Abstract
Purpose
To describe the postoperative outcomes of eyes with primary full-thickness macular holes (MH) greater than 650 μm.
Design
Retrospective, monocentric, consecutive case series.
Participants
Patients with primary MH operated at Lariboisière Hospital, Paris, France.
Methods
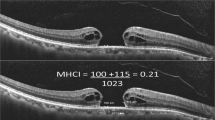
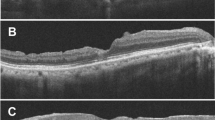
Records of patients with MH with a minimum horizontal diameter greater than 650 μm that underwent primary surgery with internal limiting membrane (ILM) peeling (complete or with inverted ILM flap) between January 2010 and January 2022 were reviewed.
Main outcome measures
Postoperative MH closure rate and visual acuity.
Results
74 eyes of 73 patients met the inclusion criteria. The mean minimum horizontal diameter was 777 ± 108 µm (650-1114). It ranged between 650 and 800 µm in 40 eyes (54%) and was ≧ 800 µm in 34 eyes (46%). The closure rate was 77% (57/74) after primary surgery and was significantly higher in MH between 650 and 800 µm, than in MH ≧ 800 µm (87.5% versus 64.7%, p = 0.02). In the 58/74 eyes in which conventional ILM peeling was performed, closure rate was 74.1% (43/58), significantly higher in MH ranging between 650 and 800 µm than in MH ≧ 800 µm (84.8% versus 60.0%, p = 0.03). In closed MH, 50/64 (78%) eyes achieved a VA gain ≥0.2 logMAR (3 lines), and 14 (21.9%) eyes a final BCVA ≥ 0.3 logMAR.
Conclusion
MH surgery with conventional ILM peeling allowed closed MH ≧ 650 μm and < 800 μm with a success rate close to 85% that decreased in larger MH. A significant visual improvement was achieved after MH closure, even in MH ≧ 800 μm.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Meuer SM, Myers CE, Klein BEK, Swift MK, Huang Y, Gangaputra S, et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography. Ophthalmology. 2015;122:787–95.
Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Retina. 1991;11:447.
Tadayoni R, Gaudric A, Haouchine B, Massin P. Relationship between macular hole size and the potential benefit of internal limiting membrane peeling. Br J Ophthalmol. 2006;90:1239–41.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611–9.
Ch’ng SW, Patton N, Ahmed M, Ivanova T, Baumann C, Charles S, et al. The Manchester large macular hole study: is it time to reclassify large macular holes? Am J Ophthalmol. 2018;195:36–42.
Yamashita T, Sakamoto T, Terasaki H, Iwasaki M, Ogushi Y, Okamoto F, et al. Best surgical technique and outcomes for large macular holes: retrospective multicentre study in Japan. Acta Ophthalmol. 2018;96:e904–10.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Rezende FA, Ferreira BG, Rampakakis E, Steel DH, Koss MJ, Nawrocka ZA, et al. Surgical classification for large macular hole: based on different surgical techniques results: the CLOSE study group. Int J Retina Vitr. 2023;9:4.
Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnon R, et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol. 2002;120:29.
Ullrich S. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002;86:390–3.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg visual acuity test. Investig Opthalmology Vis Sci. 2006;47:1236.
Yuguchi T, Ogura S, Hirano Y, Suzuki N, Yasukawa T, Ogura Y. Autologous posterior capsule flap transplantation in the management of refractory macular hole in a pseudophakic eye. Retin Cases Brief Rep. 2023;17:85–8.
The BEAVRS Macular hole outcome group, Steel DH, Donachie PHJ, Aylward GW, Laidlaw DA, Williamson TH, et al. Factors affecting anatomical and visual outcome after macular hole surgery: findings from a large prospective UK cohort. Eye. 2021;35:316–25.
Shukla D, Kalliath J. Internal limiting membrane peeling for large macular hole: tailoring the rhexis to the shape of the hole. Indian J Ophthalmol. 2022;70:182.
Gu C, Qiu Q. Inverted internal limiting membrane flap technique for large macular holes: a systematic review and single-arm meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2018;256:1041–9.
Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F. Internal limiting membrane peeling versus inverted flap technique for treatment of full-thickness macular holes: a comparative study in a large series of patients. Retina. 2018;38:S73–8.
Kannan NB, Kohli P, Parida H, Adenuga OO, Ramasamy K. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC Ophthalmol. 2018;18:177.
Shen Y, Lin X, Zhang L, Wu M. Comparative efficacy evaluation of inverted internal limiting membrane flap technique and internal limiting membrane peeling in large macular holes: a systematic review and meta-analysis. BMC Ophthalmol. 2020;20:14.
Bottoni F, Parrulli S, Mete M, D’Agostino I, Cereda M, Cigada M, et al. Large idiopathic macular hole surgery: remodelling of outer retinal layers after traditional internal limiting membrane peeling or inverted flap technique. Int J Ophthalmol. 2020;243:334–41.
Iwasaki M, Ando R, Aoki S, Miyamoto H. Restoration process of the outer retinal layers after surgical macular hole closure. Retina. 2022;42:313–20.
Bolo KA, Chang S. Broad internal limiting membrane peeling with adjunctive plasma–thrombin for repair of large macular holes: a retrospective case series. Eur J Ophthalmol. 2021;31:1338–44
Zhang H, Li Y, Chen G, Han F, Jiang W. Human amniotic membrane graft for refractory macular hole: a single-arm meta-analysis and systematic review. J Fr Ophtalmol. 2023;46:276–86.
Author information
Authors and Affiliations
Contributions
Design (RT, MB, IC, AC), Data collection (MB, IC), Data analysis (MB, IC, AC, EP, RT), Drafting the manuscript (MB, IC, EP), Manuscript Revision (RT, EP), Submission (EP). All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Data are available for queries.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bencheqroun, M., Couturier, A., Chehaibou, I. et al. Macular holes with minimal diameter greater than 650 µm close in 85% of cases after vitrectomy and ILM peeling with visual benefit. Eye 38, 3341–3346 (2024). https://doi.org/10.1038/s41433-024-03302-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03302-y