Abstract
Purpose
To evaluate factors associated with the diagnosis of open-angle glaucoma (OAG) after a retinal vein occlusion (RVO).
Design
Retrospective, cross-sectional study.
Methods
Patients diagnosed with OAG after RVO were matched 2:1 with RVO patients without prior glaucoma. Logistic regression identified factors linked to OAG diagnosis.
Results
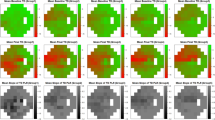
Of 1178 RVO patients without initial OAG, 51 (4.5%) were later diagnosed with OAG after an average of 5.5 ± 6.1 years. Screening tests for OAG were performed at a higher frequency in patients diagnosed with OAG compared with patients who never received this diagnosis (visual field [VF] testing 21.6% versus 10.8% (P = 0.073) and retinal nerve fiber layer [RNFL] imaging 52.9% versus 27.4% (P = 0.002), respectively). At the time of the first VF obtained after RVO, mean deviation averaged –10.3 dB in the affected eyes, compared with –5.0 dB in the fellow eyes (P < 0.001); in contrast, RNFL thickness was similar between eyes at the time of OAG diagnosis (72 µm versus 74 µm, P = 0.290). Predictive factors for OAG diagnosis included higher intraocular pressure (IOP) and cup-to-disc ratio (CDR) in the unaffected eye, and the absence of macular edema in the RVO-affected eye (R2 = 0.375, P < 0.001).
Conclusions
OAG is a significant risk factor for RVO. Our study reveals a reciprocal relationship between RVO and the development of OAG, highlighting the need for glaucoma risk assessment in all patients with RVOs to avoid delays in diagnosis and vision loss from glaucoma.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the nature of this research, as participants of this study did not agree for their data to be shared publicly but are available from the corresponding author on reasonable request.
References
Wong TY, Scott IU. Clinical practice. Retinal-vein occlusion. N Engl J Med. 2010;363:2135–44.
Rogers S, McIntosh RL, Cheung N, Lim L, Wang JJ, Mitchell P, et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia and Australia. Ophthalmology. 2010;117:313.e1–319.e1.
Tham YC, Li X, Wong TY, Quigley HA, Aung Y, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
Hayreh SS, Zimmerman MB, Beri M, Podhajsky P. Intraocular pressure abnormalities associated with central and hemicentral retinal vein occlusion. Ophthalmology. 2004;111:133–41.
Schwaber EJ, Fogelman N, Sobol EK, Mehrotra D, Powell JA, Mian U, et al. Associations with retinal vascular occlusions in a diverse, urban population. Ophthalmic Epidemiol. 2018;25:220–6.
Yin X, Li J, Zhang B, Lu P. Association of glaucoma with risk of retinal vein occlusion: a meta-analysis. Acta Ophthalmol. 2019;97:652–9.
Kim YN, Shin JW, Park YJ, Lee JY, Kim JG, Yoon YH, et al. Glaucoma as a prognostic factor of central retinal vein occlusion: visual and anatomical outcomes and occurrence of ischaemic central retinal vein occlusion. Acta Ophthalmol. 2021;99:e523–30.
Klein BE, Meuer SM, Knudtson MD, Klein R. The relationship of optic disk cupping to retinal vein occlusion: the Beaver Dam Eye Study. Am J Ophthalmol. 2006;141:859–62.
Verhoeff FH. The effect of chronic glaucoma on the central retinal vessels. Arch Ophthalmol. 1913;42:145–52.
Han JC, Eo DR, Lee TK, Shin JH, Kee C. Does glaucoma share common pathogenesis with branch retinal vein occlusion? PLoS ONE. 2016;11:e0156966.
Quality of Care Committee Glaucoma Panel. Preferred practice patterns: primary open-angle glaucoma. San Francisco: American Academy of Ophthalmology; 1992.
Gedde SJ, Vinod K, Wright MM, Muir KW, Lind JT, Chen PP, et al. Primary open-angle glaucoma preferred practice pattern®. Ophthalmology. 2021;128:P71–P150.
Li Y, Hall NE, Pershing S, Hyman L, Haller JA, Lee AY, et al. Age, gender, and laterality of retinal vascular occlusion: a retrospective study from the IRIS® Registry. Ophthalmol Retina. 2022;6:161–71.
Calugaru M. The incidence of primary open-angle glaucoma in patients with central retinal vein occlusion. Oftalmologia. 2000;52:22–27.
Kim SJ, Park KH. Four cases of normal-tension glaucoma with disk hemorrhage combined with branch retinal vein occlusion in the contralateral eye. Am J Ophthalmol. 2004;137:357–9.
Lopilly Park HY, Jeon S, Lee MY, Park CK. Glaucoma progression in the unaffected fellow eye of glaucoma patients who developed unilateral branch retinal vein occlusion. Am J Ophthalmol. 2017;175:194–200.
Kim MJ, Woo SJ, Park KH, Kim TW. Retinal nerve fiber layer thickness is decreased in the fellow eyes of patients with unilateral retinal vein occlusion. Ophthalmology. 2011;118:706–10.
Shin YI, Nam KY, Lee SE, Lim HB, Lee MW, Jo YJ, et al. Changes in peripapillary microvasculature and retinal thickness in the fellow eyes of patients with unilateral retinal vein occlusion: an OCTA study. Invest Ophthalmol Vis Sci. 2019;60:823–9.
Kim YJ, Sung KR, Lee KS, Joe SG, Lee JY, Kim JG, et al. Long-term effects of multiple intravitreal antivascular endothelial growth factor injections on intraocular pressure. Am J Ophthalmol. 2014;157:1266–71.e1.
Eadie BD, Etminan M, Carleton BC, Maberley DA, Mikelberg FS. Association of repeated intravitrous bevacizumab injections with risk for glaucoma surgery. JAMA Ophthalmol. 2017;135:363–8.
Lloyd MJ, Mansberger SL, Fortune BA, Nguyen H, Torres R, Demirel S, et al. Features of optic disc progression in patients with ocular hypertension and early glaucoma. J Glaucoma. 2013;22:343–8.
Mergen B, Ramsey DJ. Underdiagnosis of glaucoma in patients with exudative age-related macular degeneration. Eye. 2021;35:3350–7.
Kelly DS, Ganti T, Ramsey DJ. Underdiagnosis of risk of glaucoma in patients with retinal vein occlusions. Eye. 2022;36:2350–2.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13.
Gracitelli CPB, Zangwill LM, Diniz-Filho A, Abe RY, Girkin CA, Weinreb RN, et al. Detection of glaucoma progression in individuals of African descent compared with those of European descent. JAMA Ophthalmol. 2018;136:329–35.
Sharma A, Roh S, Ramsey DJ. Targeted telephone-based outreach reconnects glaucoma patients with subspecialty care. J Glaucoma. 2024;33:28–34.
Chiang MF, Sommer A, Rich WL, Lum F, Parke DW,2nd. The 2016 American Academy of Ophthalmology IRIS® Registry (Intelligent Research in Sight) database: characteristics and methods. Ophthalmology. 2018;125:143–1148.
Lee PP, Levin LA, Walt JG, Chiang TH, Doyle JJ, Stern LS, et al. The impact of glaucoma coding in a large claims database. Am J Ophthalmol. 2007;143:867–70.
Bearelly S, Mruthyunjaya P, Tzeng JP, Suner IJ, Shea AM, Lee JT, et al. Identification of patients with diabetic macular edema from claims data: a validation study. Arch Ophthalmol. 2008;126:986–9.
Gupta P, Zhao D, Guallar E, Ko F, Boland MV, Friedman DS. Prevalence of glaucoma in the United States: the 2005-2008 National Health and Nutrition Examination Survey. Invest Ophthalmol Vis Sci. 2016;57:2905–13.
Mansberger SL, Gordon MO, Jampel H, Bhorade A, Brandt JD, Wilson B, et al. Reduction in intraocular pressure after cataract extraction: the Ocular Hypertension Treatment Study. Ophthalmology. 2012;119:1826–31.
Lee BW, Murakami Y, Duncan MT, Kao AA, Huang JY, Lin S, et al. Patient-related and system-related barriers to glaucoma follow-up in a county hospital population. Invest Ophthalmol Vis Sci. 2013;54:6542–8.
Acknowledgements
The authors thank Dr. Shiyoung Roh, Dr. Paul R. Cotran, Dr. Michael L. Cooper, Dr. Haohua Qian, Dr. Kathryn M. Ramsey, Hilcia M. Downs, as well as Carol Spencer, Lahey Hospital Librarian, for research support. D.J. Ramsey was supported by the Harry N. Lee Family Chair in Innovation at the Lahey Hospital & Medical Center, Beth Israel Lahey Health. Manuscript is derived from presentations: “Delay in Diagnosis of Glaucoma after Retinal Vein Occlusion,” presented at the 2023 American Glaucoma Society (AGS) Annual Meeting, Austin, TX, and “Delay in Screening Risks Underdiagnosis of Open-angle Glaucoma in Patients with Retinal Vein Occlusions,” presented at the 2023 Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting, New Orleans, LA.
Funding
DJR: Supported by the Harry N. Lee Family Chair in Innovation, Lahey Hospital & Medical Center, Beth Israel Lahey Health, Peabody, MA.
Author information
Authors and Affiliations
Contributions
DJR was responsible for the study hypothesis and design, the development of electronic medical record reporting tools, reviewing and analyzing the data, interpreting the results, and writing of the manuscript. REM was responsible for the chart review, extracting and analyzing the data, figure development, and writing of the manuscript. AH was responsible for the chart review, extracting and analyzing the data, and writing of the manuscript. AMA was responsible for the chart review, extracting and analyzing the data, and writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muhtaseb, R.E., Huther, A., Alwreikat, A.M. et al. Optimizing open-angle glaucoma risk assessment in patients with retinal vein occlusions. Eye 38, 2985–2991 (2024). https://doi.org/10.1038/s41433-024-03205-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03205-y