Abstract
Background/aims
Optic nerve sheath fenestration (ONSF) is a surgical intervention in the management of idiopathic intracranial hypertension (IIH) infrequently performed in the United Kingdom. Numerous surgical approaches have been described, including medial transconjunctival, lateral and endoscopic. We describe our outcomes and complications from ONSF via a supero-medial eyelid skin crease incision in patients with IIH.
Methods
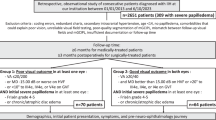
We performed a retrospective review of consecutive patients undergoing ONSF for IIH between January 2011 and December 2017 by a single surgeon.
Results
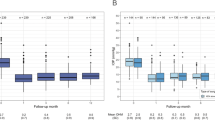
Thirty patients were included in the analysis with a median follow-up of 14.5 months. Bilateral ONSFs were undertaken in 27 (90%). The data from one eye per patient were analysed. The mean kinetic perimetry score in mean radial degrees of the I4e isopter improved from 27.3° to 35.7°, p = 0.04. After removing cases with optic atrophy, the median modified Frisén grade of papilloedema improved from 2.5 to 1.0, p = 0.007. A total of 5/30 (17%) patients had complications: two (7%) had recurrence/late failure (one managed medically and one with cerebrospinal fluid [CSF] diversion surgery), one had transient cotton wool spots post-operatively, one had transient retinal haemorrhages and one patient had a transiently oval pupil. No patients had repeat ONSF, but CSF diversion surgery was subsequently carried out in 4/30 (13%) patients.
Conclusions
ONSF via a supero-medial eyelid skin crease approach is effective at improving visual function in patients with IIH. The complication rates are low when compared with CSF diversion surgery and other surgical approaches for ONSF.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Markey KA, Mollan SP, Jensen RH, Sinclair AJ. Understanding idiopathic intracranial hypertension: mechanisms, management, and future directions. Lancet Neurol. 2016;15:78–91.
Mollan SP, Aguiar M, Evison F, Frew E, Sinclair AJ. The expanding burden of idiopathic intracranial hypertension. Eye. 2019;33:478–85.
McCluskey G, Doherty-Allan R, McCarron P, Loftus AM, McCarron LV, Mulholland D, et al. Meta-analysis and systematic review of population-based epidemiological studies in idiopathic intracranial hypertension. Eur J Neurol. 2018;25:1218–27.
Raoof N, Sharrack B, Pepper IM, Hickman SJ. The incidence and prevalence of idiopathic intracranial hypertension in Sheffield, UK. Eur J Neurol. 2011;18:1266–8.
Best J, Silvestri G, Burton B, Foot B, Acheson J. The incidence of blindness due to idiopathic intracranial hypertension in the UK. Open Ophthalmol J. 2013;7:26–9.
Piper RJ, Kalyvas AV, Young AM, Hughes MA, Jamjoom AA, Fouyas IP. Interventions for idiopathic intracranial hypertension. Cochrane Database Syst Rev. 2015;8:CD003434.
Mollan SP, Ali F, Hassan-Smith G, Botfield H, Friedman DI, Sinclair AJ. Evolving evidence in adult idiopathic intracranial hypertension: pathophysiology and management. J Neurol, Neurosurg, Psychiatry. 2016;87:982–92.
Wall M, McDermott MP, Kieburtz KD, Corbett JJ, Feldon SE, Friedman DI, et al. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA. 2014;311:1641–51.
Ball AK, Howman A, Wheatley K, Burdon MA, Matthews T, Jacks AS, et al. A randomised controlled trial of treatment for idiopathic intracranial hypertension. J Neurol. 2011;258:874–81.
Okoroafor F, Karim MA, Ali A. Idiopathic intracranial hypertension and bariatric surgery: a literature review and a presentation of two cases. Br J Neurosurg. 2019;33:112–14.
Satti SR, Leishangthem L, Chaudry MI. Meta-analysis of CSF diversion procedures and dural venous sinus stenting in the setting of medically refractory idiopathic intracranial hypertension. AJNR Am J Neuroradiol. 2015;36:1899–904. https://doi.org/10.3174/ajnr.A4377.
Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR, et al. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol, Neurosurg, Psychiatry. 2018;89:1088–100.
Fonseca PL, Rigamonti D, Miller NR, Subramanian PS. Visual outcomes of surgical intervention for pseudotumour cerebri: optic nerve sheath fenestration versus cerebrospinal fluid diversion. Br J Ophthalmol. 2014;98:1360–3.
Jaeb Center for Health Research. Surgical Idiopathic Intracranial Hypertension Treatment Trial (SIGHT). Secondary Surgical Idiopathic Intracranial Hypertension Treatment Trial (SIGHT) 2018. https://clinicaltrials.gov/ct2/show/NCT03501966. Accessed March 2020.
Moza K, McMenomey SO, Delashaw JB Jr. Indications for cerebrospinal fluid drainage and avoidance of complications. Otolaryngol Clin North Am. 2005;38:577–82.
Pickard J, Richards H, Seeley H, Mendez RF, Joannides A. UK Shunt registry, draft report 2017: The Society of British Neurological Surgeons, 2017. https://www.sbns.org.uk/index.php/audit/shunt-registry/. Accessed November 2019.
Hickman SJ, Raoof N, Panesar H, McMullan JM, Pepper IM, Sharrack B. Visual outcomes from shunting for idiopathic intracranial hypertension. Neuroophthalmology. 2014;38:310–19.
Vaidya NS, Mahmoud AM, Buzzacco D, Katz SE. Visual outcomes following optic nerve sheath fenestration via the medial transconjunctival approach. Orbit. 2016;35:271–7.
Blessing NW, Tse DT. Optic nerve sheath fenestration: a revised lateral approach for nerve access. Orbit. 2019;38:137–43.
Tarrats L, Hernandez G, Busquets JM, Portela JC, Serrano LA, Gonzalez-Sepulveda L, et al. Outcomes of endoscopic optic nerve decompression in patients with idiopathic intracranial hypertension. Int Forum Allergy Rhinol. 2017;7:615–23.
Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492–5.
Rowe FJ, Rowlands A. Comparison of diagnostic accuracy between Octopus 900 and Goldmann kinetic visual fields. BioMed Res Int. 2014;2014:214829.
Newman WD, Tocher K, Acheson JF. Vigabatrin associated visual field loss: a clinical audit to study prevalence, drug history and effects of drug withdrawal. Eye. 2002;16:567–71.
Scott CJ, Kardon RH, Lee AG, Frisen L, Wall M. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Arch Ophthalmol. 2010;128:705–11.
Pelton RW, Patel BC. Superomedial lid crease approach to the medial intraconal space: a new technique for access to the optic nerve and central space. Ophthalmic Plast Reconstr Surg. 2001;17:241–53.
Kelman SE, Sergott RC, Cioffi GA, Savino PJ, Bosley TM, Elman MJ. Modified optic nerve decompression in patients with functioning lumboperitoneal shunts and progressive visual loss. Ophthalmology. 1991;98:1449–53.
Acheson JF, Green WT, Sanders MD. Optic nerve sheath decompression for the treatment of visual failure in chronic raised intracranial pressure. J Neurol, Neurosurg, Psychiatry. 1994;57:1426–9.
Banta JT, Farris BK. Pseudotumor cerebri and optic nerve sheath decompression. Ophthalmology. 2000;107:1907–12.
Moreau A, Lao KC, Farris BK. Optic nerve sheath decompression: a surgical technique with minimal operative complications. J Neuropphthalmol. 2014;34:34–8.
Corbett JJ, Nerad JA, Tse DT, Anderson R. Results of optic nerve sheath fenestration for pseudotumor cerebri. The lateral orbitotomy approach. Arch Ophthalmol. 1988;106:1391–7.
Gupta AK, Gupta A, Kumar S, Lal V. Endoscopic endonasal management of pseudotumor cerebri: is it effective? Laryngoscope. 2007;117:1138–42.
Sencer A, Akcakaya MO, Basaran B, Yorukoglu AG, Aydoseli A, Aras Y, et al. Unilateral endoscopic optic nerve decompression for idiopathic intracranial hypertension: a series of 10 patients. World Neurosurg. 2014;82:745–50.
Pineles SL, Volpe NJ. Long-term results of optic nerve sheath fenestration for idiopathic intracranial hypertension: earlier intervention favours improved outcomes. Neuroophthalmology. 2013;37:12–19.
Thambisetty M, Lavin PJ, Newman NJ, Biousse V. Fulminant idiopathic intracranial hypertension. Neurology. 2007;68:229–32.
Spoor TC, Ramocki JM, Madion MP, Wilkinson MJ. Treatment of pseudotumor cerebri by primary and secondary optic nerve sheath decompression. Am J Ophthalmol. 1991;112:177–85.
Chandrasekaran S, McCluskey P, Minassian D, Assaad N. Visual outcomes for optic nerve sheath fenestration in pseudotumour cerebri and related conditions. Clin Exp Ophthalmol. 2006;34:661–5.
Friedman DI, Rausch EA. Headache diagnoses in patients with treated idiopathic intracranial hypertension. Neurology. 2002;58:1551–3.
Zis P, Mitsikostas DD. Nocebo responses in brain disease: a systematic review of the current literature. Int Rev Neurobiol. 2018;139:443–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jefferis, J.M., Littlewood, R.A., Pepper, I.M. et al. Optic nerve sheath fenestration via a supero-medial eyelid skin crease approach for the treatment of idiopathic intracranial hypertension in a UK population. Eye 35, 1418–1426 (2021). https://doi.org/10.1038/s41433-020-1024-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-1024-8
This article is cited by
-
Effectiveness of optic nerve sheath fenestration in preserving vision in idiopathic intracranial hypertension: an updated meta-analysis and systematic review
Acta Neurochirurgica (2024)
-
Optic Nerve Sheath Fenestration for Progressive Visual Loss in Cerebral Venous Sinus Thrombosis: A Long-Term Retrospective Observational Study
Neurology and Therapy (2023)