Abstract
Background/Objectives
To study the development, evolution, outcomes, and prognostic factors of lamellar macular hole (LMH) in highly myopic (HM) patients.
Methods
Fifty eyes from 47 HM patients with LMHs were retrospectively enrolled. Relevant pre- and post-LMH optical coherence tomography findings and visual acuity were collected. Structural progression was defined as an increase in the height of retinoschisis, and the development of foveal detachment, full-thickness macular hole, or retinal detachment.
Results
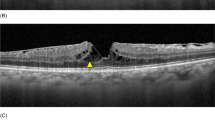
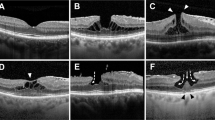
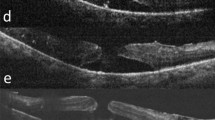
Four traction-related developmental processes were identified. Type 1 LMHs (8, 16%) developed from foveal avulsion caused by vitreomacular traction. Type 2 (32, 64%) and type 3 LMHs (5, 10%) formed from ruptured parafoveal and central foveal cysts, respectively. Progressive foveal thinning caused by epiretinal membranes (ERMs) without cystic changes led to type 4 LMHs (5, 10%). Retinoschisis developed before (9 eyes), after (10 eyes), or simultaneously with (6 eyes) the LMH formation. Structural progression was noted in 50%, 53%, 0%, 100% of patients with type 1–4 LMHs, respectively. Multivariable Cox proportional hazard model showed that greater residual foveal thickness (P = 0.001, adjusted odds ratio = 0.22, 95% confidence interval [CI], 0.08 ~ 0.56), and the absence of retinoschisis were protective against structural progression. Multivariable linear regression showed that poor baseline visual acuity (P < 0.001, β = 0.74, 95% CI 0.41 ~ 1.07) and type 4 LMH predicted worse visual outcomes.
Conclusions
Four traction-related LMH developmental processes were observed in HM eyes and exhibited different evolution and outcomes. LMHs with foveal thinning induced by ERMs had the worst outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The data are available upon reasonable request.
References
Frisina R, Pilotto E, Midena E. Lamellar macular hole: State of the art. Ophthalmic Res. 2019;61:73–82.
Witkin AJ, Ko TH, Fujimoto JG, Schuman JS, Baumal CR, Rogers AH, et al. Redefining lamellar holes and the vitreomacular interface: An ultrahigh-resolution optical coherence tomography study. Ophthalmology. 2006;113:388–97.
Hubschman JP, Govetto A, Spaide RF, Schumann R, Steel D, Figueroa MS, et al. Optical coherence tomography-based consensus definition for lamellar macular hole. Br J Ophthalmol. 2020;104:1741–7.
Tanaka Y, Shimada N, Moriyama M, Hayashi K, Yoshida T, Tokoro T, et al. Natural history of lamellar macular holes in highly myopic eyes. Am J Ophthalmol. 2011;152:96–99.e91.
Lai TT, Yang CM. Lamellar hole-associated epiretinal proliferation in lamellar macular hole and full-thickness macular hole in high myopia. Retina. 2018;38:1316–23.
Rino F, Elena Z, Ivan M, Paolo B, Barbara P, Federica R. Lamellar macular hole in high myopic eyes with posterior staphyloma: Morphological and functional characteristics. Graefes Arch Clin Exp Ophthalmol. 2016;254:2141–50.
Haritoglou C, Tadayoni R, Hubschman JP. Lamellar macular hole surgery - current concepts, future prospects. Clin Ophthalmol. 2019;13:143–6.
Danielescu C, Stanca HT, Balta F. The management of lamellar macular holes: A review. J Ophthalmol. 2020. https://doi.org/10.1155/2020/3526316.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611–9.
Govetto A, Dacquay Y, Farajzadeh M, Platner E, Hirabayashi K, Hosseini H, et al. Lamellar macular hole: Two distinct clinical entities? Am J Ophthalmol. 2016;164:99–109.
Hattori K, Kataoka K, Takeuchi J, Ito Y, Terasaki H. Predictive factors of surgical outcomes in vitrectomy for myopic traction maculopathy. Retina. 2018;38:s23–s30.
Lin CW, Ho TC, Yang CM. The development and evolution of full thickness macular hole in highly myopic eyes. Eye (Lond). 2015;29:388–96.
dell’Omo R, Virgili G, Bottoni F, Parolini B, De Turris S, Di, et al. Lamellar macular holes in the eyes with pathological myopia. Graefes Arch Clin Exp Ophthalmol. 2018;256:1281–90.
Hsia Y, Ho TC, Yang CH, Hsieh YT, Lai TT, Yang CM. Clinical characteristics and long-term evolution of lamellar macular hole in high myopia. PLoS One. 2020;15:e0232852.
Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156:948–.e941.
Bottoni F, Deiro AP, Giani A, Orini C, Cigada M, Staurenghi G. The natural history of lamellar macular holes: A spectral domain optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol. 2013;251:467–75.
Takahashi H, Tanaka N, Shinohara K, Yokoi T, Yoshida T, Uramoto K, et al. Ultra-widefield optical coherence tomographic imaging of posterior vitreous in eyes with high myopia. Am J Ophthalmol. 2019;206:102–12.
Hayashi K, Manabe SI, Hirata A, Yoshimura K. Posterior vitreous detachment in highly myopic patients. Invest Ophthalmol Vis Sci. 2020;61:33.
Koh V, Cheung CY, Wong WL, Cheung CM, Wang JJ, Mitchell P, et al. Prevalence and risk factors of epiretinal membrane in Asian Indians. Invest Ophthalmol Vis Sci. 2012;53:1018–22.
Pang CE, Spaide RF, Freund KB. Comparing functional and morphologic characteristics of lamellar macular holes with and without lamellar hole-associated epiretinal proliferation. Retina. 2015;35:720–6.
Pang CE, Spaide RF, Freund KB. Epiretinal proliferation seen in association with lamellar macular holes: A distinct clinical entity. Retina. 2014;34:1513–23.
Pang CE, Maberley DA, Freund KB, White VA, Rasmussen S, To E, et al. Lamellar hole-associated epiretinal proliferation: A clinicopathologic correlation. Retina. 2016;36:1408–12.
Parolini B, Palmieri M, Finzi A, Besozzi G, Lucente A, Nava U. et al. The new myopic traction maculopathy staging system. Eur J Ophthalmol.2020. https://doi.org/10.1177/1120672120930590.
Bringmann A, Unterlauft JD, Wiedemann R, Barth T, Rehak M, Wiedemann P. Degenerative lamellar macular holes: Tractional development and morphological alterations. Int Ophthalmol. 2021;41:1203–21.
Compera D, Cereda MG, Schumann RG, Bottoni F. Development and progression of a lamellar macular hole with lamellar hole-associated epiretinal proliferation. Retin Cases Brief Rep. 2019;13:371–5.
Author information
Authors and Affiliations
Contributions
Design and implantation of the study (YH, CYL, CMY); Collection of the data (YH, CYL, TCH, CHY, CMY); Collection, management, analysis, and interpretation of the data (YH, CYL, CMY); Drafting of the manuscript (YH); Review, revise, and approval of the manuscript (YH, CYL, TCH, CHY, CMY).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsia, Y., Lee, CY., Ho, TC. et al. The development and evolution of lamellar macular hole in highly myopic eyes. Eye 37, 1170–1177 (2023). https://doi.org/10.1038/s41433-022-02086-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-022-02086-3
This article is cited by
-
Myopic traction maculopathy in fovea-involved myopic chorioretinal atrophy
Eye (2024)
-
Lamellar macular hole in highly myopic eyes and insights into its development, evolution, and treatment: a mini-review
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Vitreoretinal Interface Changes After Anti-vascular Endothelial Growth Factor Treatment in Highly Myopic Eyes: A Real-World Study
Ophthalmology and Therapy (2023)
-
Correction: Formation and evolution of idiopathic lamellar macular hole-a pilot study
BMC Ophthalmology (2022)
-
Formation and evolution of idiopathic lamellar macular hole-a pilot study
BMC Ophthalmology (2022)