Parkinson’s Diseases in South Korea: A 10-year Nationwide Cohort Study. Sci Rep. 2018;24:11161.
Bach-Holm D, Kessing SV, Mogensen U, Forman JL, Andersen PK, Kessing LV. Normal tension glaucoma and Alzheimer disease: comorbidity? Acta Ophthalmol. 2012;90:683–5.
Krupin T. A clinical trial studying neuroprotection in low-pressure glaucoma. Eye. 2007;21:S51–4.
Chen Y-Y, Lai Y-J, Yen Y-F. Association between normal tension glaucoma and the risk of Alzheimer’s disease: a worldwide population-based cohort study in Taiwan. BMJ Open 2018;8:e022987.
McKinnon SJ. Glaucoma: ocular Alzheimer’s disease? Front Biosci. 2003;1:1140–56.
Osborne NN. Recent clinical findings with memantine should not mean that the idea of neuroprotection in glaucoma is abandoned. Acta Ophthalmol. 2009;87:450–4.
Weinreb RN, Liebman JM, Cioffi GA, Goldberg I, Brandt JD, Johnson CA, et al. Oral memantine for the treatment of glaucoma: design and results of 2 randomised, placebo-controlled, phase 3 studies. Ophthalmol. 2018. https://doi.org/10.1016/j.ophtha.2018.06.017.
Ordovas JM, Schaefer EJ. Genetic determinants of plasma lipid response to dietary intervention: the role of the APOA1/C3/A4 gene cluster and the APOE gene. Br J Nutr. 2000;83 Suppl 1 :S127–36.
Eichner JE, Dunn ST, Perveen G, Thompson DM, Stewart KE, Stroehla BC. Apolipoprotein E polymorphism and cardiovascular_disease: review. Am J Epidemiol. 2002;155:487–95.
Dallongeville J, Lussier-Cacan S, Davignon J. Modulation of plasma triglyceride levels by apoE phenotype: a meta-analysis. J Lipid Res. 1992;33:447–54.
Lahiri DK, Sambamurti K, Bennett DA. Apolipoprotein gene and its interaction with the environmentally driven risk factors: molecular, genetic and epidemiological studies of Alzheimer’s disease. Neurobiol Aging. 2004;25:651–60.
Amaratunga A, Abraham CR, Edwards RB, Sandell JH, Schreiber BM, Fine RE. Apolipoprotein E is synthesized in the retina by Muller glial cells, secreted into the vitreous, and rapidly transported into the optic nerve by retinal ganglion cells. J Biol Chem. 1996;271:5628–32.
Copin B, Brezin AP, Valtot F, Dascotte JC, Bechetoille A, Garchon HJ. Apolipoprotein E-promoter single-nucleotide polymorphisms affect the phenotype of primary open-angle glaucoma and demonstrate interaction with the myocilin gene. Am J Hum Genet. 2002;70:1575–81.
Liao R, Ye M, Xu X. An updated meta-analysis: apolipoprotein E genotypes and risk of primary open-angle glaucoma. Mol Vis. 2014;20:1025–36.
Bekris LM, Yu CE, Bird TD, Tsuang DW. Genetics of Alzheimer disease. J Geriatr Psychiatry Neurol. 2010;23:213–27.
Whitehouse P, Price D, Clark A, Coyle J, DeLong M. Alzheimer disease: evidence for selective loss of cholinergic neurons in the nucleus basalis. Ann Neurol. 1981;10:122–6.
van de Nes J, Nafe R, Schlote W. Non-tau based neuronal degeneration in Alzheimer’s disease-an immunocytochemical and quantitative study in the supragranular layers of the middle temporal neocortex. Brain Res. 2008;1213:152–65.
Hinton D, Sadun A, Blanks J, Miller C. Optic-nerve degeneration in Alzheimer’s disease. N. Engl J Med. 1986;315:485–7.
Sadun A, Bassi C. Optic nerve damage in Alzheimer’s disease. Ophthalmology 1990;97:9–17.
Ascaso FJ, Cruz N, Modrego PJ, Lopez-Anton R, Santabarbara J, Pascual LF, et al. Retinal alterations in mild cognitive impairment and Alzheimer’s disease: an optical coherence tomography study. J Neurol. 2014;261:1522–30.
Garcia-Martin ES, Rojas B, Ramirez A, de Hoz R, Salazar RJ, Yubero R, et al. Macular thickness as a potential biomarker of mild Alzheimer’s disease. Ophthalmology. 2014;121:1149–53.
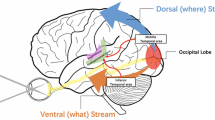
Livingstone MS, Hubel DH. Psychophysical evidence for separate channels for the perception of form, color, movement, and depth. J Neurosci. 1987;7:3416–68.
Braak H, Braak E. Staging of Alzheimer-related cortical destruction. Int Psychogeriatr. 1997;9:257–61.
Cheung CY, Ong YT, Hilal S, Ikram MK, Low S, Ong YL, et al. Retinal ganglion cell analysis using high-definition optical coherence tomography in patients with mild cognitive impairment and Alzheimer’s disease. J Alzheimer’s Dis. 2015;45:45–56.
Jaffe GJ, Caprioli J. Optical coherence tomography to detect and manage retinal disease and glaucoma. Am J Ophthalmol. 2004;137:156–69.
Iseri PK, Altinaş O, Tokay T, Yüksel N. Relationship between cognitive impairment and retinal morphological and visual functional abnormalities in Alzheimer disease. J Neuroophthalmol. 2006;26:18–24.
Blanks JC, Schmidt SY, Torigoe Y, Porrello KV, Hinton DR, Blanks RH. Retinal pathology in Alzheimer’s disease. II. Regional neuron loss and glial changes in GCL. Neurobiol Aging 1996;17:385–95.
Blanks JC, Torigoe Y, Hinton DR, Blanks RH. Retinal pathology in Alzheimer’s disease. I. Ganglion cell loss in foveal/parafoveal retina. Neurobiol Aging 1996;17:377–84.
Parisi V. Correlation between morphological and functional retinal impairment in patients affected by ocular hypertension, glaucoma, demyelinating optic neuritis and Alzheimer’s disease. Semin Ophthalmol. 2003;18:50–7.
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20.
Blanks JC, Hinton DR, Sadun AA, Miller CA. Retinal ganglion cell degeneration in Alzheimer’s disease. Brain Res. 1989;6:364–72.
Blanks JC, Torigoe Y, Hinton DR, Blanks RH. Retinal pathology in Alzheimer’s disease. Ganglion cell loss in foveal/parafoveal retina. Neurobiol Aging. 1996;17:377–84.
Hedges TR, Perez Galves R, Speigelman D, Barbas NR, Peli E, Yardley CJ. Retinal nerve fiber layer abnormalities in Alzheimer’s disease. Acta Ophthalmol Scand. 1996;74:271–5.
Flammer J, Mozaffarieh M. What is the present pathogenetic concept of glaucomatous optic neuropathy? Surv Ophthalmol. 2007;52:162–73.
Hernandez MR. The optic nerve head in glaucoma: role of astrocytes in tissue remodeling. Prog Retin Eye Res. 2000;19:297–321.
Cheung W, Guo L, Cordeiro MF. Neuroprotection in glaucoma: drug-based approaches. Optom Vis Sci. 2008;85:406–16.
Kumar M, Tanwar M, Faiq MA, Pani J, Shamsi MB, Dada T, et al. Mitochondrial DNA nucleotide changes in primary congenital glaucoma patients. Mol Vis. 2013;19:220–30.
Tanwar M, Dada T, Sihota R, Dada R. Mitochondrial DNA analysis in primary congenital glaucoma. Mol Vis. 2010;16:518–33.
Ohno-Matsui K. Parallel findings in age-related macular degeneration and Alzheimer’s disease. Prog Retin Eye Res. 2011;30:217–38.
Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353–6.
Benilova I, Karran E, De SB. The toxic Abeta oligomer and Alzheimer’s disease: an emperor in need of clothes. Nat Neurosci. 2012;15:349–57.
McKinnon SJ1, Lehman DM, Kerrigan-Baumrind LA, Merges CA, Pease ME, Kerrigan DF, et al. Caspase activation and amyloid precursor protein cleavage in rat ocular hypertension. Investig Ophthalmol Vis Sci. 2002;43:1077–87.
Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35:495–516.
Gupta A. Leptin as a neuroprotective agent in glaucoma. Med Hypoth. 2012;81:797–802.
Alexandrov PN, Pogue A, Bhattacharjee S, Lukiw WJ. Retinal amyloid peptides and complement factor H in transgenic models of Alzheimer’s disease. Neuroreport. 2011;22:623–27.
Dutescu RM, Li QX, Crowston J, Masters CL, Baird PN, Culvenor JG, et al. Amyloid precursor protein processing and retinal pathology in mouse models of Alzheimer’s disease. Graefe’s Arch Clin Exp Ophthalmol. 2009;47:1213–21.
Gupta VK, Chitranshi N, Gupta VB, Golzan M, Dhher Y, Wall RV, et al. Amyloid beta accumulation and inner retial degeneration degenerative changes in Alzheimer’s disease transgenic mouse. Neurosci Lett. 2016;623:52–56.
Guo L, Salt TE, Luong V, Wood N, Cheung W, Maass A, et al. Targeting amyloid-beta in glaucoma treatment. Proc Natl Acad Sci. 2007;104:13444–9.
More SS, Vince R. Hyperspectral imaging signatures detect amyloidopathy in alzheimer’s mouse retina well before onset of cognitive decline. ACS Chem Neurosci. 2015;6:306–15.
Hadoux X, Hui F, Lim JKH, et al. Non-invasive in vivo hyperspectral imaging of the retina for potential biomarker use in Alzheimer’s disease. Nat Commun. 2019;10:4227. https://doi.org/10.1038/s41467-019-12242-1.
McKinnon SJ. The cell and molecular biology of glaucoma: common neurodegenerative pathways and relevance to glaucoma. Investig Ophthalmol Vis Sci. 2012;53:2485–7.
Szekely CA, Zandi PP. NSAIDs and Alzheimer’s disease: the epidemiological evidence. CNS Neurol Disord Drug Targets. 2010;9:132–9.
Janciauskiene S, Westin K, Grip O, Krakau T. Detection of Alzheimer peptides and chemokines in the aqueous humor. Eur J Ophthalmol. 2011;21:104–11.
Janciauskiene S, Krakau T. Alzheimer’s peptide and serine proteinase inhibitors in glaucoma and exfoliation syndrome. Doc Ophthalmol. 2003;106:215–23.
Loeffler KU, Edward DP, Tso MO. Tau-2 immunoreactivity of corpora amylacea in the human retina and optic nerve. Investig Ophthalmol Vis Sci. 1993;34:2600–3.
Osborne NN, Lascaratos G, Bron AJ, Childlow G, Wood JP. A hypothesis to suggest that light is a risk factor in glaucoma and the mitochondrial optic neuropathies. Br J Ophthalmol. 2006;90:237–41.
Osborne NN, Alvarez CN, Del Olmo Aguado S. Targeting mitochondrial dysfunction as in aging and glaucoma. Drug Discov Today. 2014;19:1613–22.
Osborne NN, Del Olmo, Aguado S. Maintenance of retinal ganglion cell mitochondrial functions as a neuroprotective strategy in glaucoma. Curr Opin Pharm. 2013;13:16–22.
Osborne NN. Mitochondria: their role in ganglion cell death and survival in primary open angle glaucoma. Exp Eye Res. 2010;90:750–7.
Izzotti A, Bagnis A, Sacca SC. The role of oxidative stress in glaucoma. Mutat Res. 2006;612:105–14.
Jensen M, Basun H, Lannfelt L. Increased cerebrospinal fluid tau in patients with Alzheimer’s disease. Neurosci let. 1995;186:189–91.
Gupta N, Fong J, Ang LC, Yucel YH. Retinal tau pathology in human glaucomas. Can J Ophthalmol. 2008;43:53–60.
Gasparini L, Crowther RA, Martin KR, Berg N, Coleman M, Goedert M, et al. Tau inclusions in retinal ganglion cells of human P301S tau transgenic mice: effects on axonal viability. Neurobiol Aging. 2011;32:419–33.
Schon C, Hoffmann NA, Ochs SM, Burgold S, Filser S, Steinbach S, et al. Long-term in vivo imaging of fibrillar tau in the retina of P301S transgenic mice. PLoS ONE 2012;7:e53547.
Stover KR, Campbell MA, Van Winssen CM, Brown RE. Early detection of cognitive deficits in the 3xTg-AD mouse model of Alzheimer’s disease. Behav Brain Res. 2015;289:29–38.
Chiasseu M, Cueva Vargas JL, Destroismaisons L, Vande Velde C, Leclerc N, Di Polo A. Tau accumulation, altered phosphorylation, and missorting promote neurodegeneration in glaucoma. J Neurosci. 2016;25:5785–98.
Dilsiz N, Sahaboglu A, Yildiz MZ, Reichenbach A. Protective effects of various antioxidants during ischemia-reperfusion in the rat retina. Graefes Arch Clin Exp Ophthalmol. 2006;244:627–33.
Agapova OA, Ricard CS, Salvador-Silva M, Hernandez MR. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human optic nerve head astrocytes. Glia. 2001;33:205–16.
Williams PA, Thirgood RA, Oliphant H, Frizzati A, Littlewood E, Votruba M, et al. Retinal ganglion cell dendritic degeneration in a mouse model of Alzheimer’s disease. Neurobiol Aging. 2013;34:1799–806.
Fischer AJ, Dierks BD, Reh TA. Exogenous growth factors induce the production of ganglion cells at the retinal margin. Development. 2002;129:2283–91.
Choi J, Ko J, Racz B, Burette A, Lee JR, Kim S, et al. Regulation of dendritic spine morphogenesis by insulin receptor substrate 53, a downstream effector of Rac1 and Cdc42 small GTPases. J Neurosci. 2005;25:869–79.
Steen E, Terry BM, Rivera EJ, Cannon JL, Neely TR, Tavares R, et al. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease—is this type 3 diabetes? J Alzheimers Dis. 2005;7:63–80.
Moroo I, Yamada T, Makino H, Tooyama I, McGeer PL, McGeer EG, et al. Loss of insulin receptor immunoreactivity from the substantia nigra pars compacta neurons in Parkinson’s disease. Acta Neuropathol. 1994;87:343–8.
Zhao L, Teter B, Morihara T, Lim GP, Ambegaokar SS, Ubeda OJ, et al. Insulindegrading enzyme as a downstream target of insulin receptor signalling cascade: implications for Alzheimer’s disease intervention. J Neurosci. 2004;24:11120–6.
Farris W, Mansourian S, Chang Y, Lindsley L, Eckman EA, Frosch MP, et al. Insulin-degrading enzyme regulates the levels of insulin, amyloid betaprotein, and the beta-amyloid precursor protein intracellular domain in vivo. Proc Natl Acad Sci USA. 2003;100:4162–7.
Qian W, Shi J, Yin X, Iqbal K, Grundke-Iqbal I, Gong CX, et al. PP2A regulates tau phosphorylation directly and also indirectly via activating GSK-3beta. J Alzheimers Dis. 2010;19:1221–9.
Rodrigues M, Waldbillig RJ, Rajagopalan S, Hackett J, LeRoith D, Chader GJ. Retinal insulin receptors: localization using a polyclonal anti-insulin receptor antibody. Brain Res. 1988;443:389–94.
de la Monte SM, Wands JR. Alzheimer’s disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. 2008;2:1101–13.
Oh SW, Lee S, Park, Kim DJ. Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabetes Metab Res Rev. 2005;21:434–40.
Hepburn DA, Fisher BM, Thomson I, Barrie T, Frier BM. Autonomic mechanisms underlying intraocular pressure changes during insulininduced hypoglycaemia in normal human subjects: effects of pharmacological blockade. Clin Sci. 1991;80:333–8.
Berdahl JP, Allingham RR, Johnson DH. Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma. Ophthalmology. 2008;115:763–8.
Edwards ME, Wang SS, Good TA. Role of viscoelastic properties of differentiated SH-SY5Y human neuroblastoma cells in cyclic shear stress injury. Biotechnol Prog. 2001;17:760–7.
Singh K, Shrivastava A. Intraocular pressure fluctuations: how much do they matter? Curr Opin Ophthalmol. 2009;20:84–7.
Bengtsson B, Leske MC, Hyman L, Heijl A. Early manifest glaucoma trial group. Fluctuation of intraocular pressure and glaucoma progression in the early manifest glaucoma trial. Ophthalmology. 2007;114:205–9.
Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Ren R, Jonas JB, Tian G, Zhen Y, Ma K, Li S, et al. Cerebrospinal fluid pressure in glaucoma: a prospective study. Ophthalmology. 2010;117:259–66.
Chang TC, Singh K. Glaucomatous disease in patients with normal pressure hydrocephalus. J Glaucoma. 2009;18:243–6.
Wostyn P, Audenaert K, De Deyn PP. Alzheimer’s disease-related changes in diseases characterized by elevation of intracranial or intraocular pressure. Clin Neurol Neurosurg. 2008;110:101–9.
Silverberg G, Mayo M, Saul T, Fellmann J, McGuire D. Elevated cerebrospinal fluid pressure in patients with Alzheimer’s disease. Cerebrospinal Fluid Res. 2006;3:7.
Wostyn P, Audenaert K, De Deyn PP. Alzheimer’s disease and glaucoma: is there a causal relationship? Br J Ophthalmol. 2009;93:1557–9.
Killer HE, Jaggi GP, Flammer J, Miller NR. Is open-angle glaucoma caused by impaired cerebrospinal fluid circulation: around the optic nerve? Clin Exp Ophthalmol. 2008;36:308–11.
Venkataraman ST, Flanagan JG, Hudson C. Vascular reactivity of optic nerve head and retinal blood vessels in glaucoma-a review. Microcirculation. 2011;17:568–81.
Moore D, Harris A, Wudunn D, Kheradiya N, Siesky B. Dysfunctional regulation of ocular blood flow: a risk factor for glaucoma? Clin Ophthalmol. 2008;2:849–61.
Flammer J. The vascular concept in glaucoma. Surv Ophthalmol. 1994;38:S3–6.
Michelson G, Langhans MJ, Harazny J, Dichtl A. Visual field defect and perfusion of the juxtapapillary retina and the neuroretinal rim area in primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 1998a;236:80–5.
Michelson G, Welzenbach J, Pal I, Harazny J. Automatic full field analysis of perfusion images gained by scanning laser Doppler flowmetry. Br J Ophthalmol. 1998b;82:1294–1300.
Harju M, Vesti E. Blood flow of the optic nerve head and peripapillary retina in exfoliation syndrome with unilateral glaucoma or ocular hypertension. Graefes Arch Clin Exp Ophthalmol. 2001;239:271–7.
Yin ZQ, Vaegan, Millar TJ, Beaumont P, Sarks S. Widespread choroidal insufficiency in primary open-angle glaucoma. J Glaucoma. 1997;6:23–32.
Drance S, Anderson DR, Schulzer M. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol. 2001;131:699–708.
Flammer J, Kaiser H, Haufschild T. Susac syndrome: a vasospastic disorder? Eur J Ophthalmol. 2001a;11:175–9.
Flammer J, Pache M, Resink T. Vasospasm, its role in the pathogenesis of diseases with particular reference to the eye. Prog Retin Eye Res. 2001b;20:319–49.
Pluta R. The role of apolipoprotein E in the deposition of β-amyloid peptide during ischemia–reperfusion brain injury. A model of early Alzheimer’s disease. Ann NY Acad Sci. 2000a;903:324–34.
Pluta R, Jabłoński M, Czuczwar SJ. Postischemic dementia with Alzheimer phenotype: selectively vulnerable versus resistant areas of the brain and neurodegeneration versus β-amyloid peptide. Folia Neuropathol. 2012b;50:101–9.
Pluta R, Kida E, Lossinsky AS, Golabek AA, Mossakowski MJ, Wisniewski HM. Complete cerebral ischemia with short-term survival in rats induced by cardiac arrest: I. Extracellular accumulation of Alzheimer’s β-amyloid protein precursor in the brain. Brain Res. 1994b;649:323–8.
Ishimaru H, Ishikawa K, Haga S, Shoji M, Ohe Y, Haga C, et al. Accumulation of apolipoprotein E and β-amyloid-like protein in a trace of the hippocampal CA1 pyramidal cell layer after ischaemic delayed neuronal death. NeuroReport. 1996a;7:3063–7.
Armstrong RA. Plaques and tangles and the pathogenesis of Alzheimer’s disease. Folia Neuropathol. 2006;44:1–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sen, S., Saxena, R., Tripathi, M. et al. Neurodegeneration in Alzheimer’s disease and glaucoma: overlaps and missing links. Eye 34, 1546–1553 (2020). https://doi.org/10.1038/s41433-020-0836-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0836-x
This article is cited by
-
Hippocampal subregions functional connectivity alterations in primary angle-closure glaucoma patients with cognitive dysfunction: a resting-state fMRI study
BMC Neurology (2025)
-
Towards a multi-organ, multi-omics medical digital twin
Nature Biomedical Engineering (2025)
-
The association between antiglaucomatous agents and Alzheimer’s disease
Eye (2024)
-
Risk of glaucoma to subsequent dementia or cognitive impairment: a systematic review and meta-analysis
Aging Clinical and Experimental Research (2024)
-
Convolutional neural network-based classification of glaucoma using optic radiation tissue properties
Communications Medicine (2024)