Abstract
Background
Extended reality (XR) simulators, including virtual reality and augmented reality, hold significant promise for enhancing surgical training by providing trainees with a controlled practice environment. This is particularly vital in microsurgery, where the steep learning curve and the challenge of mastering surgical skills are significant. Despite notable advancements in XR technology, its role in ophthalmic surgical training remains uncertain.
Methods
In our systematic review and meta-analysis, eight electronic databases were searched, and studies were evaluated against predefined criteria. Data extraction and random-effects meta-analysis assessed the odds ratio (OR) for posterior capsular rupture (PCR), an important surgical complication.
Results
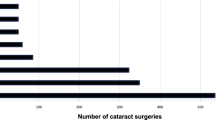
A meta-analysis of 17,623 eyes that underwent cataract surgery across seven studies revealed a significant decrease in PCR post-Eyesi practice, with low heterogeneity across studies (OR = 0.71, 95% CI = 0.60-0.85, I2 = 9%). Studies that predominantly utilized XR for cataract surgery training (84%) consistently improved surgical outcomes by reducing complications such as PCR, retained lens material, and aphakia. XR training also significantly improved operating scores (p < 0.05), self-efficacy (p < 0.01), and non-dominant hand dexterity (p < 0.01). Of the 25 studies in this review, 22 (88%) found overall XR training benefits.
Conclusions
XR simulators enhance ophthalmic surgical training by reducing complications like PCR, and improving surgical performance, self-efficacy, and non-dominant hand dexterity. These findings challenge conventional training methods and advocate for integrating XR into residency curricula to optimize learning and patient outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Javid P, Aydın A, Mohanna PN, Dasgupta P, Ahmed K. Current status of simulation and training models in microsurgery: A systematic review. Vol. 39, Microsurgery. John Wiley and Sons Inc.; 2019. p. 655–68.
Binenbaum G, Volpe NJ. Ophthalmology resident surgical competency. A National Survey. Ophthalmology 2006;113:1237–44.
Alfawaz AM Ophthalmology resident surgical training: Can we do better? Vol. 33, Saudi Journal of Ophthalmology. Elsevier B.V.; 2019. p. 159–62.
Chauhan R, Ingersol C, Wooden WA, Gordillo GM, Stefanidis D, Hassanein AH, et al. Fundamentals of Microsurgery: A Novel Simulation Curriculum Based on Validated Laparoscopic Education Approaches. In: Journal of Reconstructive Microsurgery. Thieme Medical Publishers, Inc; 2022. p. 517–25.
Al Saedi NG, Al-Sharif EM, Mousa A, Alsuhaibani AH. The impact of surgical training on the practice of recently graduated ophthalmologists at Riyadh’s ophthalmology residency program. Saudi J Ophthalmol. 2019;33:319–25.
Gedde SJ, Volpe NJ, Feuer WJ, Binenbaum G Reports Ophthalmology Resident Surgical Competence: A Survey of Program Directors [Internet]. 2020. Available from: www.aaojournal.org.
Ropelato S, Menozzi M, Michel D, Siegrist M. Augmented reality microsurgery: a tool for training micromanipulations in ophthalmic surgery using augmented reality. Simul Healthc. 2020;15:122–7.
Gavira N, Benayoun M, Hamel Q, Fournier HD, Bigorre N. Learning, teaching, and training in microsurgery: a systematic review. Hand Surg Rehabilitation Elsevier Masson s r l. 2022;41:296–304.
Badash I, Burtt K, Solorzano CA, Carey JN. Innovations in surgery simulation: a review of past, current and future techniques. Ann Transl Med. 2016;4:453.
Clarke E. Virtual reality simulation—the future of orthopaedic training? A systematic review and narrative analysis. Adv Simul. 2021;6:2.
Andrews C, Southworth MK, Silva JNA, Silva JR. Extended reality in medical practice. Vol. 21, Current Treatment Options in Cardiovascular Medicine. Springer Healthcare; 2019.
Zhang J, Lu V, Khanduja V. The impact of extended reality on surgery: a scoping review. Int Orthop Inst Ion. 2023;47:611–21.
Aydındoğan G, Kavaklı K, Şahin A, Artal P, Ürey H. Applications of augmented reality in ophthalmology [Invited]. Biomed Opt Express. 2021;12:511.
Ong CW, Tan MCJ, Lam M, Koh VTC Applications of extended reality in ophthalmology: Systematic review. Vol. 23, Journal of Medical Internet Research. JMIR Publications Inc.; 2021.
Deng Z, Xiang N, Pan J State of the Art in Immersive Interactive Technologies for Surgery Simulation: A Review and Prospective. Bioengineering [Internet]. 2023 Dec 1 [cited 2024 Apr 1];10. Available from: /pmc/articles/PMC10740891/
Ng DS, Yip BHK, Young AL, Yip WWK, Lam NM, Li KK, et al. Cost-effectiveness of virtual reality and wet laboratory cataract surgery simulation. Med (U S). 2023;102:E35067.
Iskander M, Ogunsola T, Ramachandran R, McGowan R, Al-Aswad LA. Virtual reality and augmented reality in ophthalmology: a contemporary prospective. Asia Pac J Ophthalmol (Philos). 2021;10:244 https://pmc.ncbi.nlm.nih.gov/articles/PMC9167643/.
Pieramici DJ, Heimann F, Brassard R, Barteselli G, Ranade S. Virtual reality becomes a reality for ophthalmologic surgical clinical trials. Transl Vis Sci Technol. 2020;9:1–5.
Lowater SJ, Grauslund J, Vergmann AS Modern Educational Simulation-Based Tools Among Residents of Ophthalmology: A Narrative Review. Vol. 11, Ophthalmology and Therapy. Adis; 2022. p. 1961–74.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. The BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Online). 2016;355:I4919.
Schünemann H, Brożek J, Guyatt G, Oxman A GRADE Handbook [Internet]. 2013 [cited 2024 Apr 13]. Available from: https://gdt.gradepro.org/app/handbook/handbook.html#h.m9385o5z3li7
Johnston RL, Taylor H, Smith R, Sparrow JM. The cataract national dataset electronic multi-centre audit of 55 567 operations: variation in posterior capsule rupture rates between surgeons. Eye 2010;24:888–93.
Chakrabarti A, Nazm N Posterior capsular rent: Prevention and management. Vol. 65, Indian Journal of Ophthalmology. Medknow Publications; 2017. p. 1359–69.
West SL, Gartlehner G, Mansfield AJ, Poole C, Tant E, Lenfestey N, et al. Comparative Effectiveness Review Methods: Clinical Heterogeneity. Comparative Effectiveness Review Methods: Clinical Heterogeneity [Internet]. 2010 [cited 2024 Apr 15]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK53310/.
Daly MK, Gonzalez E, Siracuse-Lee D, Legutko PA. Efficacy of surgical simulator training versus traditional wet-lab training on operating room performance of ophthalmology residents during the capsulorhexis in cataract surgery. J Cataract Refract Surg. 2013;39:1734–41.
Sun W, Kong J, Li XY, Zhang JS Application of operational simulation training system in the training of ophthalmic students Citation. International Eye Science. 2014;14:524–31.
Deuchler S, Wagner C, Singh P, Müller M, Al-Dwairi R, Benjilali R, et al. Clinical efficacy of simulated vitreoretinal surgery to prepare surgeons for the upcoming intervention in the operating room. PLoS One. 2016;11:e0150690.
Hu YG, Liu QP, Gao N, Wu CR, Zhang J, Qin L, et al. Efficacy of wet-lab training versus surgical-simulator training on performance of ophthalmology residents during chopping in cataract surgery. Int J Ophthalmol. 2021;14:26–31.
Baxter JM, Lee R, Sharp JAH, Foss AJE, Vernon SA, Maharajan S, et al. Intensive cataract training: a novel approach. Eye (Basingstoke). 2013;27:742–6.
Bergqvist J, Person A, Vestergaard A, Grauslund J. Establishment of a validated training programme on the Eyesi cataract simulator. A prospective randomized study. Acta Ophthalmol. 2014;92:629–34.
Ferris JD, Donachie PH, Johnston RL, Barnes B, Olaitan M, Sparrow JM. Royal college of ophthalmologists’ national ophthalmology database study of cataract surgery: Report 6. the impact of eyesi virtual reality training on complications rates of cataract surgery performed by first and second year trainees. Br J Ophthalmol. 2020;104:324–9.
Lopez-Beauchamp C, Singh GA, Shin SY, Magone MT. Surgical simulator training reduces operative times in resident surgeons learning phacoemulsification cataract surgery. Am J Ophthalmol Case Rep. 2020;17:100576.
Lucas L, Schellini SA, Lottelli AC. Complications in the first 10 phacoemulsification cataract surgeries with and without prior simulator training. Arq Bras Oftalmol. 2019;82:289–94.
McCannel CA Continuous curvilinear capsulorhexis training and non-rhexis related vitreous loss: the specificity of virtual reality simulator surgical training (an American Ophthalmological Society thesis). Vol. 115, Trans Am Ophthalmol Soc. 2017.
Montrisuksirikun C, Trinavarat A, Atchaneeyasakul LO Effect of surgical simulation training on the complication rate of resident-performed phacoemulsification. BMJ Open Ophthalmol. 2022;7:e000958.
Pokroy R, Du E, Alzaga A, Khodadadeh S, Steen D, Bachynski B, et al. Impact of simulator training on resident cataract surgery. Graefe’s Arch Clin Exp Ophthalmol. 2013;251:777–81.
Staropoli PC, Gregori NZ, Junk AK, Galor A, Goldhardt R, Goldhagen BE, et al. Surgical Simulation Training Reduces Intraoperative Cataract Surgery Complications among Residents. Simulation in. Healthcare 2018;13:11–5.
McCannel CA, Reed DC, Goldman DR. Ophthalmic surgery simulator training improves resident performance of capsulorhexis in the operating room. Trans Am Ophthalmol Soc. 2013;120:2456–61.
Sankarananthan R, Senthil Prasad R, Koshy TA, Dharani P, Bacchav A, Lansingh VC, et al. An objective evaluation of simulated surgical outcomes among surgical trainees using manual small-incision cataract surgery virtual reality simulator. Indian J Ophthalmol. 2022;70:4018–25.
Wisse RPL, Coster T, Van Der Schaaf M, Ten Cate O. The Eyesi simulator in training ophthalmology residents: Results of a pilot study on self-efficacy, motivation and performance. BMJ Simul Technol Enhanc Learn. 2017;3:111–5.
Nair AG, Ahiwalay C, Bacchav AE, Sheth T, Lansingh VC, Vedula SS, et al. Effectiveness of simulation-based training for manual small incision cataract surgery among novice surgeons: a randomized controlled trial. Sci Rep. 2021;11:10945.
Selvander M, Asman P. Ready for OR or not? Human reader supplements Eyesi scoring in cataract surgical skills assessment. Clin Ophthalmol. 2013;7:1973–7.
Cremers SL, Lora AN, Ferrufino-Ponce ZK. Global rating assessment of skills in intraocular surgery (GRASIS). Ophthalmology. 2005;112:1655–60.
Saleh GM. Objective structured assessment of cataract surgical skill. Arch Ophthalmol. 2007;125:363.
Saleh GM, Lamparter J, Sullivan PM, O’Sullivan F, Hussain B, Athanasiadis I, et al. The international forum of ophthalmic simulation: developing a virtual reality training curriculum for ophthalmology. Br J Ophthalmol. 2013;97:789–92.
Bisol T, Bisol RA, de R, Rezende F. Efficacy of Eyesi® surgical simulator training in improving high-tension capsules capsulorhexis performance. Rev Bras Oftalmol. 2016;75:376–9.
Gonzalez-Gonzalez LA, Payal AR, Gonzalez-Monroy JE, Daly MK. Ophthalmic surgical simulation in training dexterity in dominant and nondominant hands: Results from a pilot study. J Surg Educ. 2016;73:699–708.
Eltanamly RM, Elmekawey H, Youssef MM, Hassan LM. Can virtual reality surgical simulator improve the function of the non-dominant hand in ophthalmic surgeons? Indian J Ophthalmol. 2022;70:1795–9.
Sikder S, Luo J, Banerjee PP, Luciano C, Kania P, Song JC, et al. The use of a virtual reality surgical simulator for cataract surgical skill assessment with 6 months of intervening operating room experience. Clin Ophthalmol. 2015;9:141–9.
Deuchler S, Scholtz J, Ackermann H, Seitz B, Koch F. Implementation of microsurgery simulation in an ophthalmology clerkship in Germany: a prospective, exploratory study. BMC Med Educ. 2022;22:599.
Thomsen ASS, Bach-Holm D, Kjærbo H, Højgaard-Olsen K, Subhi Y, Saleh GM, et al. Operating Room Performance Improves after Proficiency-Based Virtual Reality Cataract Surgery Training. Ophthalmology 2017;124:524–31.
Mathis T, Mouchel R, Malecaze J, Garcin T, Mautuit T, Kodjikian L, et al. Evaluation of the time required to complete a cataract training program on EyeSi surgical simulator during the first-year residency. Eur J Ophthalmol. 2023;33:767–73.
WilliamsMAMcveighJHandaAI. 202496:537–42. https://academic.oup.com/pmj/article/96/1139/537/6958936 [Internet]. 2020 [citedMar 30].
Larsen CR, Soerensen JL, Grantcharov TP, Dalsgaard T, Schouenborg L, Ottosen C, et al. Effect of virtual reality training on laparoscopic surgery: Randomised controlled trial. BMJ (Online). 2009;338:1253.
Seymour NE, Gallagher AG, Roman SA, O’brien MK, Bansal VK, Andersen DK, et al. Virtual reality training improves operating room performance results of a randomized, double-blinded study. Ann Surg. 2002;236:458–63.
Suresh D, Aydin A, James S, Ahmed K, Dasgupta P. The role of augmented reality in surgical training: a systematic review. Surg Innov. 2023;30:366–82. https://pubmed.ncbi.nlm.nih.gov/36412148/.
Hart R, Doherty DA, Karthigasu K, Garry R. The value of virtual reality-simulator training in the development of laparoscopic surgical skills. J Minim Invasive Gynecol. 2006;13:126–33.
Chahal B, Aydin A, Ahmed KC URRENT OPINION Virtual reality vs. physical models in surgical skills training. An update of the evidence. 2023 [cited 2024 Mar 31]; Available from: www.co-urology.com.
Lees MC, Zheng B, Daniels LM, White JS. Factors Affecting the Development of Confidence Among Surgical Trainees. J Surg Educ. 2019;76:674–83.
Hodge W, Horsley T, Albiani D, Baryla J, Belliveau M, Buhrmann R, et al. The consequences of waiting for cataract surgery: A systematic review. CMAJ Can Med Assoc J. 2007;176:1285–90.
Szigiato AA, Trope GE, Jin Y, Buys YM Wait times and volume of cataract surgery in Ontario: 2000-2012. [cited 2024 Mar 31]; Available from: https://doi.org/10.1016/j.jcjo.2015.09.006.
Chan FW, Fan AH, Wong FY, Lam PT, Yeoh EK, Yam CH, et al. Waiting Time for Cataract Surgery and Its Influence on Patient Attitudes. Invest Ophthalmol Vis Sci. 2009;50:3636–42.
Lowry EA, Porco TC, Naseri A Cost analysis of virtual-reality phacoemulsification simulation in ophthalmology training programs. J Cataract Refract Surg [Internet]. 2013 Oct [cited 2024 Mar 31];39:1616–7. Available from: https://journals.lww.com/jcrs/fulltext/2013/10000/cost_analysis_of_virtual_reality.25.aspx.
Dexter F, Dexter EU, Masursky D, Nussmeier NA. Systematic review of general thoracic surgery articles to identify predictors of operating room case durations. Anesth Analg. 2008;106:1232–41. https://journals.lww.com/anesthesia-analgesia/fulltext/2008/04000/systematic_review_of_general_thoracic_surgery.31.aspx.
Pike TW, Pathak S, Mushtaq F, Wilkie RM, Mon-Williams M, Lodge JPA. A systematic examination of preoperative surgery warm-up routines. Surg Endosc. 2017;31:2202–14.
Feeley A, Feeley IH, Merghani K, Sheehan E. Use of procedure specific preoperative warm-up during surgical priming improves operative outcomes: A systematic review. Am J Surg. 2022;224:1126–34.https://pubmed.ncbi.nlm.nih.gov/35654638/
Feng S, Yi JS, Deitz G, Ding L, Van Gelder RN, Menda S. Relationships Between Sleep, Activity, and Burnout in Ophthalmology Residents. J Surg Educ. 2021;78:1035–40.
Selvander M, Åsman P. Cataract surgeons outperform medical students in Eyesi virtual reality cataract surgery: evidence for construct validity. Acta Ophthalmol. 2013;91:469–74.
Mahr MA, Hodge DO. Construct validity of anterior segment anti-tremor and forceps surgical simulator training modules: attending versus resident surgeon performance. J Cataract Refract Surg. 2008;34:980–5.
Nayer ZH, Murdock B, Dharia IP, Belyea DA. Predictive and construct validity of virtual reality cataract surgery simulators. J Cataract Refractive Surg Lippincott Williams Wilkins. 2020;46:907–12.
Acknowledgements
The authors would like to thank Caitlin McClurg for her valuable advice and technical support in developing the systematic search strategy.
Author information
Authors and Affiliations
Contributions
LY was responsible for project conceptualization, writing the review protocol, screening potentially eligible studies, extracting and analysing data, interpreting results, conducting the meta-analysis, creating tables and figures, writing the original manuscript, and reviewing and reviewing and editing the manuscript. AA was responsible for project conceptualization, designing and writing the review protocol, arbitrating potentially eligible studies, extracting and analysing data, interpreting results, conducting the meta-analysis, creating tables and figures, writing the original manuscript, and reviewing and reviewing and editing the manuscript. MSB was responsible for screening potentially eligible studies, conducting the meta-analysis, creating tables and figures, writing the original manuscript, and reviewing and editing the manuscript. PG and HC were responsible for the project’s conceptualization, manuscript drafting, review, and editing, as well as overall project supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, L., Al-Ani, A., Bondok, M.S. et al. The impact of extended reality simulators on ophthalmic surgical training and performance: a systematic review and meta-analysis of 17,623 eyes. Eye 39, 1700–1709 (2025). https://doi.org/10.1038/s41433-025-03722-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03722-4