Abstract
Purpose
Post-operative cystoid macular oedema (CMO) can cause deterioration of vision following routine cataract surgery. The incidence of persistent CMO (pCMO; defined as CMO present after 3 months) following uncomplicated surgery is uncertain. We wished to identify the incidence, management and visual outcomes of such patients.
Methods
A Scottish Ophthalmological Surveillance Unit (SOSU) questionnaire was sent monthly to every ophthalmic specialist in Scotland over an 18-month period from 1st January 2018 asking them to report all new patients with pCMO confirmed on OCT scanning following uncomplicated cataract surgery. A follow-up questionnaire was sent 9 months after initial presentation.
Results
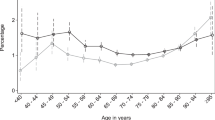
Fourteen cases of pCMO were reported, giving an incidence of 2.2 cases of pCMO per 10,000 uncomplicated cataract surgeries. Mean age was 74.9 years (SD 10.2; range 44–86) with a male preponderance (72.7%). Two patients developed pCMO in each eye. Six cases (46.2%) had hypertension and one had diabetes. Three eyes required intracameral adjuncts (two iris hooks, one intracameral phenylephrine). Postoperative visual acuity (VA) at 3 months was logMAR 0.48 (0.2–0.8). Average mean central retinal thickness (CRT) at 3 months was 497microns (270–788). The most common initial treatment comprised topical steroids and topical NSAIDs (61.5%). Other management strategies included systemic steroids, intravitreal steroids and oral acetazolamide. At 1-year post-op, mean VA was logMAR 0.18 (0.1–0.3) with average mean CRT of 327microns (245–488).
Conclusions
We identified a low incidence of pCMO following uncomplicated cataract surgery in Scotland (0.02%), with inconsistent and variable management regimes. A nationally agreed treatment protocol is required.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Royal College of Ophthalmologists (UK). National ophthalmology database audit. 2019. https://nodaudit.org.uk/u/docs/20/urxqilwxmv/NOD%20Audit%20Annual%20Report%202019.pdf, Accessed 4 Feb 2020.
Busbee BG, Brown MM, Brown GC, Sharma S. Incremental cost-effectiveness of initial cataract surgery. Ophthalmology. 2002;109:606–12.
Law SK, Kim E, Yu F, Caprioli J. Clinical cystoid macular edema after cataract surgery in glaucoma patients. J Glaucoma. 2010;19:100–4.
Chu CJ, Johnston RL, Buscombe C, Sallam AB, Mohamed Q, Yang YC. Risk factors and incidence of macular edema after cataract surgery: a database study of 81984 eyes. Ophthalmology. 2016;123:316–23.
Kim SJ, Schoenberger SD, Thorne JE, Ehlers JP, Yeh S, Bakri SJ. Topical nonsteroidal anti-inflammatory drugs and cataract surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2015;122:2159–68.
Bellocq D, Pierre-Kahn V, Matonti F, Burillon C, Voirin N, Dot C, et al. Effectiveness and safety of dexamethasone implants for postsurgical macular oedema including Irvine-Gass syndrome: the EPISODIC-2 study. Br J Ophthalmol. 2017;101:333–41.
McCafferty S, Harris A, Kew C, Kassm T, Lane L, Levine J, et al. Pseudophakic cystoid macular edema prevention and risk factors; prospective study with adjunctive once daily topical nepafenac 0.3% versus placebo. BMC Ophthalmol. 2017;17:16.
Wendel C, Zakrzewski H, Carleton B, Etminan M, Mikelberg FS. Association of postoperative topical prostaglandin analog or beta-blocker use and incidence of pseudophakic cystoid macular edema. J Glaucoma. 2018;27:402–6.
Wielders LHP, Schouten J, Winkens B, van den Biggelaar F, Veldhuizen CA, Findl O, et al. European multicenter trial of the prevention of cystoid macular edema after cataract surgery in nondiabetics: ESCRS PREMED study report 1. J Cataract Refract Surg. 2018;44:429–39.
Wielders LHP, Schouten J, Winkens B, van den Biggelaar F, Veldhuizen CA, Murta JCN, et al. Randomized controlled European multicenter trial on the prevention of cystoid macular edema after cataract surgery in diabetics: ESCRS PREMED Study Report 2. J Cataract Refract Surg. 2018;44:836–47.
Flach AJ. The incidence, pathogenesis and treatment of cystoid macular edema following cataract surgery. Trans Am Ophthalmol Soc. 1998;96:557–634.
Henderson BA, Kim JY, Ament CS, Ferrufino-Ponce ZK, Grabowska A, Cremers SL. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007;33:1550–8.
Schmier JK, Halpern MT, Covert DW, Matthews GP. Evaluation of costs for cystoid macular edema among patients after cataract surgery. Retina. 2007;27:621–8.
Karacorlu M, Ozdemir H, Karacorlu S. Intravitreal triamcinolone acetonide for the treatment of chronic pseudophakic cystoid macular oedema. Acta Ophthalmol Scand. 2003;81:648–52.
Yonekawa Y, Kim IK. Pseudophakic cystoid macular edema. Curr Opin Ophthalmol. 2012;23:26–32.
Grzybowski A, Sikorski BL, Ascaso FJ, Huerva V. Pseudophakic cystoid macular edema: update 2016. Clin Inter Aging. 2016;11:1221–9.
Puliafito CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995;102:217–29.
Guo S, Patel S, Baumrind B, Johnson K, Levinsohn D, Marcus E, et al. Management of pseudophakic cystoid macular edema. Surv Ophthalmol. 2015;60:123–37.
Foot B, Stanford M, Rahi J, Thompson J. The British Ophthalmological Surveillance Unit: an evaluation of the first 3 years. Eye (Lond). 2003;17:9–15.
Surgical Procedures. Information Services Division. NHS National Services Scotland. 2019. Accessed April 2020 at https://www.isdscotland.org/products-and-services/scottish-atlas-of-variation/view-the-atlas/surgical-procedures.asp.
Rath EZ, Frank RN, Shin DH, Kim C. Risk factors for retinal vein occlusions. A case-control study. Ophthalmology. 1992;99:509–14.
Ponto KA, Elbaz H, Peto T, Laubert-Reh D, Binder H, Wild PS, et al. Prevalence and risk factors of retinal vein occlusion: the Gutenberg Health Study. J Thromb Haemost. 2015;13:1254–63.
Martinez F, Furio E, Fabia MJ, Perez AV, Gonzalez-Albert V, Rojo-Martinez G, et al. Risk factors associated with retinal vein occlusion. Int J Clin Pr. 2014;68:871–81.
Kida T, Morishita S, Kakurai K, Suzuki H, Oku H, Ikeda T. Treatment of systemic hypertension is important for improvement of macular edema associated with retinal vein occlusion. Clin Ophthalmol. 2014;8:955–8.
Arcieri ES, Santana A, Rocha FN, Guapo GL, Costa VP. Blood-aqueous barrier changes after the use of prostaglandin analogues in patients with pseudophakia and aphakia: a 6-month randomized trial. Arch Ophthalmol. 2005;123:186–92.
Flach AJ, Dolan BJ, Irvine AR. Effectiveness of ketorolac tromethamine 0.5% ophthalmic solution for chronic aphakic and pseudophakic cystoid macular edema. Am J Ophthalmol. 1987;103:479–86.
Loewenstein A, Zur D. Postsurgical cystoid macular edema. Dev Ophthalmol. 2010;47:148–59.
Lobo C. Pseudophakic cystoid macular edema. Ophthalmologica. 2012;227:61–7.
Han JV, Patel DV, Squirrell D, McGhee CN. Cystoid macular oedema following cataract surgery: A review. Clin Exp Ophthalmol. 2019;47:346–56.
Packer M, Lowe J, Fine H. Incidence of acute postoperative cystoid macular edema in clinical practice. J Cataract Refract Surg. 2012;38:2108–11.
Thach AB, Dugel PU, Flindall RJ, Sipperley JO, Sneed SR. A comparison of retrobulbar versus sub-Tenon’s corticosteroid therapy for cystoid macular edema refractory to topical medications. Ophthalmology. 1997;104:2003–8.
Sivaprasad S, Bunce C, Wormald R. Non-steroidal anti-inflammatory agents for cystoid macular oedema following cataract surgery: a systematic review. Br J Ophthalmol. 2005;89:1420–2.
Arevalo JF, Maia M, Garcia-Amaris RA, Roca JA, Sanchez JG, Berrocal MH, et al. Intravitreal bevacizumab for refractory pseudophakic cystoid macular edema: the Pan-American Collaborative Retina Study Group results. Ophthalmology. 2009;116:1481–7, 7.e1.
Kessel L, Tendal B, Jorgensen KJ, Erngaard D, Flesner P, Andresen JL, et al. Post-cataract prevention of inflammation and macular edema by steroid and nonsteroidal anti-inflammatory eye drops: a systematic review. Ophthalmology. 2014;121:1915–24.
Mayer WJ, Kurz S, Wolf A, Kook D, Kreutzer T, Kampik A, et al. Dexamethasone implant as an effective treatment option for macular edema due to Irvine-Gass syndrome. J Cataract Refract Surg. 2015;41:1954–61.
Juthani VV, Clearfield E, Chuck RS. Non-steroidal anti-inflammatory drugs versus corticosteroids for controlling inflammation after uncomplicated cataract surgery. Cochrane Database Syst Rev. 2017;7:Cd010516.
Yuksel B, Uzunel UD, Kerci SG, Sagban L, Kusbeci T, Orsel T. Comparison of subtenon triamcinolone acetonide injection with topical nepafenac for the treatment of pseudophakic cystoid macular edema. Ocul Immunol Inflamm. 2017;25:513–9.
Jacobson DR, Dellaporta A. Natural history of cystoid macular edema after cataract extraction. Am J Ophthalmol. 1974;77:445–7.
Suleman H, Mathew M, Lakshmanan A, Abedin A, Orr G. Orbital floor triamcinolone acetonide in the treatment of pseudophakic cystoid macular oedema. Acta Ophthalmol. 2008;86. https://doi.org/10.1111/j.1755-3768.2008.6417.x.
Curkovic T, Vukojevic N, Bucan K. Treatment of pseudophakic cystoid macular oedema. Coll Antropol. 2005;29:103–5.
Hunter AA, Modjtahedi SP, Long K, Zawadzki R, Chin EK, Caspar JJ, et al. Improving visual outcomes by preserving outer retina morphology in eyes with resolved pseudophakic cystoid macular edema. J Cataract Refract Surg. 2014;40:626–31.
Lundström M, Behndig A, Kugelberg M, Montan P, Stenevi U, Thorburn W. Decreasing rate of capsule complications in cataract surgery: eight-year study of incidence, risk factors, and data validity by the Swedish National Cataract Register. J Cataract Refract Surg. 2011;37:1762–7.
Acknowledgements
We thank the SOSU committee for their guidance and support in this project. We thank the Ross Foundation for providing funding through their bursary. We wish to acknowledge the following ophthalmologists who contributed patients to the study: Dr Boyle, Dr Cobb, Dr Drummond, Dr Fairlie, Dr Gillan, Dr Gilmour, Dr MacLeod, Dr MacRae, Dr Pyott, Dr Rotchford and Dr Scott.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Granted.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Erikitola, OO., Siempis, T., Foot, B. et al. The incidence and management of persistent cystoid macular oedema following uncomplicated cataract surgery—a Scottish Ophthalmological Surveillance Unit study. Eye 35, 584–591 (2021). https://doi.org/10.1038/s41433-020-0908-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0908-y
This article is cited by
-
Retrospective evaluation of changes in choroidal thickness after cataract surgery
European Journal of Medical Research (2025)
-
Recent trends and outcomes in immediate and delayed sequential bilateral cataract surgeries: a nationwide cohort study in South Korea
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)
-
Real-world treatment patterns and economic burden of post-cataract macular edema
BMC Ophthalmology (2023)
-
Intraoperative subconjunctival steroid reduces the incidence of pseudophakic macular oedema: a cohort study of 20,066 consecutive phacoemulsification surgeries
Eye (2023)
-
Survey of UKISCRS consultant members regarding preferred practice management of persistent Cystoid Macular Oedema
Eye (2022)