Abstract
Objectives
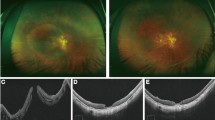
To assess the specific features of myopic traction maculopathy (MTM) in the context of myopic macular atrophy (MA). The evolution, surgical considerations, optimal surgical procedures, and results were studied.
Methods
Retrospective, consecutive cases collection was performed for highly myopic eyes with MA (category 4, the classification system of META-analysis for Pathologic Myopia). Eighty-seven eyes of 75 patients with MA were included. The characteristics and evolution of the MTM were analyzed. Surgical indications and outcomes were evaluated and specific surgical features and techniques were assessed.
Results
Approximately half (50.6%) of the cases with MA presented with various stages of MTM. The majority were maculoschisis with a lamellar macular hole (LMH) and were characterized by an O-shaped LMH, high outer retinal schisis, thin floor, and a high percentage of thickened epiretinal tissue. Half (50%) of them either displayed maculoschisis progression (61%) or developed into macular hole with retinal detachment (39%), and all received surgical intervention. The inverted ILM flap technique, with or without fovea-sparing ILM peeling, was the most frequently used surgical technique (78%). Complete traction relief was achieved in most cases (94%).
Conclusion
MA contributes to the specific configuration and evolution of MTM, and characteristic maculoschisis with LMH is a frequent presentation in MA patients. MHRD development and structural progression were two major reasons for surgical intervention. Vitrectomy with inverted ILM flap effectively stabilized the macular structure with few recurrences.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Ohno-Matsui K, Kawasaki R, Jonas JB, Cheung CM, Saw SM, Verhoeven VJ, et al. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159:877–83.e877.
Ruiz-Medrano J, Montero JA, Flores-Moreno I, Arias L, García-Layana A, Ruiz-Moreno JM. Myopic maculopathy: current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019;69:80–115.
Hsia Y, Lee CY, Ho TC, Yang CH, Yang CM. The development and evolution of lamellar macular hole in highly myopic eyes. Eye. 2023;37:1170–7.
Tian J, Qi Y, Lin C, Cao K, Wang N. The association in myopic tractional maculopathy with myopic atrophy maculopathy. Front Med. 2021;8:679192.
Chen Q, He J, Hu G, Xu X, Lv H, Yin Y, et al. Morphological characteristics and risk factors of myopic maculopathy in an older high myopia population—based on the new classification system (ATN). Am J Ophthalmol. 2019;208:356–66.
Pereira A, Ballios BG, Sarraf D, Yan P. Full-thickness macular hole due to choroidal neovascularization in the setting of pathologic myopia. J Vitreoretin Dis. 2023;7:65–9.
Lin CW, Ho TC, Yang CM. The development and evolution of full thickness macular hole in highly myopic eyes. Eye. 2015;29:388–96.
Tsui MC, Hsieh YT, Lai TT, Hsia Y, Wang SW, Ma IH, et al. Vitreoretinal interface changes after anti-vascular endothelial growth factor treatment in highly myopic eyes: a real-world study. Ophthalmol Ther. 2023;12:1693–710.
Ohno-Matsui K, Jonas JB. Posterior staphyloma in pathologic myopia. Prog Retin Eye Res. 2019;70:99–109.
Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004;122:1455–60.
Govetto A, Dacquay Y, Farajzadeh M, Platner E, Hirabayashi K, Hosseini H, et al. Lamellar macular hole: two distinct clinical entities? Am J Ophthalmol. 2016;164:99–109.
Cheong KX, Xu L, Ohno-Matsui K, Sabanayagam C, Saw SM, Hoang QV. An evidence-based review of the epidemiology of myopic traction maculopathy. Surv Ophthalmol. 2022;67:1603–30.
You QS, Peng XY, Xu L, Chen CX, Wang YX, Jonas JB. Myopic maculopathy imaged by optical coherence tomography: the Beijing eye study. Ophthalmology. 2014;121:220–4.
Parolini B, Palmieri M, Finzi A, Besozzi G, Lucente A, Nava U, et al. The new Myopic Traction Maculopathy Staging System. Eur J Ophthalmol. 2021;31:1299–312.
Fang D, Zhang Z, Wei Y, Wang L, Zhang T, Jiang X, et al. The morphological relationship between dome-shaped macula and myopic retinoschisis: a cross-sectional study of 409 highly myopic eyes. Invest Ophthalmol Vis Sci. 2020;61:19.
Baba T, Ohno-Matsui K, Futagami S, Yoshida T, Yasuzumi K, Kojima A, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135:338–42.
Wakazono T, Yamashiro K, Miyake M, Nakanishi H, Oishi A, Ooto S, et al. Association between eye shape and myopic traction maculopathy in high myopia. Ophthalmology. 2016;123:919–21.
Azuma K, Hirasawa K, Araki F, Shiraya T, Yashiro S, Kato S, et al. Fovea-sparing as opposed to total peeling of internal limiting membrane for myopic foveoschisis: a systematic review and meta-analysis. Ophthalmol Retin. 2021;5:670–9.
Sun CB, Liu Z, Xue AQ, Yao K. Natural evolution from macular retinoschisis to full-thickness macular hole in highly myopic eyes. Eye. 2010;24:1787–91.
Li S, Li T, Wang X, Cai X, Lu B, Chen Y, et al. Natural course of myopic traction maculopathy and factors influencing progression and visual acuity. BMC Ophthalmol. 2021;21:347.
Lee C-Y, Hsia Y, Yang C-M. Formation and evolution of idiopathic lamellar macular hole-a pilot study. BMC Ophthalmol. 2022;22:432.
Hsia Y, Ho TC, Yang CH, Hsieh YT, Lai TT, Yang CM. Clinical characteristics and long-term evolution of lamellar macular hole in high myopia. PLoS ONE. 2020;15:e0232852.
Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156:948–57.e941.
Jo Y, Ikuno Y, Nishida K. Retinoschisis: a predictive factor in vitrectomy for macular holes without retinal detachment in highly myopic eyes. Br J Ophthalmol. 2012;96:197–200.
Frisina R, Gius I, Palmieri M, Finzi A, Tozzi L, Parolini B. Myopic traction maculopathy: diagnostic and management strategies. Clin Ophthalmol. 2020;14:3699–708.
Shimada N, Ohno-Matsui K, Yoshida T, Sugamoto Y, Tokoro T, Mochizuki M. Progression from macular retinoschisis to retinal detachment in highly myopic eyes is associated with outer lamellar hole formation. Br J Ophthalmol. 2008;92:762–4.
Ohno-Matsui K, Yoshida T, Futagami S, Yasuzumi K, Shimada N, Kojima A, et al. Patchy atrophy and lacquer cracks predispose to the development of choroidal neovascularisation in pathological myopia. Br J Ophthalmol. 2003;87:570–3.
Yoshida T, Ohno-Matsui K, Ohtake Y, Takashima T, Futagami S, Baba T, et al. Long-term visual prognosis of choroidal neovascularization in high myopia: a comparison between age groups. Ophthalmology. 2002;109:712–9.
Yoshida T, Ohno-Matsui K, Yasuzumi K, Kojima A, Shimada N, Futagami S, et al. Myopic choroidal neovascularization: a 10-year follow-up. Ophthalmology. 2003;110:1297–305.
Zhao X, Ding X, Lyu C, Li S, Liu B, Li T, et al. Morphological characteristics and visual acuity of highly myopic eyes with different severities of myopic maculopathy. Retina. 2020;40:461–7.
Ohno-Matsui K, Jonas JB, Spaide RF. Macular bruch membrane holes in choroidal neovascularization-related myopic macular atrophy by swept-source optical coherence tomography. Am J Ophthalmol. 2016;162:133–39.e131.
Li KKW, Wong DHT, Li PSH. Are we facing an increasing surgical demand for high myopic traction maculopathies? A 12-year study from Hong Kong. BMC Ophthalmol. 2023;23:31.
Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007;125:767–72.
Gómez-Resa M, Burés-Jelstrup A, Mateo C. Myopic traction maculopathy. Dev Ophthalmol. 2014;54:204–12.
Hattori K, Kataoka K, Takeuchi J, Ito Y, Terasaki H. Predictive factors of surgical outcomes in vitrectomy for myopic traction maculopathy. Retina. 2018;38:S23–30.
Shimada N, Sugamoto Y, Ogawa M, Takase H, Ohno-Matsui K. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012;154:693–701.
Wakatsuki Y, Nakashizuka H, Tanaka K, Mori R, Shimada H. Outcomes of vitrectomy with fovea-sparing and inverted ILM flap technique for myopic foveoschisis. J Clin Med. 2022;11:1274.
Lin JP, Yang CM. Combined fovea-sparing internal limiting membrane peeling with internal limiting membrane flap technique for progressive myopic traction maculopathy. Graefes Arch Clin Exp Ophthalmol. 2022;260:489–96.
Uramoto K, Azuma T, Watanabe T, Takahashi H, Igarashi-Yokoi T, Shimada N, et al. Extreme macular schisis-simulating retinal detachment in eyes with pathologic myopia. Retina. 2022;42:1836–43.
Flores-Moreno I, Puertas M, Ruiz-Medrano J, Almazán-Alonso E, García-Zamora M, Ruiz-Moreno JM. Influence of posterior staphyloma in myopic maculopathy and visual prognosis. Eye. 2024;38:145–52.
Ruiz-Moreno JM, Puertas M, Flores-Moreno I, Almazán-Alonso E, García-Zamora M, Ruiz-Medrano J. Posterior staphyloma as determining factor for myopic maculopathy. Am J Ophthalmol. 2023;252:9–16.
Lee CY, Hsia Y, Tsui MC, Wang SW, Huang CJ, Ma IH, et al. Correlation of visual acuity and outer retinal thickness in myopic atrophic maculopathy: a retrospective review. Ophthalmol Ther. 2023;12:1989–2003.
Author information
Authors and Affiliations
Contributions
CYL conducted data curation, formal analysis, investigation, and figure production, wrote the original draft, and contributed to manuscript revision and editing. TTL, TCC, and YTH were involved in conceptualization, provided resources, contributed to methodology development, and offered feedback on the manuscript. TCH participated in conceptualization, provided resources, assisted with methodology development, guided the discussion, and offered feedback. CHY provided resources, assisted with methodology development, and commented on the manuscript. CMY contributed to conceptualization, supervised the investigation, validated the methodology and final results, provided resources, and reviewed, revised, edited, and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, CY., Lai, TT., Chen, TC. et al. Myopic traction maculopathy in fovea-involved myopic chorioretinal atrophy. Eye 38, 3586–3594 (2024). https://doi.org/10.1038/s41433-024-03366-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03366-w
This article is cited by
-
Diabetic macular atrophy, a pilot exploration of its characteristics, progression, and visual implications
Eye (2026)
-
Efficacy of posterior scleral reinforcement in the management of myopic traction maculopathy: a single-arm retrospective study
BMC Ophthalmology (2025)
-
Comment on: ‘Myopic traction maculopathy in fovea-involved myopic chorioretinal atrophy’
Eye (2025)
-
Classification and management of myopic traction maculopathy: a vitrectomy-based consensus from taiwanese experts
International Ophthalmology (2025)