Abstract
Introduction
Acute anterior uveitis (AAU) is a frequently encountered form of uveitis, most commonly an immune-mediated condition associated with the HLA-B27 gene with or without spondyloarthritis, or idiopathic in nature. This study’s aim was to measure clinical and patient-reported outcomes 5 years after the first episode of immune-mediated AAU.
Methods
This is a longitudinal observational study. Ninety-six patients who underwent evaluation at the time of presentation with their first episode of AAU were invited to return for evaluation 5 years later. Standardised ocular history, clinical examination and quality of life (QOL) assessment with the Short Form 36 (SF-36) and the Vision Core Measure 1 (VCM 1) questionnaire were completed and analysed.
Results
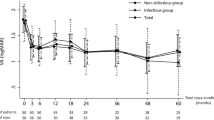
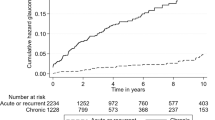
Fifty-four patients (56%) returned for subsequent assessment. Physical function was the only sub scale domain of the SF-36 that had significantly deteriorated over the 5 years since the first episode of AAU (45.95 vs. 49.37, p = 0.003). Only 7.4% (n = 4) of patients expressed “more than a little concern” regarding their vision, reflected by a VCM1 score of 2.0 or more. At 5 years, the mean best corrected visual acuity (BCVA) of eyes affected by AAU was LogMAR 0.02 and only 3% (n = 2) of eyes had a BCVA of less than Logmar of 0.3. Five affected eyes (8%) had developed cataract and no patients had developed glaucoma by the 5 year review.
Conclusions
This study demonstrates that immune-mediated AAU has an excellent 5 year prognosis with minimal impact on patients’ health and vision-related quality of life.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111:491–500. discussion
Darrell RW, Wagener HP, Kurland LT. Epidemiology of uveitis. Incidence and prevalence in a small urban community. Arch Ophthalmol (Chic, Ill: 1960). 1962;68:502–14.
Acharya NR, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, et al. Incidence and prevalence of uveitis: results from the pacific ocular inflammation study. JAMA Ophthalmol. 2013;131:1405–12.
Suhler EB, Lloyd MJ, Choi D, Rosenbaum JT, Austin DF. Incidence and prevalence of uveitis in veterans affairs medical centers of the Pacific Northwest. Am J Ophthalmol. 2008;146:890–6.
Chang JH, McCluskey PJ, Wakefield D. Acute anterior uveitis and HLA-B27. Surv Ophthalmol. 2005;50:364–88.
Haroon M, O’Rourke M, Ramasamy P, Murphy CC, FitzGerald O. A novel evidence-based detection of undiagnosed spondyloarthritis in patients presenting with acute anterior uveitis: the DUET (Dublin Uveitis Evaluation Tool). Ann Rheum Dis. 2015;74:1990–5.
Frost NA, Sparrow JM, Durant JS, Donovan JL, Peters TJ, Brookes ST. Development of a questionnaire for measurement of vision-related quality of life. Ophthalmic Epidemiol. 1998;5:185–210.
O’Rourke M, Haroon M, Alfarasy S, Ramasamy P, FitzGerald O, Murphy CC. The Effect of Anterior Uveitis and Previously Undiagnosed Spondyloarthritis: Results from the DUET Cohort. J Rheumatol. 2017;44:1347–54.
Ware J, Snoww K, Ma K, Bg G SF36 Health Survey: manual and Interpretation Guide. 301993. p. 6:1–6:22, 8:1–8:5, 10:1–10:2.
Park SC, Ham DI. Clinical features and prognosis of HLA-B27 positive and negative anterior uveitis in a Korean population. J Korean Med Sci. 2009;24:722–8.
Linssen A, Meenken C. Outcomes of HLA-B27-positive and HLA-B27-negative acute anterior uveitis. Am J Ophthalmol. 1995;120:351–61.
Power WJ, Rodriguez A, Pedroza-Seres M, Foster CS. Outcomes in anterior uveitis associated with the HLA-B27 haplotype. Ophthalmology. 1998;105:1646–51.
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, et al. The lens opacities classification system III. The longitudinal study of cataract study group. Arch Ophthalmol (Chic, Ill: 1960) 1993;111:831–6.
Ware JE Jr. SF-36 health survey update. Spine 2000;25:3130–9.
Jenkinson C. The SF-36 physical and mental health summary measures: an example of how to interpret scores. J health Serv Res Policy. 1998;3:92–6.
Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ: Br Med J. 1993;306:1437–40.
Frost A, Eachus J, Sparrow J, Peters TJ, Hopper C, Davey-Smith G, et al. Vision-related quality of life impairment in an elderly UK population: associations with age, sex, social class and material deprivation. Eye (Lond, Engl). 2001;15(Pt 6):739–44.
World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
{Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation)}. Off J Eur Union. 2016;L119:1–88.
Jalil A, Yin K, Coyle L, Harper R, Jones NP. Vision-related quality of life and employment status in patients with uveitis of working age: a prospective study. Ocul Immunol Inflamm. 2012;20:262–5.
Gran JT, Skomsvoll JF. The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol. 1997;36:766–71.
Fabiani C, Vitale A, Orlando I, Capozzoli M, Fusco F, Rana F, et al. Impact of uveitis on quality of life: a prospective study from a tertiary referral rheumatology-ophthalmology collaborative uveitis center in Italy. Isr Med Assoc J. 2017;19:478–83.
Schiffman RM, Jacobsen G, Whitcup SM. Visual functioning and general health status in patients with uveitis. Arch Ophthalmol. 2001;119:841–9.
Murphy CC, Hughes EH, Frost NA, Dick AD. Quality of life and visual function in patients with intermediate uveitis. Br J Ophthalmol. 2005;89:1161–5.
Silva LMP, Arantes TE, Casaroli-Marano R, Vaz T, Belfort R, Jr., Muccioli C. Quality of Life and psychological aspects in patients with visual impairment secondary to uveitis: a clinical study in a tertiary care hospital in Brazil. Ocul Immunol Inflamm. 2019;27:99–107.
Institute NE 2010 U.S. Age-specific prevalence rates for cataract by age, and race/ethnicity [webpage]. 2010. https://www.nei.nih.gov/learn-about-eye-health/resources-for-health-educators/eye-health-data-and-statistics/cataract-data-and-statistics.
Miserocchi E, Modorati G, Mosconi P, Colucci A, Bandello F. Quality of life in patients with uveitis on chronic systemic immunosuppressive treatment. Ocul Immunol Inflamm. 2010;18:297–304.
Pavlik VN, Hyman DJ, Vallbona C, Dunn JK, Louis K, Dewey CM, et al. Response rates to random digit dialing for recruiting participants to an onsite health study. Public health Rep. (Wash, DC: 1974). 1996;111:444–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goodchild, C., O’Rourke, M., Haroon, M. et al. 5-year longitudinal study of clinical and patient-reported outcomes in acute anterior uveitis. Eye 35, 651–658 (2021). https://doi.org/10.1038/s41433-020-0937-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-0937-6