Abstract
Background
Ophthalmology consultation on inpatients is often important to optimise eye care and provide information for referring teams. Inpatient consultation may constitute a not-insignificant workload however. This study reports on the nature and necessity of ophthalmology inpatient consults in a large Irish hospital.
Methods
Retrospective analysis of all consecutive ophthalmology inpatient consultations over a 12-month period.
Results
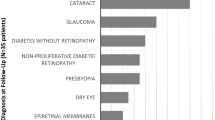
In total, 359 consult requests were received primarily from adult medicine (57.9%), surgery (22%) and paediatric teams (18.4%). The most common reasons for referral were loss of vision (23.7%); visual field testing (15%); diplopia or abnormal eye movements (11.4%); and screening for ocular features of systemic disease (10.6%). Presumptive diagnoses by referring teams were correct in 29.5% of cases. The majority had normal eye examinations (53.2%) or non-sight-threatening features (16.8%), while a minority had acute eye pathology (30%). Most patients (80.4%) required no intervention. A minority required medical (12.5%), orthoptic (4.6%) or surgical (2.4%) intervention. The majority of patients (81%) were fit for transfer to the eye clinic and did not require bedside examination.
Conclusions
Our study found a high proportion of ophthalmology inpatient consultations had normal eye exams and required no intervention. The quality of referrals was variable suggesting that clearer guidelines and more ophthalmology education is needed for referring teams.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that supports the findings of this study are available from the corresponding author (RM), upon reasonable request.
References
Scantling-Birch Y, Naveed H, Tollemache N, Gounder P, Rajak S. Is undergraduate ophthalmology teaching in the United Kingdom still fit for purpose? Eye (Lond). 2022;36:343–5.
Lipkova V, Asodaria P, Fu L, O'Sullivan EP. Quality of inpatient ophthalmology referrals and implications for undergraduate ophthalmology teaching. Eye. 2022;36:2365–6.
Gelston CD, Patnaik JL. Ophthalmology training and competency levels in care of patients with ophthalmic complaints in United States internal medicine, emergency medicine and family medicine residents. J Educ Eval Health Prof. 2019;16:25.
Health Service Executive, Irish College of Ophthalmologists. National clinical programme for ophthalmology Model of Eye Care. 2017.
Singh JS, Imbrogno VM, Howard MK, Cheema AS, Selvadurai AD, Bansal S. Relocation consequences on an ophthalmology consultation service from an inpatient to outpatient facility. Clin Ophthalmol. 2015;9:1859–63.
Mayer J, Landis Z, Wang M, Scott IU. Characteristics of inpatient ophthalmology consults associated with ocular pathology and need for ophthalmologic intervention. Invest Ophthalmol Vis Sci. 2014;55:5554.
Patel SH, Park S, Rosenberg JB. Comparison of pediatric and adult ophthalmology consultations in an urban academic medical center. J Pediatr Ophthalmol Strabismus. 2017;54:17–21.
Jacobs J, Bielory B, Wandel T, Juechter K. Comparison of adult versus pediatric ophthalmology consults at a tertiary Level 1 trauma medical center. Invest Ophthalmol Vis Sci. 2017;58:2434.
Bala C, Poon, JC, Joblin P, McCluskey PJ. Ophthalmologists in teaching hospitals: do we make a difference to patient outcome? Clin Exp Ophthalmol. 2001;29:59–63.
Fattah M, Abuzubida A, Al Qahtani FM. Ophthalmology consultations in a large specialist hospital. Acta Sci Ophthalmol. 2022;5.5:65–8.
Kayoma DH, Ukponmwan CU, Ese-Onakewhor JN. Evaluation of ophthalmology inpatients consultation in a Nigerian tertiary eye care centre. West Afr J Med. 2020;37:221–4.
Tajunisah I, Azida J, Zuria A, Reddy SC. Ophthalmology inpatient consultation: does it make a difference to inpatient management? Med J Malays. 2009;64:130–3.
Hazelwood J, Nderitu P. The reliability of visual acuity measurements from inpatient referrals to ophthalmology. Eye (Lond). 2022;36:666–8.
Schachat AP, McDonnell PJ, Petty BG, Jampel HD, Patel A, Wittpenn JR, et al. Ophthalmology consultations at a large teaching hospital. Metab Pediatr Syst Ophthalmol. 1985;12:105–9.
Rowe FJ, Wright D, Brand D, Jackson C, Harrison S, Maan T, et al. A prospective profile of visual field loss following stroke: prevalence, type, rehabilitation, and outcome. Biomed Res Int. 2013;12:719096.
Gnanalingham KK, Bhattachajee S, Pennington R, Ng J, Mendoza N. The time course of visual field recovery following transphenoidal surgery for pituitary adenomas: predictive factors for a good outcome. J Neurol Neurosurg Psychiatry. 2005;76:415–9.
Rowe FJ, Hepworth LR, Howard LR, Hanna KL, Cheyne CP, Currie J. High incidence and prevalence of visual problems after acute stroke: An epidemiology study with implications for service delivery. PLoS One. 2019;14:e0213035.
Belin PJ, Greaves G, Weiss A, Winokur J, Gorski M. Characteristics and incidence of inpatient ophthalmology consultations to screen for papilledema. Invest Ophthalmol Vis Sci. 2017;58:3307.
Nazir S, O'Brien M, Qureshi NH, Slape L, Green TJ, Phillips PH. Sensitivity of papilledema as a sign of shunt failure in children. J AAPOS. 2009;13:63–6.
Dozier CC, Tarantla RM, Jiramongkolchai K, Donahue SP. Fungal eye disease at a tertiary care center: the utility of routine inpatient consultation. Ophthalmology. 2011;118:1671–6.
Breazzano MP, Day HR Jr, Bloch KC, Tanaka S, Cherney EF, Sternberg P Jr., et al. Utility of ophthalmologic screening for patients with candida bloodstream infections: a systematic review. JAMA Ophthalmol. 2019;137:698–710.
Breazzano MP, Bond JB 3rd, Bearelly S, Kim DH, Donahue SP, Lum F, et al. American academy of ophthalmology recommendations on screening for endogenous candida endophthalmitis. Ophthalmology. 2022;129:73–6.
Oh DJ, Kanu LN. Inpatient and emergency room ophthalmology consultations at a tertiary care center. J Ophthalmol 2019;7807391.
Carter K, Miller KM. Ophthalmology inpatient consultation. Ophthalmology. 2001;108:1505–11.
Grewal DS, Chiang E, Wong E, Volpe NJ, Bryar PJ. Adult ophthalmology inpatient consults at a tertiary care teaching hospital. Ophthalmology. 2014;121:1489–e1481.
Gautam N, Ram R, Bustamante E, Sharrah D, Mets-Halgrimson R. Pediatric ophthalmology inpatient consults at a tertiary care children’s hospital. J AAPOS. 2023;27:75.e71–75.e75.
Frisbie J, Cornman H, Swamy R, Alexander JL, Kemp PS, Friedrich R, et al. A novel interactive virtual medical student clinical rotation for ophthalmology. J Acad Ophthalmol (2017). 2022;14:e52–e9.
Kilduff CL, Thomas AA, Dugdill J, Casswell EJ, Dabrowski M, Lovegrove C, et al. Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Health Care Inf. 2020;27:e100179.
Kalra G, Commiskey PW, Schempf T, Williams AM, Bowers EMR, Waxman EL, et al. Initial results and patient survey of virtual inpatient ophthalmology consultations during the COVID-19 Pandemic. Semin Ophthalmol. 2021;36:461–8.
Lupidi M, Danieli L, Fruttini D, Nicolai M, Lassandro N, Chhablani J, et al. Artificial intelligence in diabetic retinopathy screening: clinical assessment using handheld fundus camera in a real-life setting. Acta Diabetol. 2023;60:1083–8.
Nagino K, Sung J, Midorikawa-Inomata A, Eguchi A, Fujimoto K, Okumura Y, et al. Clinical utility of smartphone applications in ophthalmology: a systematic review. Ophthalmol Sci. 2024;4:100342.
Corr RH. Fundoscopy in the smartphone age: current ophthalmoscopy methods in neurology. Arq Neuropsiquiatr. 2023;81:502–9.
Wang H, Liao X, Zhang M, Pang CP, Chen H. Smartphone ophthalmoscope as a tool in teaching direct ophthalmoscopy: a crossover randomized controlled trial. Med Educ online. 2023;28:2176201.
Gardiner MF, Miller JW. The ophthalmic hospitalist. Ophthalmology. 2020;127:1143–4.
Khurshid SG, Duff SM. A solution for inpatient ophthalmology coverage! Int J Clin Pract. 2021;75:e14464.
Kim DH. Perspectives from an ophthalmic hospitalist-changing how we view hospital-based consults. J Acad Ophthalmol (2017). 2023;15:e258–e60.
Author information
Authors and Affiliations
Contributions
RM was responsible for data collection and writing the report. EA contributed to data collection. MJ, ZI and EoC contributed to reviewing and editing the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previously presented at Irish College of Ophthalmologists Annual Meeting 2022.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McGrath, R., Ahern, E., James, M. et al. Ophthalmology inpatient consultations: an Irish tertiary hospital experience. Eye 38, 3519–3524 (2024). https://doi.org/10.1038/s41433-024-03354-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03354-0
This article is cited by
-
Inpatient urology consultations: intervention rates, determinant factors, and findings related to the refugee population
World Journal of Urology (2025)