Abstract
Objectives
To develop and implement a simulation-based training model for the management of posterior capsule rupture (PCR) from a non-technical skills (NTS) perspective, and analyse changes in participant’s NTS and technical skills (TS).
Methods
The simulation-based training model consisted of two identical PCR simulations with NTS stressors applied, separated by a predominantly NTS focussed training intervention. Participants’ TS and NTS were evaluated by two blinded assessors using the Objective Structured Assessment of Technical Skill (OSATS) global rating scale and the HUman Factors in intraoperative Ophthalmic Emergencies Scoring System (HUFOES) respectively. Paired t-tests were used to establish the difference in mean HUFOES and OSATS scores between initial and repeat simulations; p < 0.05 indicated statistical significance. McGaghie’s model of translational outcomes for simulation-based learning was used to establish the simulation model’s educational status.
Results
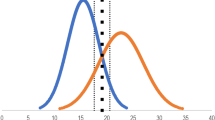
Seventeen cataract surgeons of varying training grades participated in the simulation-based training model. NTS improved with statistical significance; mean HUFOES scores increased from 48.7 ± 16.6 to 59.2 ± 14.8 (p < 0.001). Mean OSATS scores increased without statistical significance from 16.0 ± 7.3 to 17.9 ± 8.3 (p = 0.07). This simulation model achieved Level 1 (internal acceptability) and Level 2 (contained effects) according to McGaghie’s model.
Conclusions
This novel simulation-based training model was designed to improve the NTS required for managing intraoperative PCR, through the provision of an interactive training session. Statistically significant improvements in participants’ NTS in combination with statistically insignificant improvements in TS demonstrate that the simulation-based training model has specificity within the NTS domain.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Chan E, Mahroo OAR, Spalton DJ. Complications of cataract surgery. Clin Exp Optom. 2010;93:379–89.
Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, Galloway P, et al. The Cataract National Dataset electronic multi-centre audit of 55 567 operations: updating benchmark standards of care in the United Kingdom and internationally. Eye. 2009;23:38–49.
Ionides A, Minassian D, Tuft S. Visual outcome following posterior capsule rupture during cataract surgery. Br J Ophthalmol. 2001;85:222–4.
Turnbull AMJ, Lash SC. Confidence of ophthalmology specialist trainees in the management of posterior capsule rupture and vitreous loss. Eye. 2016;30:943–8.
Zevin B, Levy JS, Satava RM, Grantcharov TP. A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg. 2012;215:580–6.
Thomsen ASS, Subhi Y, Kiilgaard JF, la Cour M, Konge L. Update on simulation-based surgical training and assessment in ophthalmology: a systematic review. Ophthalmology. 2015;122:1111–30.
Lee R, Raison N, Lau WY, Aydin A, Dasgupta P, Ahmed K, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye. 2020;34:1737–59.
Pena G, Altree M, Field J, Sainsbury D, Babidge W, Hewett P, et al. Nontechnical skills training for the operating room: a prospective study using simulation and didactic workshop. Surgery. 2015;158:300–9.
Brunckhorst O, Khan MS, Dasgupta P, Ahmed K. Nontechnical skill training and the use of scenarios in modern surgical education. Curr Opin Urol. 2017;27:330–6.
Saleh GM, Wawrzynski JR, Saha K, Smith P, Flanagan D, Hingorani M, et al. Feasibility of human factors immersive simulation training in ophthalmology the london pilot. JAMA Ophthalmol. 2016;134:905–11.
Brunckhorst O, Shahid S, Aydin A, Khan S, McIlhenny C, Brewin J, et al. The relationship between technical and nontechnical skills within a simulation-based ureteroscopy training environment. J Surgical Educ. 2015;72:1039–44.
Wood TC, Maqsood S, Nanavaty MA, Rajak S. Validity of scoring systems for the assessment of technical and non-technical skills in ophthalmic surgery—a systematic review. Eye. 2021;35:1833–49.
Wood TC, Maqsood S, Zoutewelle S, Nanavaty MA, Rajak S. Development of the HUman Factors in intraoperative Ophthalmic Emergencies Scoring System (HUFOES) for non-technical skills in cataract surgery. Eye. 2021;35:616–24.
Kelly SP, Steeples LR, Smith R, Azuara-Blanco A. Surgical checklist for cataract surgery: progress with the initiative by the Royal College of Ophthalmologists to improve patient safety. Eye. 2013;27:878–82.
Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. J Br Surg. 1997;84:273–8.
McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. 2014;48:375–85.
Kao LS, Thomas EJ. Navigating towards improved surgical safety using aviation-based strategies. J Surgical Res. 2008;145:327–35.
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R. The impact of stress on surgical performance: a systematic review of the literature. Surgery. 2010;147:318–30.
Hassan I, Weyers P, Maschuw K, Dick B, Gerdes B, Rothmund M, et al. Negative stress-coping strategies among novices in surgery correlate with poor virtual laparoscopic performance. J Br Surg. 2006;93:1554–9.
Azuara-Blanco A, Reddy A, Wilkinson G, Flin R. Safe eye surgery: non-technical aspects. Eye. 2011;25:1109–11.
Brunckhorst O, Shahid S, Aydin A, McIlhenny C, Khan S, Raza SJ, et al. Simulation-based ureteroscopy skills training curriculum with integration of technical and non-technical skills: a randomised controlled trial. Surgical Endosc. 2015;29:2728–35.
Staropoli PC, Gregori NZ, Junk AK, Galor A, Goldhardt R, Goldhagen BE, et al. Surgical simulation training reduces intraoperative cataract surgery complications among residents. Simul Healthc: J Soc Simul Healthc. 2018;13:11.
Henderson BA, Kim JY, Golnik KC, Oetting TA, Lee AG, Volpe NJ, et al. Evaluation of the virtual mentor cataract training program. Ophthalmology. 2010;117:253–8.
Isreb S, Attwood SE. The fallacy of comparing surgeons with pilots in the search for safer surgical training. J Br Surg. 2011;98:467–8.
Sommer K. Pilot training: what can surgeons learn from it? Arab J Urol. 2014;12:32–5.
Wood TC, Maqsood S, Sancha W, Nanavaty MA, Rajak S. Comparisons between cataract surgery and aviation. Eye. 2022:1–2.
Yorston D, Duncalfe M. Managing emergencies: lessons from aviation. Community Eye Health. 2018;31:58–9.
Singh A, Strauss GH. High-fidelity cataract surgery simulation and third world blindness. Surgical Innov. 2015;22:189–93.
Acknowledgements
The authors would like to thank the Simulation department at the University Hospitals Sussex (UHSussex) NHS Trust for helping with the semantics of the simulation. The authors are also grateful to: Theatre staff: Jenny Brookes, Vasiliki Xenaki, Chris Tully, Letizia Buccoliero, Tina McMilan, Regis Chaco, Myrna McHarg and Philip Harris. Consultants: Edward Hughes, Dominic Heath. Trainees: Hasan Naveed, Simerdeep Kaur, Hanbin Lee, Christopher Holmes, Ahmed Roble, Vidushi Golash, Patrick Idam, Jamal Sawan, Radhika Dashputra, Huw Oliphant, Tristian Mann, Gabriela Ortiz, Krystian Kyza. Management: Emma Goudman, Alex Shaw, Jane McNevin, and Neil Vine.
Author information
Authors and Affiliations
Contributions
TCW contributed to the study’s concept and design, data acquisition and statistical analysis, drafting and revision of the manuscript, administrative and technical support throughout the study, and final approval of the manuscript. SM contributed to the study’s concept and design, data acquisition and statistical analysis, drafting and revision of the manuscript, administrative and technical support throughout the study, provided regular supervision, and approved the final manuscript. AS contributed to the study’s concept and design, data acquisition, revision of the manuscript, administrative and technical support throughout the study, provided regular supervision, and approved the final manuscript. WS contributed to the study’s concept and design, revision of the manuscript, administrative and technical support throughout the study, provided regular supervision, and approved the final manuscript. MAN contributed to the study’s concept and design, data analysis, drafting and revision of the manuscript, administrative and technical support throughout the study, provided regular supervision, and approved the final manuscript. MW contributed to data acquisition, drafting and revision of the manuscript, technical support throughout the study, provided supervision, and approved the final manuscript. SR contributed to the study’s concept and design, data acquisition and statistical analysis, drafting and revision of the manuscript, administrative and technical support throughout the study, provided regular supervision, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
None of the authors have any financial interest in any product or procedures mentioned in this manuscript. Other disclosures are as follows: TCW, SM, AS, WS, MW and SR: none. MAN: research grants from Alcon Laboratories, USA; European Society of Cataract and Refractive Surgery; Johnson & Johnson, USA; Rayner Intraocular lenses, UK. Lecture fees from Alcon Laboratories, USA. Consultant to Hoya. Travel grant from Alcon Laboratories, USA & Bausch & Lomb, USA.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wood, T.C., Maqsood, S., Saunders, A. et al. Non-technical skills simulation-based training model for managing intraoperative posterior capsule rupture during cataract surgery. Eye 37, 474–479 (2023). https://doi.org/10.1038/s41433-022-01962-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-01962-2
This article is cited by
-
Beyond the microscope: embracing soft skills in ophthalmology for enhanced patient care and clinician well-being
Eye (2024)
-
Simulation-based training for intraoperative posterior capsule rupture management: an analysis of nontechnical skills development and the relationship between technical and nontechnical skills
Eye (2024)