Abstract
Background
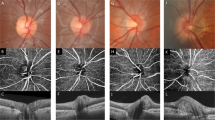
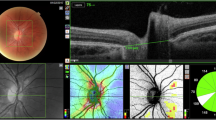
Optic nerve head drusen (ONHD) are considered the most common cause for pseudopapilloedema in children. We aimed to investigate and further characterize a new type of optic nerve head lesion on enhanced depth imaging optical coherence tomography (EDI-OCT) named peripapillary hyperreflective ovoid mass-like structures (PHOMS), and ONHD in asymptomatic children with pseudopapilloedema.
Methods
Retrospective cohort study including 64 eyes from 32 patients with pseudopapilloedema due to PHOMS and/or ONHD. Mean age was 9.0 ± 3.1 years. PHOMS and ONHD were identified and classified on EDI-OCT and infrared images. Ultrasound images were classified for the presence of hyperechogenic structures of the optic nerve head.
Results
On EDI-OCT, PHOMS were detected in 63 out of 64 eyes (98.4%). In 60 eyes (93.8%), small hyperreflective foci inside the PHOMS were present. In all cases, we identified a new ring sign visible on infrared images, corresponding clearly to the edge of the PHOMS as seen on EDI-OCT. On ultrasound, we describe a new feature of PHOMS appearing as small hyperechogenic structures without posterior shadowing. In 13 eyes (20.3%), ONHD were present on EDI-OCT and ultrasound.
Conclusion
This is the first study showing that PHOMS are the most common cause for pseudopapilloedema in children. PHOMS is a new entity of optic nerve head lesions. It might be a precursor of buried optic nerve head drusen, which can lead to visual field defects, haemorrhages and CNV. This study offers new tools to identify and follow-up these lesions early in childhood using EDI-OCT.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kovarik JJ, Doshi PN, Collinge JE, Plager DA. Outcome of pediatric patients referred for papilledema. J AAPOS. 2015;19:344–8.
Chang MY, Pineles SL. Optic disk drusen in children. Surv Ophthalmol. 2016;61:745–58.
Leon M, Hutchinson AK, Lenhart PD, Lambert SR. The cost-effectiveness of different strategies to evaluate optic disk drusen in children. J AAPOS. 2014;18:449–52.
Mishra A, Mordekar SR, Rennie IG, Baxter PS. False diagnosis of papilloedema and idiopathic intracranial hypertension. Eur J Paediatr Neurol. 2007;11:39–42.
Erkkila H. Clinical appearance of optic disc drusen in childhood. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975;193:1–18.
Auw-haedrich C, Staubach F, Witschel H, Breisgau F. Optic disk drusen. Surv Ophthalmol. 2002;47:515–32.
Frisen L, Frise L, Frisen L. Evolution of drusen of the optic nerve head over 23 years. Acta Ophthalmol. 2008;86:111–2.
Spencer TS, Katz BJ, Weber SW, Digre KB. Progression from anomalous optic discs to visible optic disc drusen. J Neuroophthalmol. 2004;24:297–8.
Sato T, Mrejen S, Spaide RF. Multimodal imaging of optic disc drusen. Am J Ophthalmol. 2013;156:275–282.e1.
Gise R, Gaier ED, Heidary G, Gise R, Gaier ED, Heidary G. Diagnosis and imaging of optic nerve head drusen diagnosis and imaging of optic nerve head drusen. Semin Ophthalmol. 2019;0:1–8. https://doi.org/10.1080/08820538.2019.1620804.
Lee KM, Woo SJ, Hwang J-M. Morphologic characteristics of optic nerve head drusen on spectral-domain optical coherence tomography. Am J Ophthalmol. 2013;155:1139–1147.e1.
Silverman AL, Tatham AJ, Medeiros FA, Weinreb RN. Assessment of optic nerve head drusen using enhanced depth imaging and swept source optical coherence tomography. J Neuro-Ophthalmol. 2015;34:198–205.
Traber GL, Weber KP, Sabah M, Keane PA, Plant GT. Enhanced depth imaging optical coherence tomography of optic nerve head drusen a comparison of cases with and without visual field loss. Ophthalmology. 2016;124:66–73.
Malmqvist L, Bursztyn L, Costello F, Digre K, Fraser JA, Fraser C, et al. The optic disc drusen studies consortium recommendations for diagnosis of optic disc drusen using optical coherence tomography. J Neuro-Ophthalmol. 2017;38:299–307.
Merchant KY, Su D, Park SC, Qayum S, Banik R, Liebmann JM, et al. Enhanced depth imaging optical coherence tomography of optic nerve head drusen. Ophthalmology. 2012;120:1409–14.
Slotnick S, Sherman J. Disc drusen. Ophthalmology. 2012;119:652–652.e1.
Lee KM, Woo SJ, Hwang J-M. Differentiation of optic nerve head drusen and optic disc edema with spectral-domain optical coherence tomography. Ophthalmology. 2011;118:971–7.
Chang MY, Velez FG, Demer JL, Bonelli L, Quiros PA, Arnold AC, et al. Accuracy of diagnostic imaging modalities for classifying pediatric eyes as papilledema versus pseudopapilledema. Ophthalmology. 2017;124:1839–48.
Kulkarni KM, Pasol J, Rosa PR, Lam BL. Differentiating mild papilledema and buried optic nerve head drusen using spectral domain optical coherence tomography. Ophthalmology. 2014;121:959–63.
Neudorfer M, Ben-Haim MS, Leibovitch I, Kesler A. The efficacy of optic nerve ultrasonography for differentiating papilloedema from pseudopapilloedema in eyes with swollen optic discs. Acta Ophthalmol. 2013;91:376–80.
Teixeira FJ, Marques RE, Mano SS, Couceiro R, Pinto F. Optic disc drusen in children: morphologic features using EDI-OCT. Eye. 2019. https://doi.org/10.1038/s41433-019-0694-6; https://pubmed.ncbi.nlm.nih.gov/31745329.
McNicholas MM, Power WJ, Griffin JF, Funduscopic W, Normal A. Sonography imaging findings when funduscopic in optic disk drusen: and role in diagnosis findings are normal. Am J Roentgenol. 1994;162:161–3.
Malmqvist L, Lund-Andersen H, Hamann S. Long-term evolution of superficial optic disc drusen. Acta Ophthalmol. 2017;95:352–6.
Lyu IJ, Park K-A, Oh SY. Association between myopia and peripapillary hyperreflective ovoid mass-like structures in children. Sci Rep. 2020;10:2238.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mezad-Koursh, D., Klein, A., Rosenblatt, A. et al. Peripapillary hyperreflective ovoid mass-like structures—a novel entity as frequent cause of pseudopapilloedema in children. Eye 35, 1228–1234 (2021). https://doi.org/10.1038/s41433-020-1067-x
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-020-1067-x
This article is cited by
-
Identifying biomarkers for papilledema and pseudopapilledema
Scientific Reports (2025)
-
Peripapillary hyperreflective ovoid mass-like structure (PHOMS) and optic disc drusen in pediatric pseudo-papilledema
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)
-
Prevalence of peripapillary hyperreflective ovoid mass-like structures (PHOMS) in suspected papilloedema in children
Eye (2023)
-
Response to: Comment on: “Peripapillary hyperreflective ovoid mass-like structures—a novel entity as frequent cause of pseudopapilloedema in children”
Eye (2022)
-
Comment on: ‘Peripapillary hyperreflective ovoid mass-like structures—a novel entity as frequent cause of pseudopapilloedema in children’
Eye (2022)