Abstract
Neuro-ophthalmic features are a known association in tuberculosis, especially common in central nervous system tuberculosis (CNS-TB). They are mostly the result of the visual pathway and/or ocular motor and other cranial nerve involvement. Furthermore, toxic optic neuropathy and paradoxical response to anti-tubercular drugs (ATT) are also not uncommon. The etiopathogenesis is by the complex interplay of various factors like exudates, vasculitis, arachnoiditis, presence of tuberculomas, hydrocephalus, brain infarcts and/or immune-mediated reaction. The entity often poses a diagnostic dilemma for the ophthalmologists/neuro-ophthalmologists and may lead to irreversible vision loss. The presence of neuro-ophthalmic features not only affect the visual outcome but are also predictors of systemic morbidity of the disease. Therefore, understanding and knowledge about this entity are necessary for the comprehensive management of the disease. While various forms of TB including CNS-TB have been well-dealt with in literature, little is discussed specifically about the neuro-ophthalmic manifestations of tuberculosis. Therefore, the purpose of this review is to highlight current understanding of the types of neuro-ophthalmic involvement in tuberculosis, its etiopathogenesis, diagnosis and management.
摘要
摘要
众所周知结核病与神经眼科特征有关, 尤其是在中枢神经系统结核病 (central nervous system tuberculosis, CNS-TB) 常见。它们大多是视觉通路和/或眼运动和其他颅神经受累的结果。此外, 毒性视神经病变和抗结核药物 (anti-tubercular drugs, ATT) 的副作用也并不少见。其病因是由于各种因素如渗出、血管炎、蛛网膜炎、结核瘤、脑积水、脑梗塞和/或免疫因素介导的复杂的相互作用引起的。这种复杂的相互作用网络给眼科医生/神经眼科医生对于疾病诊断的困境, 并可导致不可逆的视力丧失。神经眼科特征的存在不仅影响视力结局, 也是疾病系统发病率的预测因素。因此, 了解和学习这个知识体系对于疾病的综合管理是必要的。虽然文献中对包括CNS-TB在内的各种类型的结核都有很好的论述, 但很少有人针对结核的神经眼科表现进行讨论。因此, 本综述旨在强调结核合并神经眼科疾病的类型、发病机制、诊断和治疗。
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Organization WH. WHO Global tuberculosis report 2019. World Health Organization. 2020. Available from: http://www.who.int/tb/publications/global_report/en/.
WHO. WHO | Tuberculosis and HIV. WHO. 2015. Available from: http://www.who.int/hiv/topics/tb/en/.
Rieder HL, Snider DE Jr, Cauthen GM. Extrapulmonary tuberculosis in the United States. Am Rev Respir Dis. 1990;141:347–51.
CDC. Extrapulmonary tuberculosis cases and percentages by site of disease: reporting areas. Atlanta, GA: Centers Disease Control and Prevention; 2005.
Berger JR. Tuberculous meningitis. Curr Opin Neurol 1994;7:191–200.
Amitava AK, Alam S, Hussain R. Neuro-ophthalmic features in pediatric tubercular meningoencephalitis. J Pediatr Ophthalmol Strabismus. 2001;38:229–34.
Sinha MK, Garg RK, Anuradha HK, Agarwal A, Singh MK, Verma R. et al. Vision impairment in tuberculous meningitis: predictors and prognosis. J Neurol Sci. 2010;290:27–32. https://doi.org/10.1016/j.jns.2009.12.012.
Verma R, Sarkar S, Garg RK, Malhotra HS, Sharma PK, Saxena S. Ophthalmological manifestation in patients of tuberculous meningitis. QJM. 2019;112:409–19.
Dastur HM. Diagnosis and neurosurgical treatment of tuberculous disease of the CNS. Neurosurg Rev. 1983;6:111–7.
Garg RK, Paliwal V, Malhotra HS. Tuberculous optochiasmatic arachnoiditis: a devastating form of tuberculous meningitis. Expert Rev Anti Infect Ther. 2011;9:719–29.
Paige C, Bishai WR. Penitentiary or penthouse condo: the tuberculous granuloma from the microbe’s point of view. Cell Microbiol. 2010;12:301–9. https://doi.org/10.1111/j.1462-5822.2009.01424.x. Accessed 10 May 2020.
Gray F, Duyckaerts C, de Girolami U. Escourolle and Poirier’s manual of basic neuropathology. Oxford University Press, Oxford; 2018. https://doi.org/10.1093/med/9780190675011.001.0001.
Aulakh R, Chopra S. Pediatric tubercular meningitis: a review. J Pediatr Neurosci. 2018;13:373–82. Available from: /pmc/articles/PMC6413593/?report=abstract. Accessed 22 Jul 2020.
Teoh R, Poon W, Humphries MJ, O’Mahony G. Suprasellar tuberculoma developing during treatment of tuberculous meningitis requiring urgent surgical decompression. J Neurol. 1988;235:321–2.
Afghani B, Lieberman JM. Paradoxical enlargement or development of intracranial tuberculomas during therapy: case report and review. Clin Infect Dis. 1994;19:1092–9.
Kalkan A, Serhatlioglu S, Ozden M, Denk A, Demirdag K, Yilmaz T, et al. Paradoxically developed optochiasmatic tuberculoma and tuberculous lymphadenitis: a case report with 18-month follow up by MRI. South Med J. 2006;99:388–92.
Van Crevel R, Kleinnijenhuis J, Oosting M, Joosten LAB, Netea MG. Innate immune recognition of mycobacterium tuberculosis. Clin Dev Immunol. 2011;2011:405310.
Mishra M, Rath S, Acharya B, Mohanty S, Panigrahi B. Neuro-ophthalmic profile in TBM. Ind J Tub. 1985;23:142.
Mooney AJ. Some ocular sequelae of tuberculous meningitis: a preliminary survey, 1953–4. Am J Ophthalmol. 1956;41:753–68. https://doi.org/10.1016/0002-9394(56)91768-8.
Gupta V, Gupta A, Rao NA. Intraocular Tuberculosis-An Update. Surv Ophthalmol 2007;52:561–87.
Davis EJ, Rathinam SR, Okada AA, Tow SL, Petrushkin H, Graham EM, et al. Clinical spectrum of tuberculous optic neuropathy. J Ophthalmic Inflamm Infect. 2012;2:183–9.
Narayanan S, Prakash D, Subramaniam G. Bilateral primary optic neuropathy as the presenting manifestation of tuberculosis in an immunocompetent patient. IDCases. 2019;18:e00579. https://doi.org/10.1016/j.idcr.2019.e00579.
Jacob M, Kodjikian L, Ponceau B, Grange JD. La névrite péri-optique: complication méconnue de la tuberculose? J Français d'Ophtalmologie. 2006;29:328.e1–328.e5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16557166. Accessed 11 May 2020.
Ryu WY, Kim JS. Optic perineuritis simultaneously associated with active pulmonary tuberculosis without intraocular tuberculosis. Int J Ophthalmol. 2017;10:1477–8.
Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiological features. Arch Ophthalmol. 2001;119:1299–306. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11545635. Accessed 11 May 2020.
Murugan S, Sundaralakshmi P. Commentary: tuberculosis in neuro ophthalmology—how different it is? Indian J Ophthalmol. 2019;67:1212–4.
Leonard JM, Des Prez RM. Tuberculous meningitis. Infect Dis Clin N Am. 1990;4:769–87.
Abbas A, Shukla R, Ahuja RC, Gupta RK, Singh KD, Saxena S. Visual impairment in HIV negative tuberculosis meningitis. J Meningitis. 2015;1:1–7.
Moghekar AR. Neuro-ophthalmic manifestations in adult hydrocephalus. Int Ophthalmol Clin. 2014;54:115–21.
Murthy JMK. Management of intracranial pressure in tuberculous meningitis. Neurocrit Care 2005;2:306–12.
Raut T, Garg RK, Jain A, Verma R, Singh MK, Malhotra HS. et al. Hydrocephalus in tuberculous meningitis: Incidence, its predictive factors and impact on the prognosis. J Infect. 2013;66:330–7. https://doi.org/10.1016/j.jinf.2012.12.009.
Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical response to tuberculostatic chemotherapy. Review of the literature and own experience. Acta Neurochir. 1997;139:194–202.
Anupriya A, Sunithi M, Maya T, Goel M, Alexander M, Aaron S, et al. Tuberculous optochiasmatic arachnoiditis. Neurol India. 2010;58:732–5.
Grzybowski A, Zülsdorff M, Wilhelm H, Tonagel F. Toxic optic neuropathies: an updated review. Acta Ophthalmol. 2015;93:402–10. Available from: https://pubmed.ncbi.nlm.nih.gov/25159832/. Accessed 21 Sep 2020.
Wilkinson RG, Shepherd RG, Thomas JP, Baughn C. Stereospecificity in a new type of synthetic antituberculous agent. J Am Chem Soc. 1961;83:2212–3.
Leibold JE. The ocular toxicity of ethambutol and its relation to dose. Ann N Y Acad Sci. 1966;135:904–9. Available from: https://pubmed.ncbi.nlm.nih.gov/5220245/. Accessed 30 Jul 2020.
Kahana LM. Toxic ocular effects of ethambutol. Can Med Assoc J. 1987;137:213–6. Available from: /pmc/articles/PMC1492367/?report=abstract. Accessed 30 Jul 2020.
Van Dijk BW, Spekreijse H. Ethambutol changes the color coding of carp retinal ganglion cells reversibly. Investig Ophthalmol Vis Sci. 1983;24:128–33.
Polak BCP, Leys M, Van Lith GHM. Blue yellow colour vision changes as early symptoms of ethambutol oculotoxicity. Ophthalmologica 1985;191:223–6. Available from: http://library1.nida.ac.th/termpaper6/sd/2554/19755.pdf.
Behbehani R. Clinical approach to optic neuropathies. Clin Ophthalmol. 2007;1:233–46. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19668477. Accessed 30 Apr 2020.
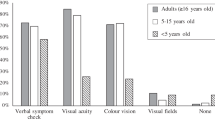
Mandal S, Saxena R, Dhiman R, Mohan A, Padhy SK, Phuljhele S, et al. Prospective study to evaluate incidence and indicators for early detection of ethambutol toxicity. Br J Ophthalmol. 2020:bjophthalmol-2020-316897. Available from: http://bjo.bmj.com/lookup/doi/10.1136/bjophthalmol-2020-316897. Accessed 30 Jul 2020.
Koul PA. Ocular toxicity with ethambutol therapy: timely recaution. Lung India. 2015;32:1–3. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4298909/. Accessed 22 Jul 2020.
Menon V, Jain D, Saxena R, Sood R. Prospective evaluation of visual function for early detection of ethambutol toxicity. Br J Ophthalmol. 2009;93:1251–4. Available from: https://pubmed.ncbi.nlm.nih.gov/19525243/. Accessed 22 Jul 2020.
Miller NR, Walsh FB. In: Frank B, Hoyt WF, editors. Walsh and Hoyt’s clinical neuro-ophthalmology. Lippincott Williams & Wilkins, Philadelphia; 2005.
Van Stavern GP, Newman NJ. Optic neuropathies. An overview. Ophthalmol Clin North Am. 2001;14:61–71.
Kass I, Mandel W, Cohen H, Dressler SH. Isoniazid as a cause of optic neuritis and atrophy. J Am Med Assoc. 1957;164:1740–3. https://doi.org/10.1001/jama.1957.02980160012003.
De Vriese AS, Van Coster R, Smet J, Seneca S, Lovering A, Van Haute LL, et al. Linezolid-induced inhibition of mitochondrial protein synthesis. Clin Infect Dis. 2006;42:1111–7.
Javaheri M, Khurana RN, O’Hearn TM, Lai MM, Sadun AA. Linezolid-induced optic neuropathy: a mitochondrial disorder? Br J Ophthalmol. 2007;91:111–5.
Nataprawira HM, Ruslianti V, Solek P, Hawani D, Milanti M, Anggraeni R, et al. Outcome of tuberculous meningitis in children: the first comprehensive retrospective cohort study in Indonesia. Int J Tuberc Lung Dis. 2016;20:909–14.
Thwaites GE, Hien TT. Tuberculous meningitis: many questions, too few answers. Lancet Neurol. 2005;4:160–70.
Verdon R, Chevret S, Laissy J-P, Wolff M. Tuberculous meningitis in adults: review of 48 cases. Clin Infect Dis. 1996;22:982–8.
Kent SJ, Crowe SM, Yung A, Lucas CR, Mijch AM. Tuberculous meningitis: a 30-year review. Clin Infect Dis Publ Infect Dis Soc Am. 1993;17:987–94.
Kumar S, Rajshekher G, Prabhakar S. Isolated bilateral ptosis as the presentation of midbrain tuberculoma. Neurol India. 2008;56:212–3.
Werring DJ, Marsden CD. Visual hallucinations and palinopsia due to an occipital lobe tuberculoma. J Neurol Neurosurg Psychiatry. 1999;66:684.
Motamed M, Kalan A. Gradenigo’s syndrome. Postgrad Med J. 2000;76:559–60. Available from: www.postgradmedj.com. Accessed 22 Jul 2020.
Zatjirua V, Butler J, Carr J, Henning F. Neuromyelitis optica and pulmonary tuberculosis: a case-control study. Int J Tuberc Lung Dis. 2011;15:1675–9.
Chitnis T, Ness J, Krupp L, Waubant E, Hunt T, Olsen CS, et al. Clinical features of neuromyelitis optica in children: US Network of Pediatric MS Centers report. Neurology. 2016;86:245–52. Available from: /pmc/articles/PMC4733158/?report=abstract. Accessed 22 Jul 2020.
Sütlaş PN, Ünal A, Forta H, Şenol S, Kırbaş D. Tuberculous meningitis in adults: review of 61 cases. Infection. 2003;31:387–91. Available from: http://link.springer.com/10.1007/s15010-003-3179-1. Accessed 23 May 2020.
Ardito F, Posteraro B, Sanguinetti M, Zanetti S, Fadda G. Evaluation of BACTEC Mycobacteria Growth Indicator Tube (MGIT 960) automated system for drug susceptibility testing of Mycobacterium tuberculosis. J Clin Microbiol. 2001;39:4440–4. Available from: https://pubmed.ncbi.nlm.nih.gov/11724858/. Accessed 22 Jul 2020.
Nicolls DJ, King M, Holland D, Bala J, Del, Rio C. Intracranial tuberculomas developing while on therapy for pulmonary tuberculosis. Lancet Infect Dis. 2005;5:795–801.
Sharma SK, Ryan H, Khaparde S, Sachdeva KS, Singh AD, Mohan A, et al. Index-TB guidelines: guidelines on extrapulmonary tuberculosis for India. Indian J Med Res. 2017;145:448–63. Available from: /pmc/articles/PMC5663158/?report=abstract. Accessed 21 Sep 2020.
World Health Organization. Rapid implementation of the Xpert MTB/RIF diagnostic test. Technical and operational ‘How to’ practical considerations. World Health Organization. 2011. p. 1–34. Available from: http://www.who.int/about/licensing/copyright_form/en/index.html. Accessed 21 Sep 2020.
Jakka S, Veena S, Rao ARM, Eisenhut M. Cerebrospinal fluid adenosine deaminase levels and adverse neurological outcome in pediatric tuberculous meningitis. Infection 2005;33:264–6.
Bernaerts A, Vanhoenacker FM, Parizel PM, Van Goethem JWM, van Altena R, Laridon A, et al. Tuberculosis of the central nervous system: overview of neuroradiological findings. Eur Radiol. 2003;13:1876–90.
Clavier E, Thiebot J, Freger P, Mihout B, Bernet J, Benozio M. [Optochiasmatic tuberculoma and MRI. 2 cases]. J Radiol. 1988;69:333–7.
Anupriya A, Sunithi M, Maya T, Goel M, Alexander M, Aaron S, et al. Tuberculous optochiasmatic arachnoiditis. Neurol India. 2010;58:732–5.
Gupta RK, Jobanputra KJ, Yadav A. MR spectroscopy in brain infections. Neuroimaging Clin N Am. 2013;23:475–98. https://doi.org/10.1016/j.nic.2013.03.004.
Kingsley PB, Shah TC, Woldenberg R. Identification of diffuse and focal brain lesions by clinical magnetic resonance spectroscopy. NMR Biomed. 2006;19:435–62. Available from: http://doi.wiley.com/10.1002/nbm.1039. Accessed 23 May 2020.
Morales H, Alfaro D, Martinot C, Fayed N, Gaskill-Shipley M. MR spectroscopy of intracranial tuberculomas: a singlet peak at 3.8 ppm as potential marker to differentiate them from malignant tumors. Neuroradiol J. 2015;28:294–302.
Andronikou S, Smith B, Hatherhill M, Douis H, Wilmshurst J. Definitive neuroradiological diagnostic features of tuberculous meningitis in children. Pediatr Radiol. 2004;34:876–85.
Sharma P, Sharma R. Toxic optic neuropathy. Indian J Ophthalmol. 2011;59:137–41.
Gümüş A, Öner V. Follow up of retinal nerve fiber layer thickness with optic coherence tomography in patients receiving anti-tubercular treatment may reveal early optic neuropathy. Cutan Ocul Toxicol. 2015;34:212–6.
Wang L-J, Chen L-M, Chen Y, Bao L-Y, Zheng N-N, Wang Y-Z, et al. Ultrasonography assessments of optic nerve sheath diameter as a noninvasive and dynamic method of detecting changes in intracranial pressure. JAMA Ophthalmol. 2018;136:250–6.
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A. et al. Executive summary: Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: treatment of drug-susceptible tuberculosis. Clin Infect Dis. 2016;63:853–67. https://doi.org/10.1093/cid/ciw566.
American Academy of Pediatrics. Red book: 2015 report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015.
Thwaites GE, Bang ND, Dung NH, Quy HT, Oanh DTT, Thoa NTC, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004;351:1741–51. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMoa040573. Accessed 23 May 2020.
Nicolls DJ, King M, Holland D, Bala J, Del Rio C. Intracranial tuberculomas developing while on therapy for pulmonary tuberculosis. Lancet Infect Dis. 2005;5:795–801.
Roberts MTM, Mendelson M, Meyer P, Carmichael A, Lever AML. The use of thalidomide in the treatment of intracranial tuberculomas in adults: two case reports. J Infect. 2003;47:251–5.
Schoeman JF, Andronikou S, Stefan DC, Freeman N, Van Toorn R. Tuberculous meningitis-related optic neuritis: recovery of vision with thalidomide in 4 consecutive cases. J Child Neurol. 2010;25:822–8.
Blackmore TK, Manning L, Taylor WJ, Wallis RS. Therapeutic use of infliximab in tuberculosis to control severe paradoxical reaction of the brain and lymph nodes. Clin Infect Dis. 2008;47:e83–5.
Saxena R, Singh D. Tuberculous optic neuropathy. In: Kumar A, Chawla R, Sharma N, editors. Ocular tuberculosis. Essentials in Ophthalmology. Springer, Cham; 2017. p. 95–9. https://doi.org/10.1007/978-3-319-57520-9_10.
Rizvi I, Garg RK, Malhotra HS, Kumar N, Sharma E, Srivastava C. et al. Ventriculoperitoneal shunt surgery for tuberculous meningitis: a systematic review. J Neurol Sci. 2017;375:255–63. Available from: https://pubmed.ncbi.nlm.nih.gov/28320142/. Accessed 8 Feb 2021.
Nadvi SS, Nathoo N, Annamalai K, van Dellen JR, Bhigjee AI. Role of cerebrospinal fluid shunting for human immunodeficiency virus-positive patients with tuberculous meningitis and hydrocephalus. Neurosurgery. 2000;47:644–50–51. Available from: https://pubmed.ncbi.nlm.nih.gov/10981752/. Accessed 8 Feb 2021.
Rajshekhar V. Management of hydrocephalus in patients with tuberculous meningitis. Neurol India. 2009;57:368. Available from: http://www.neurologyindia.com/text.asp?2009/57/4/368/55572. Accessed 8 Feb 2021.
Marcus AO, Demakas JJ, Ross HA, Duick DS, Crowell RM. Optochiasmatic arachnoiditis with treatment by surgical lysis of adhesions, corticosteroids, and cyclophosphamide: report of a case. Neurosurgery 1986;19:101–3.
Navarro IM, Peralta VH, Leon JA, Varela EA, Cabrera JM. Tuberculous optochiasmatic arachnoiditis. Neurosurgery 1981;9:654–60.
Mahadevan B, Mahadevan S, Serane VT. Prognostic factors in childhood tuberculous meningitis. J Trop Pediatr. 2002;48:362–5. https://doi.org/10.1093/tropej/48.6.362.
Acknowledgements
We would like to acknowledge Dr. Saurabh Verma for helping us with the images.
Author information
Authors and Affiliations
Contributions
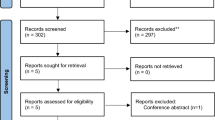
The authors declare that the manuscript has been read and approved by all the authors. RD and SL were responsible for designing the review protocol, writing the protocol and report, conducting the search, screening potentially eligible studies, extracting and analysing data, interpreting results, updating reference lists, creating ‘Summary of findings’ table, critical revision of the article and the final approval of the version. PKP and NH were responsible for writing the protocol and report, screening potentially eligible studies, extracting and analysing data, interpreting results and updating reference lists. SS and RS were responsible for the critical revision of the article and the final approval of the version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dhiman, R., Lakra, S., Panda, P.K. et al. Neuro-ophthalmic manifestations of tuberculosis. Eye 36, 15–28 (2022). https://doi.org/10.1038/s41433-021-01619-6
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01619-6
This article is cited by
-
Optical coherence tomography biomarkers and visual functions in tuberculous meningitis: an observational study
International Ophthalmology (2025)