Abstract
Background
The specialty-registration of independent prescribing (IP) was introduced for optometrists in 2008, which extended their roles including into acute ophthalmic services (AOS). The present study is the first since IP’s introduction to test concordance between IP optometrists and consultant ophthalmologists for diagnosis and management in AOS.
Methods
The study ran prospectively for 2 years at Manchester Royal Eye Hospital (MREH). Each participant was individually assessed by an IP optometrist and then by the reference standard of a consultant ophthalmologist; diagnosis and management were recorded on separate, masked proformas. IP optometrists were compared to the reference standard in stages. Cases of disagreement were arbitrated by an independent consultant ophthalmologist. Cases where disagreement persisted after arbitration underwent consensus-review. Agreement was measured with percentages, and where possible kappa (Κ), for: diagnosis, prescribing decision, immediate management (interventions during assessment) and onward management (review, refer or discharge).
Results
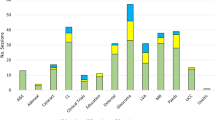
A total of 321 participants presented with 423 diagnoses. Agreement between all IP optometrists and the staged reference standard was as follows: ‘almost perfect’ for diagnosis (Κ = 0.882 ± 0.018), ‘substantial’ for prescribing decision (Κ = 0.745 ± 0.034) and ‘almost perfect’ for onward management (0.822 ± 0.032). Percentage-agreement between all IP optometrists and the staged reference standard per diagnosis was 82.0% (CI 78.1–85.4%), and per participant using stepwise weighting was 85.7% (CI 81.4–89.1%).
Conclusions
Clinical decision-making in MREH’s AOS by experienced and appropriately trained IP optometrists is concordant with consultant ophthalmologists. This is the first study to explore and validate IP optometrists’ role in the high-risk field of AOS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Blunt I, Bardsley M, Dixon J, Trends in emergency admissions in England 2004–2009: is greater efficiency breeding inefficiency? London: Nuffield Trust; 2010. https://www.kingsfund.org.uk/publications/how-nhs-performing-june-2018. Accessed 5 Feb 2020.
Office for National Statistics, Population estimates for the UK, England and Wales, Scotland and Northern Ireland: mid-2017. 2018: https://webarchive.nationalarchives.gov.uk/20180904135853/https://www.ons.gov.uk/releases/populationestimatesforukenglandandwalesscotlandandnorthernirelandmid2017?:uri=releases/populationestimatesforukenglandandwalesscotlandandnorthernirelandmid2017. Accessed 5 Feb 2020.
Smith HB, Daniel CS, Verma S. Eye casualty services in London. Eye. 2013;27:320–8.
Royal College of Ophthalmologists, Workforce Census 2016. 2016: https://www.rcophth.ac.uk/wp-content/uploads/2017/03/RCOphth-Workforce-Census-2016.pdf. Accessed 5 Feb 2020.
Anandaciva S, Jabbal J, Maguire D, Ward D, How is the NHS performing? June 2018 quarterly monitoring report. 2018, London: The King’s Fund. https://www.kingsfund.org.uk/publications/how-nhs-performing-june-2018 Accessed 5 Feb 2020.
Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract. 2013;63:e813–20.
Harper R, Creer R, Jackson J, Erlich D, Tompkin A, Bowen M, et al. Scope of practice of optometrists working in the UK Hospital Eye Service: a national survey. Ophthalmic Physiol Opt. 2015;36:197–206.
Crown J. Review of prescribing, supply and administration of medicines. Final Report (Crown II Report). Department of Health, Editor. 1999. London.
Hammond CJ, Shackleton J, Flanagan DW, Herrtage J, Wade J. Comparison between an ophthalmic optician and an ophthalmologist in screening for diabetic retinopathy. Eye. 1996;10:107–12.
Oster J, Culham LE, Daniel R. An extended role for the hospital optometrist. Ophthalmic Physiol Opt. 1999;19:351–6.
Spry PG, Spencer IC, Sparrow JM, Peters TJ, Brookes ST, Gray S, et al. The Bristol Shared Care Glaucoma Study: reliability of community optometric and hospital eye service test measures. Br J Ophthalmol. 1999;83:707–12.
Gray SF, Spry PG, Brookes ST, Peters TJ, Spencer IC, Baker IA, et al. The Bristol shared care glaucoma study: outcome at follow up at 2 years. Br J Ophthalmol. 2000;84:456–63.
Banes MJ, Culham LE, Bunce C, Xing W, Viswanathan A, Garway-Heath D. Agreement between optometrists and ophthalmologists on clinical management decisions for patients with glaucoma. Br J Ophthalmol. 2006;90:579–85.
Azuara-Blanco A, Burr J, Thomas R, Maclennan G, McPherson S. The accuracy of accredited glaucoma optometrists in the diagnosis and treatment recommendation for glaucoma. Br J Ophthalmol. 2007;91:1639–43.
Vernon SA, Adair A. Shared care in glaucoma: a national study of secondary care lead schemes in England. Eye. 2010;24:265–9.
Ho S, Vernon SA. Decision making in chronic glaucoma-optometrists vs ophthalmologists in a shared care service. Ophthalmic Physiol Opt. 2011;31:168–73.
Marks JR, Harding AK, Harper RA, Williams E, Haque S, Spencer AF, et al. Agreement between specially trained and accredited optometrists and glaucoma specialist consultant ophthalmologists in their management of glaucoma patients. Eye. 2012;26:853–61.
Roberts HW, Rughani K, Syam P, Dhingra S, Ramirez-Florez S. The Peterborough scheme for community specialist optometrists in glaucoma: results of 4 years of a two-tiered community-based assessment and follow-up service. Curr Eye Res. 2015;40:690–6.
Voyatzis G, Roberts HW, Keenan J, Rajan MS. Cambridgeshire cataract shared care model: community optometrist-delivered postoperative discharge scheme. Br J Ophthalmol. 2014;98:760–4.
Bowes OMB, Shah P, Rana M, Farrell S, Rajan MS. Quality indicators in a community optometrist led cataract shared care scheme. Ophthalmic Physiol Opt. 2018;38:183–92.
Konstantakopoulou E, Edgar DF, Harper RA, Baker H, Sutton M, Janikoun S, et al. Evaluation of a minor eye conditions scheme delivered by community optometrists. BMJ Open. 2016;6:e011832.
Hau S, Ehrlich D, Binstead K, Verma S. An evaluation of optometrists’ ability to correctly identify and manage patients with ocular disease in the accident and emergency department of an eye hospital. Br J Ophthalmol. 2007;91:437–40.
College of Optometrists, How to use the Clinical Management Guidelines. 2020. https://www.college-optometrists.org/guidance/clinical-management-guidelines/what-are-clinical-management-guidelines.html. Accessed 5 Feb 2020.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Adair JG. The Hawthorne effect: a reconsideration of the methodological artefact. J Appl Psychol. 1984;69:334–45.
Royal College of Ophthalmologists, The Common Clinical Competency Framework for Non-medical Ophthalmic Healthcare Professionals in Secondary Care. 2016. https://www.rcophth.ac.uk/wp-content/uploads/2017/01/CCCF-Acute-Emergency-Care.pdf. Accessed 5 Feb 2020.
Jones NP, Hayward JM, Khaw PT, Claoue CM, Elkington AR. Function of an ophthalmic “accident and emergency” department: results of a six month survey. Br Med J. 1986;292:188–90.
Vernon SA. Analysis of all new cases seen in a busy regional centre ophthalmic casualty department during 24-week period. J R Soc Med. 1983;76:279–82.
Vlaev I, King D, Dolan P, Darzi A. The theory and practice of ‘nudging’: changing health behaviors. Public Adm Rev. 2016;76:550–61.
Dhalmann-Noor AH, Gupta N, Hay GR, Cates AC, Galloway G, Jordan K, et al. Streamlining the patient journey; The interface between community- and hospital-based eye care. Clin Gov. 2007;13:185–91.
General Optical Council. Education Strategic Review. 2019. https://www.optical.org/en/Education/education-strategic-review-est/index.cfm. Accessed 5 Feb 2020.
Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672.
Acknowledgements
The authors would like to acknowledge the participants, and the research teams at MREH and Aston University.
Funding
The study was awarded a Small Grant Scheme by the College of Optometrists.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Todd, D., Bartlett, H., Thampy, R. et al. Agreement in clinical decision-making between independent prescribing optometrists and consultant ophthalmologists in an emergency eye department. Eye 34, 2284–2294 (2020). https://doi.org/10.1038/s41433-020-0839-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0839-7