Abstract
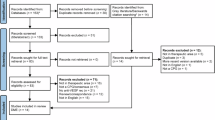
To present an evidence map for explicating research trends and gaps, we systematically review clinical practice guidelines (CPGs) on diabetic retinopathy (DR) and assess the quality of CPGs and consistency of recommendations. A literature search was performed in PubMed, Embase, Web of Science, CPG databases, and website of diabetes society to include the CPGs. The basic information, methodological quality, and reporting quality of CPGs, recommendations for DR were exacted by the Excel 2013. Methodological and reporting quality of DR CPGs were evaluated by AGREE II instrument and RIGHT checklist. The bubble plot format of evidence map was made by Excel 2013. Nineteen CPGs proved eligible, which included eight DR CPGs and 11 comprehensive diabetic CPGs. The identified CPGs were of mixed quality and they scored poorly in the rigor of development, applicability domains by AGREE II. Field two (background) had the highest reporting rate (86.31%) and field five (review and quality assurance) obtained the lowest reporting rate (31.58%) among the seven domains of RIGHT checklist. According to the recommendations of CPGs, there were three inconsistencies in the screening of DR, and CPGs recommendations for treatment were consistent on the whole. At the same time, recommendations for laser therapy were not accurate. Some recommendations were not specific and clear in some DR CPGs. This evidence map could collect and evaluate the characteristics of published CPGs, add to our knowledge and promote the development of trustworthy CPGs for DR.
摘要
我们对糖尿病视网膜病变 (diabetic retinopathy, DR) 的临床实践指南 (clinical practice guidelines, CPGs) 进行了系统回顾, 并评估了CPGs的质量和建议的一致性, 旨在呈现一份详细阐述研究趋势和差距的证据图。我们对PubMed、Embase、科学网、CPG数据库和糖尿病协会网进行了文献检索。采用2013版Excel对CPGs的基本信息、方法学质量、报告质量以及DR指南推荐进行整理, 采用评价工具AGREE-II和 RIGHT检查表对DR CPGs的方法学和报告质量进行评估, 采用2013版Excel制作证据图的气泡图。结果表明19个CPGs是合格的, 其中包括8个DR CPGs和11个综合性糖尿病CPGs。这些CPGs质量参差不齐, 在AGREE II的严格的开发和其领域的适用性很低。在RIGHT检查表的七项评估内容中, 第二项 (背景) 的报告率最高 (86.31%), 第五项 (综述和质量保证) 的报告率最低 (31.58%) 。根据CPGs推荐, 在DR的筛查上存在三项不一致, CPGs在治疗方面的推荐总体上是一致的。同时, 激光治疗的建议并不精准。在某些DR CPGs中一些推荐并不明确。这份证据图收集了并且针对已发表的CPGs特征进行了评价, 增加了我们对DR的认识, 促进了DR的CPGs的可靠性的不断进步。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14.
Cheung N, Mitchell P, Wong TY, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–34.
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21.
Do DV, Wang X, Vedula SS, Marrone M, Sleilati G, Hawkins BS, et al. Blood pressure control for diabetic retinopathy. Cochrane Database Syst Rev. 2015;1:CD006127.
Zhang HW, Zhang H, Grant SJ, Wan X, Li G. Single herbal medicine for diabetic retinopathy. Cochrane Database Syst Rev. 2018;12:CD007939.
Frank RN. Diabetic retinopathy. N Eng J Med. 2004;350:48–58.
Kahn HA, Hiller R. Blindness caused by diabetic retinopathy. Am J Ophthalmol. 1974;78:58–67.
Stolk RP, Vingerling JR, De Jong PTVM, Dielemans I, Hofman A, Lamberts SW, et al. Retinopathy, glucose, and insulin in an elderly population: the rotterdam study. Diabetes. 1995;44:11–5.
Song P, Yu J, Chan KY, Theodoratou E, Rudan I. Prevalence, risk factors and burden of diabetic retinopathy in China: a systematic review and meta-analysis. J Glob Health. 2018;8:010803.
Saaddine JB, Honeycutt AA, Narayan KM, Zhang X, Klein R, Boyle JP. Projection of diabetic retinopathy and other major eye diseases among people with diabetes mellitus: United States, 2005–2050. Arch Ophthalmol. 2008;126:1740–7.
Owolabi MO, Yaria JO, Daivadanam M, Makanjuola AI, Parker G, Oldenburg B, et al. Gaps in guidelines for the management of diabetes in low- and middle-income versus high-income countries—a systematic review. Diabetes Care. 2018;41:1097–105.
Grimshaw J, Freemantle N, Wallace S, Russell I, Hurwitz B, Watt I, et al. Developing and implementing clinical practice guidelines. Qual Saf Health Care. 1995;4:55–64.
Bennett WL, Odelola OA, Wilson LM, Bolen S, Selvaraj S, Robinson KA, et al. Evaluation of guideline recommendations on oral medications for type 2 diabetes mellitus. Ann Intern Med. 2012;156:27.
Hakkennes S, Dodd K. Guideline implementation in allied health professions: a systematic review of the literature. Qual Saf Health Care. 2008;17:296–300.
Petroni A, Corso A, Melano R, Rossi A, Galas M. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:1–72.
Ge L, Tian JH, Li YN, Pan JX, Li G, Wei D, et al. Association between prospective registration and overall reporting and methodological quality of systematic reviews: a meta-epidemiological study. J Clin Epidemiol. 2018;93:45–55.
Erickson J, Sadeghirad B, Lytvyn L, Slavin J, Johnston BC. The scientific basis of guideline recommendations on sugar intake: a systematic review. Ann Intern Med. 2017;166:257–67.
Lam J, Howard BE, Thayer K, Shah RR. Low-calorie sweeteners and health outcomes: a demonstration of rapid evidence mapping (rEM). Environ Int. 2019;123:454–8.
Hetrick SE, Parker AG, Callahan P, Purcell R. Evidence mapping: illustrating an emerging methodology to improve evidence-based practice in youth mental health. J Eval Clin Pract. 2010;16:1025–30.
Graham R, Miller Wolman D, Greenfield S, et al. Clinical practice guidelines we can trust. Institute of Medicine (US) Committee on Standards for developing trustworthy clinical practice guidelines. Washington (DC): The National Academies press (US); 2011.
AGREE Next Steps Consortium. The AGREE II Instrument [2019-04-02]. 2011. http://www.agreetrust.org.
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl J, Flottorp S, et al. A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med. 2017;166:128–32.
Jiang M, Guan WJ, Fang ZF, Xie YQ, Xie JX, Chen H, et al. A critical review of the quality of cough clinical practice guidelines. Chest. 2016;150:777–88.
Bartko JJ. The intraclass correlation coefficient as a measure of reliability. Psychol Rep. 1966;19:3–11.
Alonso-Coello P, Irfan A, Sola I, Gich I, Delgado-Noguera M, Rigau D, et al. The quality of clinical practice guidelines over the last two decades: a systematic review of guideline appraisal studies. Qual Saf Health Care. 2010;19:e58.
The Royal College of Ophthalmologists. Diabetic retinopathy guidelines. 2012.
Institute for Clinical Systems Improvement (ICSI). Diagnosis and management of type 2 diabetes mellitus in adults. 2014.
Korean Diabetes Association (KDA). Treatment guidelines for diabetes. 2015.
American Academy of Ophthalmology. Diabetic retinopathy. 2014.
Haneda M, Noda M, Origasa H, Noto H, Yabe D, Fujita Y, et al. Japanese clinical practice guideline for diabetes 2016. Diabetol Int. 2018;9:1–45.
Ministry of Healthy. Diabetic retinal screening, grading, monitoring and referral guidance. 2016.
Goh SY, Ang SB, Bee YM, Chen YT, Gardner DS, Ho ET, et al. Ministry of health clinical practice guidelines: diabetes mellitus. Singap Med J. 2014;55:334–47.
American Diabetes Association (ADA). Standards of medical care in diabetes. 2017.
International Council of Ophthalmology. ICO guidelines for diabetic eye care. 2017.
American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes. 2018.
Korean Diabetes Association (KDA). Treatment guidelines for diabetes. 2015.
Mahmud FH, Elbarbary NS, Fröhlich-Reiterer E, Holld ReinhardW, Kordonourie Olga, Knipf Mikael, et al. Other complications and associated conditions in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2018;19:275–86.
Polish Diabetes Association (PDA). 2018 Guidelines on the management of diabetic patients. A position of Diabetes Poland. 2018.
Handelsman Y, Bloomgarden ZT, Grunberger G, Umpierrez G, Zimmerman RS, Bailey TS, et al. American association of clinical endocrinologists and american college of endocrinology—clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocr Pract. 2015;21 Suppl 1:1–87.
Diabetes (type 1 and type 2) in children and young people: diagnosis and management. Diabetic foot problems: prevention and management. London (UK); 2015.
Hooper P, Boucher MC, Cruess A, Dawson KG, Delpero W, Greve M, et al. Excerpt from the Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of diabetic retinopathy. Can J Ophthalmol. 2017;52 Suppl 1:S45–74.
Scottish Intercollegiate Guidelines Network (SIGN). Management of diabetes A national clinical guideline. Part of NHS quality improvement Scotland. 2010.
Royal Australian and New Zealand College of Ophthalmologists. Diabetic macular oedema: evidence-based treatment recommendations for Asian countries. 2017.
Chinese Medical Association. Expert consensus on the prevention and treatment of diabetic retinopathy. 2018.
Shen WQ, Yao L, Wang XQ, Hu Y, Bian ZX. Quality assessment of cancer cachexia clinical practice guidelines. Cancer Treat Rev. 2018;70:9–15.
International Clinical Classification System for Diabetic Retinopathy and Diabetic Macular Edema—2012.
Stitt AW, Lois N, Medina RJ, Adamson P, Curtis TM. Advances in our understanding of diabetic retinopathy. Clin Sci. 2013;125:1–17.
Bandello F, Battaglia PM, Tremolada G, Lattanzio R, De Benedetto U, Iacono P. Steroids as part of combination treatment: the future for the management of macular edema? Ophthalmologica. 2010;224 Suppl 1:41–5.
Park YG, Roh YJ. New diagnostic and therapeutic approaches for preventing the progression of diabetic retinopathy. J Diabetes Res. 2016;2016:1753584.
Powers M, Greven M, Kleinman R, Nguyen QD, Do D. Recent advances in the management and understanding of diabetic retinopathy. F1000Res. 2017;6:2063.
Ferris FL 3rd. How effective are treatments for diabetic retinopathy? JAMA. 1993;269:1290–1.
Harjutsalo V, Maric-Bilkan C, Forsblom C, Groop PH. Age at menarche and the risk of diabetic microvascular complications in patients with type 1 diabetes. Diabetologia. 2016;59:472–80.
Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376:124–36.
Lally DR, Shah CP, Heier JS. Vascular endothelial growth factor and diabetic macular edema. Surv Ophthalmol. 2016;61:759–68.
Yilmaz T, Weaver CD, Gallagher MJ, Corderocoma M, Cervantescastaneda RA, Klisovic D, et al. Intravitreal triamcinolone acetonide injection for treatment of refractory diabetic macular edema: a systematic review. Ophthalmology. 2009;116:902–11.
Zhao JX, Wang SD, Pang B, Tan Q. Standards for diagnosis and treatment of traditional Chinese medicine for diabetes with hypertension. World Journal of Integrated Traditional and Western Medicine. 2011;6:638–44.
Deng H, Jing M, Yuan W, Zhan MX, Jing PW. Clinical observation on treating early diabetic retinopathy with compound danshen dripping pills. Chin J Ophthalmol. 2005;15:72–5.
Xing YW, Zou JJ, Shi YQ, Liu ZM. Protection of Fufang Xueshuantong capsule against retinal oxidative damage of diabetic rats. J Med Res. 2016;45:40–3.
Heng LZ, Comyn O, Peto T, Tadros C, Ng E, Sivaprasad S, et al. Diabetic retinopathy: pathogenesis, clinical grading, management and future developments. Diabet Med. 2013;30:640–50.
Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. The Diabetic Retinopathy Study Research Group. Ophthalmology. 1981; 88:583–600.
Sun Y, Gao Y, Chen J, Sun H, Cai YT, Ge L, et al. Evidence mapping of recommendations on diagnosis and therapeutic strategies for diabetes foot: an international review of 22 guidelines. Metabolism. 2019;100:153956.
Feng ZP, Tao QS, Peng DY. Evolution characteristics and enlightenment of self-innovation of traditional Chinese medicine industry. Chin J Chin Materia Medica. 2015;40:2252–7.
Acknowledgements
The authors appreciate Xiaoqing Wang and Nan Yang (Chinese GRADE Center) for their methodological support and assistance with the final editing of the article.
Author information
Authors and Affiliations
Contributions
Y.S., and J.H.-T., did the study design. Y.T.-C., and J.H.-T. performed literature search. Y.S and J.C. contributed to the data acquisition. Y.S., and J.C. contributed to data interpretation and statistical analysis. L.G., and J.H.-Z., supervised and provide mentorship. Y.S., and Y.T.-C. wrote the first draft of the report. Y.S., and J.B.-X., edited the report and all authors contributed to revision of the report. All authors reviewed the paper, approved the final draft, and agreed to submit it for publication.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sun, Y., Cai, Yt., Chen, J. et al. An evidence map of clinical practice guideline recommendations and quality on diabetic retinopathy. Eye 34, 1989–2000 (2020). https://doi.org/10.1038/s41433-020-1010-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-1010-1
This article is cited by
-
Knowledge gaps in diabetes research: an evidence mapping of the literature
Journal of Diabetes & Metabolic Disorders (2022)