Abstract
Objectives
To audit the structural and functional outcomes of surgery for acute tractional retinal detachment due to retinopathy or prematurity between 2004 and 2014 in Oxford UK.
Methods
Consecutive operations were identified from a surgical log. Clinical data including demography, perioperative data, and retinal outcomes were extracted into a spreadsheet and compared against two international data sets referenced in the method section. Nonparametric tests (Fisher’s exact, and the Mann–Whitney U-tests) were used for statistical analysis with a p-value < 0.05 considered significant.
Results
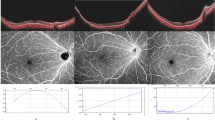
Twenty-nine eyes of 19 babies underwent surgery. The mean age (SD) at final follow-up was 6.4 (3.7) years of age and comparable to the reference data sets. The mean birth weight and gestational age of babies matched the ETROP data set referenced in the method section. Anatomical success was obtained in 16/29 (55.2%) of eyes and more likely with stage 4 ROP than stage 5 disease (p < 0.05). Thirteen of 29 eyes (44.8%) obtained form vision post-operatively. All instances of macular retinal reattachment during follow up were verified with post-operative OCT.
Conclusions
Surgery for stage 5 ROP is not worthwhile. For stage 4 ROP it yielded better visual outcomes than ETROP but registration for visual impairment was not prevented. Innovation such as endoscopic vitrectomy could yield better outcomes. Earlier detection of vitreoretinal fibrosis could result in timelier referral. A formally funded national service is needed to ring-fence resource to avoid delays in access to surgery, which has a narrow surgical window.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Terry T. Fibroblastic overgrowth of persistent tunica vasculosa lentis in infants bom prematurely: II. report of cases-clinical aspects. Trans Am Ophthalmol Soc. 1942;40:262–81.
Aaberg T, Ben-Sira I, Charles S, Clarkson J, Cohen BZ, Flynn J, et al. An international classification of retinopathy of prematurity: II. the classification of retinal detachment. Arch Ophthalmol. 1987;105:906–12.
Palmer M. Retinopathy of prematurity. Arch Ophthalmol. 1988;106:471–9.
Hardy RJ, Good WV, Dobson V, Palmer EA, Tung B, Phelps DL. Early Treatment for Retinopathy of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121:1684–96.
Hansen ED, Hartnett ME. A review of treatment for retinopathy of prematurity. Exp Rev Ophthalmol. 2019;14:73–87.
Repka MX, Tung B, Good WV, Shapiro M, Capone A, Baker JD, et al. Outcome of eyes developing retinal detachment during the early treatment for retinopathy of prematurity study. Arch Ophthalmol. 2011;129:1175–9.
Karacorlu M, Hocaoglu M, Muslubas IS, Arf S. Long-term functional results following vitrectomy for advanced retinopathy of prematurity. Br J Ophthalmol. 2017;101:730–4.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol (Chic, Ill: 1960). 2005;123:991.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Brett J, Smith L, et al. Non-contact ultra-widefield imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye. 2013;27:589–96.
Sonkson PM. The assessment of ‘vision for development’ in severely visually handicapped babies. Acta Ophthalmol. 1983;61:82–90.
Patel CK, Chen SD, Farmery AD. Optical coherence tomography under general anesthesia in a child with nystagmus. Am J Ophthalmol. 2004;137:1127–9.
Fung T, Muqit M, Mordant D, Smith L, Patel C. Modification of spectralis HRA+ OCT for intraoperative multi-modality imaging in pediatric retinal diseases. Investig Ophthalmol Vis Sci. 2013;54:1496–96.
Patel CK. Optical coherence tomography in the management of acute retinopathy of prematurity. Am J Ophthalmol. 2006;141:582–4.
Chen X, Prakalapakorn SG, Freedman SF, Vajzovic L, Toth CA. Differentiating retinal detachment and retinoschisis using handheld optical coherence tomography in stage 4 retinopathy of prematurity. JAMA Ophthalmol. 2020;138:81–5.
Kothari N, Chu A, Huang JM, Lin F, Lin BR, Manoharan N et al. Arm-mounted optical coherence tomography angiography in extremely low birth weight neonates with retinopathy of prematurity. Am J Ophthalmol. 2020; 100624. https://doi.org/10.1016/j.ajoc.2020.100624.
Adams GG, Bunce C, Xing W, Butler L, Long V, Reddy A, et al. Treatment trends for retinopathy of prematurity in the uk: active surveillance study of infants at risk. BMJ Open. 2017;7:e013366.
Yonekawa Y, Wu WC, Nitulescu CE, Chan RP, Thanos A, Thomas BJ, et al. Progressive retinal detachment in infants with retinopathy of prematurity treated with intravitreal bevacizumab or ranibizumab. Retina. 2018;38:1079–83.
Yonekawa Y, Thanos A, Abbey AM, Thomas BJ, Todorich B, Faia LJ, et al. Hybrid 25-and 27-gauge vitrectomy for complex vitreoretinal surgery. Ophthalmic surgery, lasers imaging. Retina. 2016;47:352–5.
Nagiel A, Yang U, Reid MW, Anulao KJ, Say EA, Wong SC, et al. Visual and anatomic outcomes of pediatric endoscopic vitrectomy in 326 cases. Retina. 2020;40:2083–90.
Acknowledgements
The delivery of care for the babies described in this study would not have been possible without contributions from a multidisciplinary team of medical (neontologists, paediatric anaesthetists, vitreoretinal fellows, specialist registrars) and non-medical staff (nurses, orthoptists, optometrists) of the Oxford Eye Hospital and Oxford University. I must acknowledge the help of Professor Andrew Farmery for his airway management expertise that facilitated the initial development of OCT imaging under anaesthesia and the subsequent fund-raising efforts of hospital staff and parents to develop the Spectralis OCT. I am very grateful for the dedication of the imaging team with special thanks extended to Anne Bolton, Lewis Smith and Jon Brett. Ozdemir Ozdemir, a paediatric ophthalmologist from Istanbul was an observer who I would like to thank for some of the data collection to assist with the audit.
Funding
As this work describes an audit of clinical activity in a National Health Setting no funding has been required for the study. The cost of publication of will be met from University of Oxford research funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
No funding was required or provided for this audit. CK Patel has received fees from Optos and Heidelberg engineering for lectures on retinal imaging in children. CK Patel conceived the methodology that was reviewed and modified by contributions from all authors (CKP, EC, RH, SCW, SB), who also participated in the writing and review of the written article. None of the other authors have any conflict of interest to declare relevant to the content of this publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Patel, C.K., Carreras, E., Henderson, R.H. et al. Evolving outcomes of surgery for retinal detachment in retinopathy of prematurity: the need for a national service in the United Kingdom. Eye 36, 1590–1596 (2022). https://doi.org/10.1038/s41433-021-01679-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01679-8