Abstract
Introduction
Iris melanomas are a rare entity accounting for 2–5% of uveal melanomas. The most frequent primary treatment for circumscribed iris melanomas is irradiation, particularly by proton beam therapy (PBT). Short-term efficacy is encouraging but there is little data on long-term tumour control and side effects.
Objectives
To describe the long-term results in terms of local and systemic control, eye preservation and side-effects after PBT for circumscribed iris melanomas.
Methods
Retrospective chart review of patients treated by PBT between 1998 and 2022. Diffuse iris melanomas, ciliary body melanomas with iris involvement or tumours with extrascleral invasion were excluded.
Results
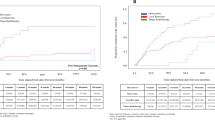
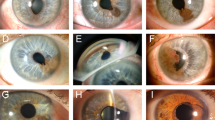
Of 143 patients treated by PBT, n = 91 were treated five years or more before data update and were included. Median follow-up was 10.7 years (range 1.7–22.7 years). Documented growth was present for 74% of patients. The median clinical largest diameter was 5 mm, and the median ultrasound thickness was 2.1 mm. The tumour invaded the iridocorneal angle in 68% of patients. Overall survival was 94%. Three patients presented with metastatic disease, of which one died of metastasis. Seven deaths were unrelated to iris melanoma. Five (3.5%) patients experienced ocular relapse. The most frequent complications were cataract and raised intraocular pressure (no neovascular glaucoma). Four patients (4.3%) required secondary enucleation.
Conclusion
Long-term follow-up confirms that PBT is an excellent treatment option for localized iris melanomas, with very favourable local tumour control, eye preservation, and overall survival. Relapses are very rare but can occur several years after treatment, warranting a prolonged follow-up.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to confidentiality restrictions but are available from the corresponding author on reasonable request.
References
Popovic M, Ahmed IIK, DiGiovanni J, Shields CL. Radiotherapeutic and surgical management of iris melanoma: a review. Surv Ophthalmol. 2017;62:302–11.
Lumbroso-Le Rouic L, Delacroix S, Dendale R, Levy-Gabriel C, Feuvret L, Noel G, et al. Proton beam therapy for iris melanomas. Eye. 2006;20:1300–5.
Damato B, Kacperek A, Chopra M, Sheen MA, Campbell IR, Errington RD. Proton beam radiotherapy of iris melanoma. Int J Radiat Oncol Biol Phys. 2005;63:109–15. https://doi.org/10.1016/j.ijrobp.2005.01.050.
Thariat J, Rahmi A, Salleron J, Mosci C, Butet B, Maschi C, et al. Proton beam therapy for iris melanomas in 107 patients. Ophthalmology. 2018;125:606–14.
Willerding GD, Cordini D, Hackl C, Karle B, Lakotka N, Foerster MH, et al. Proton beam radiotherapy of diffuse iris melanoma in 54 patients. Br J Ophthalmol. 2015;99:812–6.
Sabazade S, Herrspiegel C, Gill V, StÃ¥lhammar G. No differences in the long-term prognosis of iris and choroidal melanomas when adjusting for tumor thickness and diameter. BMC Cancer. 2021;21:021–09002.
Msika LC, Desjardins L, Cockenpot V, Dendale R, Berges O, Aït Raïs K, et al. Iris melanoma relapsing sixteen years after proton-beam therapy: the importance of lifelong follow-up. Am J Ophthalmol Case Rep. 2018;13:89–92.
Marigo FA, Finger PT. Anterior segment tumors: current concepts and innovations. Surv Ophthalmol. 2003;48:569–93.
Shields J, Shields C. Melanocytic tumors of the iris stroma. In: Intraocular tumors A text and atlas. Philadelphia, Pennsylvania: Saunders; 1992. p. 69–77.
Gollrad J, Boeker A, Vitzthum S, Besserer A, Heufelder J, Gauger U, et al. Proton therapy for 166 patients with iris melanoma: side effects and oncological outcome. Ophthalmol Retin. 2022;6530:00452–3.
Eibenberger K, Heimann H, Gatchalian L, Kacperek A, Hussain R. Side effects of proton beam radiotherapy treatment on iris melanoma. Ophthalmology. 2023;130:958–65.
Sandinha MT, Kacperek A, Errington RD, Coupland SE, Damato B. Recurrence of iris melanoma after proton beam therapy. Br J Ophthalmol. 2014;98:484–7.
Kivela T, Simpson ER, Grossniklaus HE, Jager MJ, Singh AD, Caminal JM, Pavlick AC, et al. PT Finger Uveal melanoma. In: Amin M, editor. AJCC cancer staging manual, 8th ed. New York (NY): Springer; 2017. p. 805–17.
Shields CL, Di Nicola M, Bekerman VP, Kaliki S, Alarcon C, Fulco E, et al. Iris melanoma outcomes based on the American Joint Committee on cancer classification (eighth edition) in 432 patients. Ophthalmology. 2018;125:913–23.
Shields CL, Shah SU, Bianciotto CG, Emrich J, Komarnicky L, Shields JA. Iris melanoma management with iodine-125 plaque radiotherapy in 144 patients: impact of melanoma-related glaucoma on outcomes. Ophthalmology. 2013;120:55–61.
Acknowledgements
Nathalie Algret (data manager).
Author information
Authors and Affiliations
Contributions
LLR: Conceptualization; Supervision; Writing—original draft; Writing—review & editing. XM: Formal analysis; Methodology; Validation; Visualization; Writing—original draft; Writing—review & editing, SD: Data curation; Formal analysis; Methodology; Validation; Visualization; Writing—original draft; Writing—review & editing. FD: Writing—original draft; Writing—review & editing. RD: Conceptualization; Writing—original draft, Writing—review & editing. AM: Writing—original draft; Writing—review & editing. NC: Writing—original draft, Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lumbroso-Le Rouic, L., Maynadier, X., Goudjil, F. et al. Long-term follow-up of circumscribed iris melanomas treated by proton beam therapy. Eye 39, 2599–2603 (2025). https://doi.org/10.1038/s41433-025-03934-8
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03934-8