Abstract
Objectives
To investigate the population-based incidence of uveitis and the differences between anterior and non-anterior uveitis using the comprehensive Korean National Health Insurance Service (NHIS) database.
Methods
We extracted data of patients who visited the clinic and were diagnosed with uveitis (based on Korean Classification of Diseases) from 2010 to 2021. The incidence of uveitis, differences between the demographics, and the underlying co-morbidities of anterior uveitis, non-anterior uveitis, and control groups were investigated.
Results
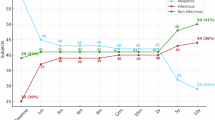
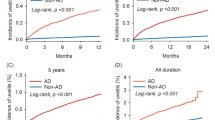
We identified 919,370 cases with uveitis (anterior: 800,132; non-anterior: 119,238). The average incidences (per 10,000 persons) of anterior and non-anterior uveitis were 13.0 (95% confidence interval [CI], 12.9–13.0), and 1.9 (95% CI, 1.9–1.9), respectively. The incidence increased (2010: 13.0; 2019: 16.5) but decreased during the coronavirus disease (COVID-19) pandemic (2020: 15.5; 2021: 15.4). The non-anterior group was significantly associated with sex (female, odds ratio [OR]: 1.09, p < 0.0001), specific age range (40–69 years, p < 0.0001), high Charlson Comorbidity Index (p < 0.0001), high household income (p < 0.0001), and various immunologic diseases (antiphospholipid antibody syndrome, OR: 1.79, p < 0.0001; systemic lupus erythematosus, OR: 1.22, p < 0.0001; psoriasis, OR: 1.13, p < 0.0001; ulcerative colitis, OR: 1.11, p = 0.0013; tuberculosis, OR: 1.09, p < 0.0001; rheumatoid arthritis, OR: 1.05, p < 0.0001) compared with the anterior group.
Conclusions
Using the NHIS database, we conducted the largest population-based epidemiological study on uveitis in South Korea to estimate its increasing incidence in the past decade (including changes during COVID-19 pandemic) as well as its anatomical distribution. Our results may be beneficial for estimating the national burden of uveitis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Jabs DA, McCluskey P, Palestine AG, Thorne JE. The standardisation of uveitis nomenclature (SUN) project. Clin Exp Ophthalmol. 2022;9:991–1000.
Tomkins-Netzer O, Talat L, Bar A, Lula A, Taylor SRJ, Joshi L, et al. Long-term clinical outcome and causes of vision loss in patients with uveitis. Ophthalmology. 2014;121:2387–92.
de Smet MD, Taylor SRJ, Bodaghi B, Miserocchi E, Murray PI, Pleyer U, et al. Understanding uveitis: the impact of research on visual outcomes. Prog Retin Eye Res. 2011;30:452–70.
Suttorp-Schulten MS, Rothova A. The possible impact of uveitis in blindness: a literature survey. Br J Ophthalmol. 1996;80:844–8.
García-Aparicio Á, García de Yébenes MJ, Otón T, Muñoz-Fernández S. Prevalence and Incidence of Uveitis: A Systematic Review and Meta-analysis. Ophthalmic Epidemiol. 2021;28:461–8.
Rim TH, Kim SS, Ham DI, Yu SY, Chung EJ, Lee SC. Incidence and prevalence of uveitis in South Korea: a nationwide cohort study. Br J Ophthalmol. 2018;102:79–83.
Acharya NR, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, et al. Incidence and prevalence of uveitis: results from the pacific ocular inflammation study. JAMA Ophthalmol. 2013;131:1405–12.
Zhang Y, Amin S, Lung KI, Seabury S, Rao N, Toy BC. Incidence, prevalence, and risk factors of infectious uveitis and scleritis in the United States: A claims-based analysis. PloS one. 2020;15:e0237995.
Miettinen R. Incidence of uveitis in Northern Finland. Acta Ophthalmol. 1977;55:252–60.
Hwang D-K, Chou Y-J, Pu C-Y, Chou P. Epidemiology of uveitis among the Chinese population in Taiwan: a population-based study. Ophthalmology. 2012;119:2371–6.
Kim ST, Seong SC 2016 national health insurance statistical yearbook. Health Insurance Review and Assessment Service, National Health Insurance service, 2017:622.
Kim BH, Chang IB, Lee S, Oh B-L, Hong IH. Incidence and prevalence of pediatric noninfectious uveitis in Korea: a population-based study. J Korean Med Sci. 2022;37. https://doi.org/10.3346/jkms.2022.37.e344.
Lerner A. 11th Annual Congress on immunology: the world incidence and prevalence of autoimmune diseases is increasing. J Timely Top Clin Immunol. 2018;2:42.
Miller FW. The increasing prevalence of autoimmunity and autoimmune diseases: an urgent call to action for improved understanding, diagnosis, treatment, and prevention. Curr Opin Immunol. 2023;80:102266.
Glover K, Mishra D, Singh TRR. Epidemiology of ocular manifestations in autoimmune disease. Front Immunol. 2021;12:744396.
Song YJ. The South Korean health care system. JMAJ. 2009;52:206–9.
OECD. Health at a Glance 2015. 2015.
Kang E, Yun J, Hwang S-H, Lee H, Lee JY. The impact of the COVID-19 pandemic in the healthcare utilization in Korea: Analysis of a nationwide survey. J Infect Public Health. 2022;15:915–21.
Sim B, Nam EW. The Impact of COVID-19 pandemic on outpatient visits for all-cause and chronic diseases in Korea: a nationwide population-based study. Int J Environ Res Public Health. 2022;19:5674.
Lee M, You M. Avoidance of Healthcare Utilization in South Korea during the Coronavirus Disease 2019 (COVID-19) Pandemic. Int J Environ Res Public Health. 2021;18:4363.
Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020;183:40–41.
Lee H, Park J. Changes in health care utilization during the MERS epidemic. Int J Infect Dis. 2018;73:187.
Tomer Y, Shoenfeld Y. Ageing and autoantibodies. Autoimmunity. 1988;1:141–9.
Vadasz Z, Haj T, Kessel A, Toubi E. Age-related autoimmunity. BMC Med. 2013;11:94.
Wang L, Wang F-S, Gershwin ME. Human autoimmune diseases: a comprehensive update. J Intern Med. 2015;278:369–95.
Do S-R. “Changes in healthcare utilization in South Korea”. Health Welf Issue Focus. 2009;8:1–8.
Gritz DC. Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004;111:491–500.
Rathinam SR, Krishnadas R, Ramakrishnan R, Thulasiraj RD, Tielsch JM, Katz J, et al. Population-based prevalence of uveitis in Southern India. Br J Ophthalmol. 2011;95:463–7.
González MM, Solano MM, Porco TC, Oldenburg CE, Acharya NR, Lin SC, et al. Epidemiology of uveitis in a US population-based study. J Ophthalmic Inflamm Infect. 2018;8:6.
Miquel C-H, Faz-Lopez B, Guéry J-C. Influence of X chromosome in sex-biased autoimmune diseases. J Autoimmun. 2023:102992. https://doi.org/10.1016/j.jaut.2023.102992
Desai MK, Brinton RD. Autoimmune disease in women: endocrine transition and risk across the lifespan. Front Endocrinol. 2019;10:265.
Cohen-Solal JF, Jeganathan V, Hill L, Kawabata D, Rodriguez-Pinto D, Grimaldi C, et al. Hormonal regulation of B-cell function and systemic lupus erythematosus. Lupus. 2008;17:528–32.
Robert J, Alastair K, Benjamin R. Rheumatic Disease. In: Sadda S, Schachat A, Wilkinson C, editors. Ryan’s Retina. 7th ed. Amsterdam: Elsevier Health Sciences; 2022. p. 1684-712.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Alian SM, Khalil SS, Zaghlol RS. Charlson comorbidity index in patients with systemic lupus erythematosus in egypt and its relation with disease characteristics. Indian J Rheumatol. 2019;14:277–82.
Dick AD, Tundia N, Sorg R, Zhao C, Chao J, Joshi A, et al. Risk of ocular complications in patients with noninfectious intermediate uveitis, posterior uveitis, or panuveitis. Ophthalmology. 2016;123:655–62.
Acknowledgements
We would like to thank Biostatistical Consulting and the Research Lab of Hanyang University for assistance with statistical analysis.
Funding
This research was supported by the National Research Foundation of Korea (NRF) grants funded by the Korean government (RS-2023-00251816 (HC) and NRF-2021R1I1A1A01059690 (EHH)). The Byers Eye Institute is supported by funding from the National Eye Institute (NEI P30-EY026877) and from the Research to Prevent Blindness, Inc. The funding organizations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
EHH was responsible for interpretation of the results, funding acquisition, and writing the original draft. JK was responsible for data extraction and analysis and drafted the original manuscript. SP was responsible for validation of the analysis and edited the manuscript. HC was responsible for funding acquisition and providing resources. MHK interpreted the results and provided resources. AB, ANTT, AA, CMCO, and ZXT validated the analysis and reviewed the manuscript. YUS conceived and supervised the presented work, interpreted the results and critical reviewed the manuscript. QDN was responsible for funding acquisition and supervised the presented work. All authors contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hong, E.H., Kim, J., Park, S. et al. Trends in nationwide incidence of uveitis in South Korea using the National Health Insurance claims database from 2010 to 2021. Eye 39, 1123–1131 (2025). https://doi.org/10.1038/s41433-024-03500-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-024-03500-8