Abstract
Purpose
To describe clinical characteristics and visual outcomes of non-traumatic open globe injuries.
Setting
A level 1 trauma centre in a large urban medical centre.
Design
Retrospective study.
Methods
Charts of non-traumatic open globe patients admitted to MHH-TMC from 1/2010 to 3/2015 were reviewed for demographics, cause, clinical characteristics, visual acuity (VA) and enucleation.
Results
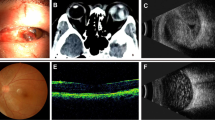
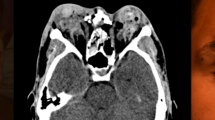
Thirty eyes were included: 15 (50%) were males with a mean age of 47 (±28) years. All presented with zone 1 injury. Twenty-five (83%) had a perforated corneal ulcer. Presenting VA was count fingers (n = 3, 10%) to NLP (n = 6, 20%). Twenty-four (80%) involved infection, 5 (17%) congenital, 3 (10%) chemical burn and 2 (7%) neurotrophic. Conjunctival injection (n = 22, 77%), corneal opacification (n = 20, 71%) and relative afferent pupillary defect (n = 9, 44%) were common. After treatment, 23 (88%) were worse than 6/60 (20/200), 9 (35%) were NLP and 8 (27%) required enucleation.
Conclusions
Often non-traumatic open globe injuries are zone 1 and due to perforated infectious ulcers. Compared to previously reported traumatic injuries, these have higher rates of enucleation (27% vs 8%) and poorer final VA (88% vs 68% worse than 6/60 20/200).
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002;15:139–43.
Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3.
Mansouri M, Faghihi H, Hajizadeh F, Rasoulinejad S, Rajabi M, Tabatabaey A. et al. Epidemiology of open-globe injuries in Iran: analysis of 2,340 cases in 5 years (Report No. 1). Retina. 2009;29:1141–9.
Parver LM, Dannenberg AL, Blacklow B, Fowler CJ, Brechner RJ, Tielsch JM. Characteristics and causes of penetrating eye injuries reported to the National Eye Trauma System Registry, 1985-9. Public Health Rep. 1993;108:625–32.
Casson RJ, Walker JC, Newland HS. Four-year review of open eye injuries at the Royal Adelaide Hospital. Clin Exp Ophthalmol. 2002;30:15–18.
Fujikawa A, Mohamed YH, Kinoshita H, Matsumoto M, Uematsu M, Tsuiki E, et al. Visual outcomes and prognostic factors in open-globe injuries. BMC Ophthalmol. 2018;18:138.
Lekskul M, Fracht HU, Cohen EJ, Rapuano CJ, Laibson PR. Nontraumatic corneal perforation. Cornea. 2000;19:313–9.
Sahin Atik S, Ugurlu S, Egrilmez ED. Open globe injury: demographic and clinical features. J Craniofac Surg. 2018;29:628–31.
Rao L, Ninan A, Rao K. Descriptive study on ocular survival, visual outcome and prognostic factors in open globe injuries. Indian J Ophthalmol. 2010;58:321.
Pieramici DJ, MacCumber MW, Humayun MU, Marsh MJ, de Juan E. Open-globe Injury. Ophthalmology. 1996;103:1798–803.
Yalcin Tök O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71:1794–1800.
Kent C. Winning the battle against corneal ulcers. Rev Ophthalmol. 2013. https://www.reviewofophthalmology.com/article/winning-the-battle-against-corneal-ulcers-42796. Accessed June 27, 2019.
Singh P, Tyagi M, Kumar Y, Gupta KK, Sharma PD. Ocular chemical injuries and their management. Oman J Ophthalmol. 2013;6:83–6.
Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton M. Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005;59:175–8.
Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–41.
Shah A, Sachdev A, Coggon D, Hossain P. Geographic variations in microbial keratitis: an analysis of the peer-reviewed literature. Br J Ophthalmol. 2011;95:762–7.
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis. Ophthalmology. 2006;113:109–16.
Wong TY, Ng TP, Fong KS, Tan DT. Risk factors and clinical outcomes between fungal and bacterial keratitis: a comparative study. CLAO J. 1997;23:275–81.
Funding
This work was supported in part by National Eye Institution Vision Core Grant P30EY028102 and Research to Prevent Blindness. Funding sources were not involved in collection, analysis or collection of data, or writing of this manuscript.
Author information
Authors and Affiliations
Contributions
AWG collected data and wrote first drafts of the manuscript. ELC contributed to the conception and review of the article. JZF, MLP, AZC, KR, and ELC edited subsequent drafts and revisions. AZC additionally contributed to data analysis. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gross, A.W., Fan, J.Z., Pfeiffer, M.L. et al. Non-traumatic open globe injuries: presenting characteristics and visual outcomes. Eye 36, 2323–2327 (2022). https://doi.org/10.1038/s41433-021-01869-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-021-01869-4
This article is cited by
-
Outpatient visits and secondary surgeries following open globe injuries: a single institution retrospective analysis
International Ophthalmology (2026)