Abstract
Objective
This study aimed to analyse the correlation between corneal astigmatism and disparity in corneal thickness.
Methods
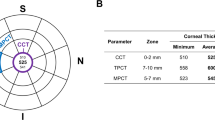
In this retrospective analysis, data from 342 patients (684 eyes) were collected. The Sirius three-dimensional corneal topography system was utilised to ascertain the mean corneal thickness of the meridians. Correlation analyses were conducted between the mean difference in corneal thickness along the two principal meridians and the astigmatic values computed by simulated keratometry values (Sim-K) for total corneal astigmatism (TCA) and posterior corneal astigmatism (PCA), respectively. Variability in differential corneal thickness (DCT) values at different TCA levels was analysed. The variability of DCT within the 3-mm corneal range at different differences between whole-eye astigmatism and TCA (Difference between corneal astigmatism and computer optometry, DWT) levels was analysed.
Results
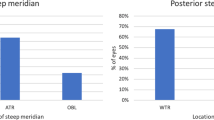
Within the ranges of 3, 4.5, and 6 mm, the mean corneal thickness of the meridian with the maximum refractive power (Sim-K2) was greater than that of the meridian with the minimum refractive power (Sim-K1) (P < 0.05). The TCA showed a negative correlation with DCT across all three ranges (P < 0.001), whereas PCA exhibited a positive correlation with DCT (P < 0.001). A difference was observed among the TCA groups within each range, with DCT increasing alongside the dioptre of astigmatism (P < 0.05). In the 3 mm corneal range, an increase in the difference in corneal thickness was associated with an increase in the difference between whole-eye astigmatism and TCA (P < 0.05).
Conclusion
The meridian with the maximum refractive power had a thicker mean corneal thickness than the meridian with the minimum refractive power. The difference in corneal thickness is closely related to the severity of corneal astigmatism. The extent of residual astigmatism is influenced by this thickness difference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Moshirfar M, Reynolds JC, Moin KA, Lim MY, Stoakes IM, Hoopes PC. Perioperative recommendations for corneal refractive surgery patients with inherited bleeding disorders. Cornea. 2024. https://doi.org/10.1097/ICO.0000000000003631.
Betz J, Locatelli EVT, Harkness BM, Perez-Blanco M, Everist SJ, Chen S, et al. Prospective cohort study investigating frequency and risk factors for acute pain 1 day after refractive surgery. BMJ Open Ophthalmol. 2024;9:e001624. https://doi.org/10.1136/bmjophth-2023-001624.
Feng Y, Nitter T, Bertelsen G, Stojanovic A. Repeatability and agreement of total corneal astigmatism measured in keratoconic eyes using four current devices. Clin Exp Ophthalmol. 2024. https://doi.org/10.1111/ceo.14423.
Song T, Nie F, Zhao Y, Liao M, He L, Tang Q, et al. Ocular Dominance Shift in Refractive Cataract Surgery: A prospective, observational study. J Cataract Refract Surg. 2024. https://doi.org/10.1097/j.jcrs.0000000000001520.
Meyer JJ, Gokul A, Vellara HR, Prime Z, McGhee CN. Repeatability and agreement of Orbscan II, Pentacam HR, and Galilei tomography systems in corneas with keratoconus. Am J Ophthalmol. 2017;175:122–8. https://doi.org/10.1016/j.ajo.2016.12.003.
Li HY, Li J, Song H. The distribution of the back-front corneal radius ratio and its effect on the corneal refractive power based on Pentacam. Recent Adv Ophthalmol. 2020;40:1065–9.
Ho JD, Tsai CY, Tsai RJ, Kuo LL, Tsai IL, Liou SW. Validity of the keratometric index: evaluation by the Pentacam rotating Scheimpflug camera. J Cataract Refract Surg. 2008;34:137–45. https://doi.org/10.1016/j.jcrs.2007.09.033.
Fam HB, Lim KL. Validity of the keratometric index: large population-based study. J Cataract Refract Surg. 2007;33:686–91. https://doi.org/10.1016/j.jcrs.2006.11.023.
Savini G, Versaci F, Vestri G, Ducoli P, Næser K. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg. 2014;40:1645–53. https://doi.org/10.1016/j.jcrs.2014.01.046.
Mendes J, Ribeiro FJ, Ferreira TB. Evaluation of posterior and total corneal astigmatism with colour-LED topography. Eye (Lond). 2021;35:2585–93. https://doi.org/10.1038/s41433-020-01278-z.
Sano M, Hiraoka T, Ueno Y, Itagaki H, Ogami T, Oshika T. Influence of posterior corneal astigmatism on postoperative refractive astigmatism in pseudophakic eyes after cataract surgery. BMC Ophthalmol. 2016;16:212. https://doi.org/10.1186/s12886-016-0391-1.
Wang L, Cao D, Vilar C, Koch DD. Posterior and total corneal astigmatism measured with optical coherence tomography-based biometer and dual Scheimpflug analyzer. J Cataract Refract Surg. 2020;46:1652–8. https://doi.org/10.1097/j.jcrs.0000000000000327.
Lu AQ, Poulsen A, Cui D, Seeger C, Lehman E, Scott IU, et al. Repeatability and comparability of keratometry measurements obtained with swept-source optical coherence and combined dual Scheimpflug-Placido disk-based tomography. J Cataract Refract Surg. 2020;46:1637–43. https://doi.org/10.1097/j.jcrs.0000000000000346.
Gao YC, Jiang YF, Lin S, Tian F. Comparison of corneal refractive power and astigmatism measured by the new anterior segment optical coherence tomographic device and Scheimpflug imaging device in age-related cataract patients]. Zhonghua Yan Ke Za Zhi. 2021;57:48–55. https://doi.org/10.3760/cma.j.cn112142-20200904-00574. Chinese
Feizi S, Delfazayebaher S, Javadi MA. Agreement Between Internal Astigmatism and Posterior Corneal Astigmatism in Pseudophakic Eyes. J Refract Surg. 2018;34:379–86. https://doi.org/10.3928/1081597X-20180425-01.
Cao JM, Cha X, Zhang YP. Research Progress of Personalized Incision for Surgical Astigmatism and Refractive Cataract. Modern Med Health. 2022;38:2798–803.
Liu Y, Zhao SZ, Yang RB, Liu H. Effect of limbal release incision for correction of preoperative astigmatism on corneal curvature in cataract. New Progress Ophthalmol. 2016;36:340–4. https://doi.org/10.13389/j.cnki.rao.2016.0092.
Reinstein DZ, Archer TJ, Vida RS. Epithelial thickness mapping for corneal refractive surgery. Curr Opin Ophthalmol. 2022;33:258–68. https://doi.org/10.1097/ICU.0000000000000867.
Agarwal L, Agrawal N, Badhu BP, Lavaju P. Central corneal thickness and intraocular pressure in patients of primary open angle glaucoma and normal population in Nepalese population: a hospital based study. Nepal J Ophthalmol. 2019;11:46–54. https://doi.org/10.3126/nepjoph.v11i1.25418.
Milla M, Piñero DP, Amparo F, Alió JL. Pachymetric measurements with a new Scheimpflug photography-based system: intraobserver repeatability and agreement with optical coherence tomography pachymetry. J Cataract Refract Surg. 2011;37:310–6. https://doi.org/10.1016/j.jcrs.2010.08.038.
Funding
Research Project of Sichuan Provincial Administration of Traditional Chinese Medicine (No.2021MS296).
Author information
Authors and Affiliations
Contributions
Conception and design of the work: Zhao D, Mei B; Data collection: Zhu LT, Wen L, Zhou CY; Supervision: Zhao D, Mei B; Analysis and interpretation of the data: Zhu LT, Wen L, Zhou CY; Statistical analysis: Zhao D, Mei B; Drafting the manuscript: Zhao D, Mei B; Critical revision of the manuscript: all authors; Approval of the final manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Ineye Hospital of Chengdu University of TCM (No. 2020yh-004) and conducted in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained from all subjects prior to any study-related procedures or examinations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, D., Mei, B., Zhu, L. et al. Analysing the correlation between differential corneal thickness along principal meridians and corneal astigmatism: implications for whole-eye astigmatism. Eye 39, 1465–1469 (2025). https://doi.org/10.1038/s41433-025-03645-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03645-0