Abstract
Background/Objectives
Although it has been reported that thyroid-stimulating immunoglobulin (TSI) is associated with the clinical characteristics of thyroid eye disease (TED), there is a paucity of literature regarding the role of TSI in diagnosing active TED. This study investigated the relationship between the level of TSI and the activity of TED and assessed the cut-off value of TSI discriminating active TED from inactive TED.
Methods
This cross-sectional study included 101 patients with TED. TSI was quantitatively measured with a cell-based bioassay using a chimeric TSH receptor and a cyclic adenosine monophosphate response element-dependent luciferase. The association between TSI and a variety of demographic and clinical features of TED was analysed. Multivariate regression analysis was performed to determine possible independent factors affecting the level of TSI.
Results
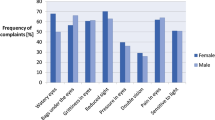
TSI level was higher in males than in females (p = 0.023) and smokers than in nonsmokers (p = 0.004). TSI level was inversely correlated with the duration of ocular symptoms (r = −0.295, p = 0.003). The level of TSI was also significantly different when compared to the thyroid function (p = 0.003), TED activity (p < 0.001), and TED severity (p = 0.001). Multivariate regression analysis revealed a significant relationship between TED activity and thyroid function jointly and the TSI level. The cut-off level of TSI for predicting active TED was a specimen-to-reference ratio of 406.7 (p < 0.001, area under the curve = 0.847, sensitivity 77.4%, specificity 81.3%).
Conclusions
TSI was a functional biomarker strongly associated with TED activity even after being adjusted by other clinical characteristics. Serum TSI level may help identify patients with active TED in clinics.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Li Z, Cestari DM, Fortin E. Thyroid eye disease: what is new to know? Curr Opin Ophthalmol. 2018;29:528–34.
Gerding MN, Terwee CB, Dekker FW, Koornneef L, Prummel MF, Wiersinga WM. Quality of life in patients with Graves’ ophthalmopathy is markedly decreased: measurement by the medical outcomes study instrument. Thyroid. 1997;7:885–9.
Bahn RS. Graves’ ophthalmopathy. N. Engl J Med. 2010;362:726–38.
Khong JJ, McNab AA, Ebeling PR, Craig JE, Selva D. Pathogenesis of thyroid eye disease: review and update on molecular mechanisms. Br J Ophthalmol. 2016;100:142–50.
McLachlan SM, Rapoport B. Breaking tolerance to thyroid antigens: changing concepts in thyroid autoimmunity. Endocr Rev. 2014;35:59–105.
Douglas RS, Afifiyan NF, Hwang CJ, Chong K, Haider U, Richards P, et al. Increased generation of fibrocytes in thyroid-associated ophthalmopathy. J Clin Endocrinol Metab. 2010;95:430–8.
Bahn RS, Dutton CM, Joba W, Heufelder AE. Thyrotropin receptor expression in cultured Graves’ orbital preadipocyte fibroblasts is stimulated by thyrotropin. Thyroid. 1998;8:193–6.
Morris JC 3rd, Hay ID, Nelson RE, Jiang NS. Clinical utility of thyrotropin-receptor antibody assays: comparison of radioreceptor and bioassay methods. Mayo Clin Proc. 1988;63:707–17.
Gupta MK. Thyrotropin receptor antibodies: advances and importance of detection techniques in thyroid diseases. Clin Biochem. 1992;25:193–9.
Lytton SD, Li Y, Olivo PD, Kohn LD, Kahaly GJ. Novel chimeric thyroid-stimulating hormone-receptor bioassay for thyroid-stimulating immunoglobulins. Clin Exp Immunol. 2010;162:438–46.
Ponto KA, Kanitz M, Olivo PD, Pitz S, Pfeiffer N, Kahaly GJ. Clinical relevance of thyroid-stimulating immunoglobulins in graves’ ophthalmopathy. Ophthalmology. 2011;118:2279–85.
Jang SY, Shin DY, Lee EJ, Choi YJ, Lee SY, Yoon JS. Correlation between TSH receptor antibody assays and clinical manifestations of Graves’ orbitopathy. Yonsei Med J. 2013;54:1033–9.
Kampmann E, Diana T, Kanitz M, Hoppe D, Kahaly GJ. Thyroid Stimulating but Not Blocking Autoantibodies Are Highly Prevalent in Severe and Active Thyroid-Associated Orbitopathy: A Prospective Study. Int J Endocrinol. 2015;2015:678194.
Ponto KA, Diana T, Binder H, Matheis N, Pitz S, Pfeiffer N, et al. Thyroid-stimulating immunoglobulins indicate the onset of dysthyroid optic neuropathy. J endocrinological Investig. 2015;38:769–77.
Takakura A, Kirkeby K, Earle K, Silkiss RZ. Predicting the Development of Orbitopathy in Graves Thyroidopathy Patients: The Potential Role of TSI Testing. Ophthalmic Plast Reconstructive Surg. 2015;31:369–72.
Diana T, Kahaly GJ. Thyroid Stimulating Hormone Receptor Antibodies in Thyroid Eye Disease-Methodology and Clinical Applications. Ophthalmic Plast Reconstructive Surg. 2018;34:S13–s19.
Seo S, Sánchez Robledo M. Usefulness of TSH receptor antibodies as biomarkers for Graves’ ophthalmopathy: a systematic review. J Endocrinol Investig. 2018;41:1457–68.
Roos JCP, Paulpandian V, Murthy R. Serial TSH-receptor antibody levels to guide the management of thyroid eye disease: the impact of smoking, immunosuppression, radio-iodine, and thyroidectomy. Eye. 2019;33:212–7.
Bartley GB, Gorman CA. Diagnostic criteria for Graves’ ophthalmopathy. Am J Ophthalmol. 1995;119:792–5.
Jang SY, Lee SY, Lee EJ, Yoon JS. Clinical features of thyroid-associated ophthalmopathy in clinically euthyroid Korean patients. Eye. 2012;26:1263–9.
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L. Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin Endocrinol. 1997;47:9–14.
Bartalena L, Baldeschi L, Dickinson A, Eckstein A, Kendall-Taylor P, Marcocci C, et al. Consensus statement of the European Group on Graves’ orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol. 2008;158:273–85.
Lytton SD, Ponto KA, Kanitz M, Matheis N, Kohn LD, Kahaly GJ. A novel thyroid stimulating immunoglobulin bioassay is a functional indicator of activity and severity of Graves’ orbitopathy. J Clin Endocrinol Metab. 2010;95:2123–31.
Lytton SD, Schluter A, Banga PJ. Functional diagnostics for thyrotropin hormone receptor autoantibodies: bioassays prevail over binding assays. Front Biosci. 2018;23:2028–43.
Perez-Moreiras JV, Gomez-Reino JJ, Maneiro JR, Perez-Pampin E, Romo Lopez A, Rodríguez, et al. Efficacy of Tocilizumab in Patients With Moderate-to-Severe Corticosteroid-Resistant Graves Orbitopathy: A Randomized Clinical Trial. Am J Ophthalmol. 2018;195:181–90.
Dolman PJ. Grading Severity and Activity in Thyroid Eye Disease. Ophthalmic Plast Reconstructive Surg. 2018;34:S34–s40.
Kahaly GJ, Diana T, Glang J, Kanitz M, Pitz S, König J. Thyroid Stimulating Antibodies Are Highly Prevalent in Hashimoto’s Thyroiditis and Associated Orbitopathy. J Clin Endocrinol Metab. 2016;101:1998–2004.
Woo YJ, Jang SY, Lim TH, Yoon JS. Clinical Association of Thyroid Stimulating Hormone Receptor Antibody Levels with Disease Severity in the Chronic Inactive Stage of Graves’ Orbitopathy. Korean J Ophthalmol. 2015;29:213–9.
Suzuki N, Noh JY, Kameda T, Yoshihara A, Ohye H, Suzuki M, et al. Clinical course of thyroid function and thyroid associated-ophthalmopathy in patients with euthyroid Graves’ disease. Clin Ophthalmol. 2018;12:739–46.
Jang SY, Shin DY, Lee EJ, Lee SY, Yoon JS. Relevance of TSH-receptor antibody levels in predicting disease course in Graves’ orbitopathy: comparison of the third-generation TBII assay and Mc4-TSI bioassay. Eye. 2013;27:964–71.
Acknowledgements
The statistical analysis used in this manuscript was supported by Division of Biostatistics, Hallym Institute for Clinical Medicine of Hallym University Medical Center.
Funding
This research was supported by the National Research Foundation of Korea (NRF): 2019R1G1A1100257.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception of the study, data analysis, revision of the manuscript and approval of the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jeon, H., Lee, J.Y., Kim, Y.J. et al. Clinical relevance of thyroid-stimulating immunoglobulin as a biomarker of the activity of thyroid eye disease. Eye 37, 543–547 (2023). https://doi.org/10.1038/s41433-022-01981-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-01981-z