Abstract
Objectives
To describe the features, management approaches, and outcomes of orbito-cranial schwannomas.
Methods
Retrospective review of ten patients with orbito-cranial schwannomas managed in six orbital services over 22 years. Data collected included demographics, presenting features, neuroimaging characteristics, histology, management approach, complications, and outcomes.
Results
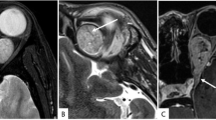
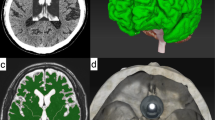
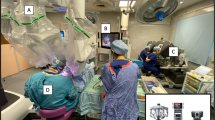
Mean age of the patients was 41.4 ± 19.9 years, and 6 (60%) were females. The majority presented with proptosis (90%), limited extraocular motility (80%), eyelid swelling (60%), and optic neuropathy (60%). Most lesions (80%) involved the entire anterior-posterior span of the orbit, with both intra- and extraconal involvement. All tumours involved the orbital apex, the superior orbital fissure, and extended at least to the cavernous sinus. Surgical resection was performed for all. Seven (70%) of the tumours were completely or subtotally resected combining an intracapsular approach by an orbital-neurosurgical collaboration, with no recurrence on postoperative follow-up (6–186 months). Three underwent tumour debulking. Of these, two remained stable on follow-up (6–34 months) and one showed progression of the residual tumour over 9 years (cellular schwannoma on histology) necessitating stereotactic radiotherapy (SRT) for local control. Adjuncts to the orbito-cranial resection included perioperative frozen section (n = 5), endoscopic transorbital approach (n = 2), and image-guided navigation (n = 1). Post-surgical adjuvant SRT was used in three subjects.
Conclusions
These results highlight the possibility of successful surgical control in complex orbito-cranial schwannomas. A combined neurosurgical/orbital approach with consideration of an intracapsular resection is recommended. Recurrence may not occur with subtotal excision and observation may be reasonable. Adjunctive SRT for progression or residual tumour can be considered.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rose GE, Wright JE. Isolated peripheral nerve sheath tumours of the orbit. Eye 1991;5:668–73.
Pushker N, Khurana S, Kashyap S, Sen S, Shrey D, Meel R, et al. Orbital schwannoma: a clinicopathologic study. Int Ophthalmol. 2015;35:481–6.
Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. Ophthalmol [Internet]. 2004;111:997–1008. https://linkinghub.elsevier.com/retrieve/pii/S0161642003014957
Rootman J, Goldberg C, Robertson W. Primary orbital schwannomas. Br J Ophthalmol [Internet]. 1982;66:194–204. https://bjo.bmj.com/lookup/doi/10.1136/bjo.66.3.194
Yong K-L, Beckman TJ, Cranstoun M, Sullivan TJ. Orbital Schwannoma-Management and Clinical Outcomes. Ophthal Plast Reconstr Surg [Internet]. 2020;36:590–5. http://www.ncbi.nlm.nih.gov/pubmed/32282644
Hamm KD, Gross MW, Fahrig A, Surber G, Henzel M, Kleinert G, et al. Stereotactic radiotherapy for the treatment of nonacoustic schwannomas. Neurosurg [Internet]. 2008;62:A29–36. https://academic.oup.com/neurosurgery/article/62/suppl_5/A29/2558352
Abe M, Kawase T, Urano M, Mizoguchi Y, Kuroda M, Kasahara M, et al. Analyses of proliferative potential in schwannomas. Brain Tumor Pathol [Internet]. 2000;17:35–40. http://link.springer.com/10.1007/BF02478916
Yoshida K, Kawase T. Trigeminal neurinomas extending into multiple fossae: surgical methods and review of the literature. J Neurosurg [Internet] 1999;91:202–11. https://thejns.org/view/journals/j-neurosurg/91/2/article-p202.xml
Samii M, Migliori MM, Tatagiba M, Babu R. Surgical treatment of trigeminal schwannomas. J Neurosurg [Internet]. 1995;82:711–8. https://thejns.org/view/journals/j-neurosurg/82/5/article-p711.xml
Jefferson G. The Trigeminal Neurinomas with Some Remarks on Malignant Invasion of the Gasserian Ganglion. Neurosurg [Internet]. 1955;1:11–54. http://academic.oup.com/neurosurgery/article/1/CN_suppl_1/11/4100295
Zhang L, Yang Y, Xu S, Wang J, Liu Y, Zhu S. Trigeminal schwannomas: a report of 42 cases and review of the relevant surgical approaches. Clin Neurol Neurosurg [Internet]. 2009;111:261–9. https://linkinghub.elsevier.com/retrieve/pii/S0303846708003831
Wanibuchi M, Fukushima T, Zomordi AR, Nonaka Y, Friedman AH. Trigeminal Schwannomas: Skull Base Approaches and Operative Results in 105 Patients. Oper Neurosurg [Internet]. 2012;70:ons132–44. https://academic.oup.com/ons/article/70/suppl_1/ons132/2408529
Schick U, Bleyen J, Hassler W. Treatment of orbital schwannomas and neurofibromas. Br J Neurosurg [Internet]. 2003;17:541–5. http://www.tandfonline.com/doi/full/10.1080/02688690310001627786
Kron M, Bohnsack BL, Archer SM, McHugh JB, Kahana A. Recurrent orbital schwannomas: clinical course and histopathologic correlation. BMC Ophthalmol [Internet]. 2012;12:44. http://bmcophthalmol.biomedcentral.com/articles/10.1186/1471-2415-12-44
Dervin JE, Beaconsfield M, Wright JE, Moseley IF. CT findings in orbital tumours of nerve sheath origin. Clin Radio [Internet]. 1989;40:475–9. https://linkinghub.elsevier.com/retrieve/pii/S0009926089802508
Cantore G, Ciappetta P, Raco A, Lunardi P. Orbital Schwannomas: Report of Nine Cases and Review of the Literature. Neurosurg [Internet]. 1986;19:583–8. https://academic.oup.com/neurosurgery/article/19/4/583/2745519
Shields JA, Kapustiak J, Arbizo V, Augsburger JJ, Schnitzer RE. Orbital Neurilemoma With Extension Through the Superior Orbital Fissure. Arch Ophthalmol [Internet]. 1986;104:871–3. http://archopht.jamanetwork.com/article.aspx?articleid=636090
Chen MH, Yan JH. Imaging characteristics and surgical management of orbital neurilemmomas. Int J Ophthalmol [Internet]. 2019;12:1108–15. http://www.ijo.cn/gjyken/ch/reader/view_abstract.aspx?file_no=20190709&flag=1
Al-Mefty O, Ayoubi S, Gaber E. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcomes of cranial nerve function. J Neurosurg [Internet]. 2002;96:453–63. https://thejns.org/view/journals/j-neurosurg/96/3/article-p453.xml
Konovalov AN, Spallone A, Mukhamedjanov DJ, Tcherekajev VA, Makhmudov UB. Trigeminal neurinomas a series of 111 surgical cases from a single institution. Acta Neurochir (Wien) [Internet]. 1996;138:1027–35. http://link.springer.com/10.1007/BF01412304
Kauser H, Rashid O, Anwar W, Khan S. Orbital oculomotor nerve schwannoma extending to the cavernous sinus: a rare cause of proptosis. J Ophthalmic Vis Res [Internet]. 2014;9:514. http://www.jovr.org/text.asp?2014/9/4/514/150833
Park HH, Hong SD, Kim YH, Hong C-K, Woo KI, Yun I-S, et al. Endoscopic transorbital and endonasal approach for trigeminal schwannomas: a retrospective multicenter analysis (KOSEN-005). J Neurosurg [Internet]. 2020;133:467–76. https://thejns.org/view/journals/j-neurosurg/133/2/article-p467.xml
Kong D-S, Young SM, Hong C-K, Kim Y-D, Hong SD, Choi JW, et al. Clinical and ophthalmological outcome of endoscopic transorbital surgery for cranioorbital tumors. J Neurosurg [Internet]. 2019;131:667–75. https://thejns.org/view/journals/j-neurosurg/131/3/article-p667.xml
Zabel A, Thilmann C, Schlegel W, Wannenmacher M. Management of benign cranial nonacoustic schwannomas by fractionated stereotactic radiotherapy. Int J Cancer [Internet]. 2001;96:356. http://doi.wiley.com/10.1002/ijc.1036
Kharod SM, Herman MP, Amdur RJ, Mendenhall WM. Fractionated Radiation Therapy for Benign Nonacoustic Schwannomas. Am J Clin Oncol [Internet]. 2018;41:13–7. https://journals.lww.com/00000421-201801000-00003
Goh ASC, Kim YD, Woo KI, Lee J-Il. Benign orbital apex tumors treated with multisession gamma knife radiosurgery. Ophthalmol [Internet]. 2013;120:635–41. https://linkinghub.elsevier.com/retrieve/pii/S0161642012007865
Author information
Authors and Affiliations
Contributions
YS: analysis and interpretation of data, drafting of paper and critical revision. VJ: conception or design of the work, acquisition of data, and critical revision. TD: conception or design of the work, acquisition of data, and critical revision. AH: conception or design of the work, acquisition of data, and critical revision. DM: conception or design of the work, acquisition of data, and critical revision. AW: conception or design of the work, acquisition of data, and critical revision. AY: conception or design of the work, acquisition of data, and critical revision. PS: conception or design of the work, acquisition of data, and critical revision. KIW: conception or design of the work, acquisition of data, and critical revision. TH: conception or design of the work, acquisition of data, and critical revision. BP: conception or design of the work, acquisition of data, and critical revision. KD: conception or design of the work, acquisition of data, and critical revision. DS: conception or design of the work, analysis and interpretation of data, and critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shapira, Y., Juniat, V., Dave, T. et al. Orbito-cranial schwannoma—a multicentre experience. Eye 37, 48–53 (2023). https://doi.org/10.1038/s41433-021-01850-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01850-1