Abstract
Background
Diabetic retinopathy (DR) is the leading cause of preventable blindness. Although hyperglycaemia is the primary driver, other modifiable risk factors may contribute to DR development. This study investigated the association between haemoglobin levels and DR risk in adults with type 2 diabetes.
Methods
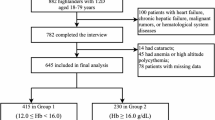
We conducted a retrospective cohort study using the TriNetX network (2010–2022). Adults aged ≥45 years with type 2 diabetes were divided into low haemoglobin (LHB, 8–12 g/dL) and control (≥12 g/dL) groups. Propensity score matching was used to address potential confounders. The primary outcome was new-onset DR occurring 6–36 months after the index date. The secondary outcomes included DR subtypes and diabetic ophthalmic complications. Subgroup analyses examined effect modifications by hypertension status, glycaemic control, and sex.
Results
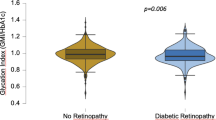
After propensity score matching (28,882 patients per group), patients in the LHB group showed significantly higher risk of overall DR (HR: 1.33, 95% CI: 1.24–1.44), proliferative DR (HR: 1.95, 95% CI: 1.62–2.35), and non-proliferative DR (HR: 1.19, 95% CI: 1.06–1.33). Even mild haemoglobin reductions (10–12 g/dL) were associated with increased DR risk. The association was stronger in patients without hypertension (HR: 1.58 vs 1.21), remained consistent regardless of HbA1c levels, and was more pronounced in males than females.
Conclusion
Low haemoglobin levels independently increased the risk of DR in adults with type 2 diabetes, with the strongest association for proliferative DR. Routine haemoglobin monitoring and maintenance of optimal levels may represent a modifiable risk factor for DR prevention along with glycaemic control and blood pressure management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the TriNetX Research Network, but restrictions apply to the availability of these data, which were used under a collaboration agreement for the current study, and so are not publicly available. Data are available from the corresponding author (Kuo-Chuan Hung) upon reasonable request and with permission from TriNetX. Access to de-identified data requires either TriNetX network membership or establishment of a collaborative agreement with TriNetX.
References
Kropp M, Golubnitschaja O, Mazurakova A, Koklesova L, Sargheini N, Vo T-TKS, et al. Diabetic retinopathy as the leading cause of blindness and early predictor of cascading complications—risks and mitigation. EPMA J. 2023;14:21–42.
Steinmetz JD, Bourne RRA, Briant PS, Flaxman SR, Taylor HRB, Jonas JB, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e60.
Teo ZL, Tham Y-C, Yu M, Chee ML, Rim TH, Cheung N, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128:1580–91.
Ting DSW, Cheung GCM, Wong TY. Diabetic retinopathy: global prevalence, major risk factors, screening practices and public health challenges: a review. Clin Exp Ophthalmol. 2016;44:260–77.
Bek T. Systemic risk factors contribute differently to the development of proliferative diabetic retinopathy and clinically significant macular oedema. Diabetologia. 2020;63:2462–70.
Sakko S, Karpale M, Tapio J, Leppänen I, Ahokas O, Saarela V, et al. Hemoglobin levels are associated with retinal vascular caliber in a middle-aged birth cohort. Sci Rep. 2024;14:9092.
Zhuang X, Cao D, Zeng Y, Yang D, Yao J, Kuang J, et al. Associations between retinal microvasculature/microstructure and renal function in type 2 diabetes patients with early chronic kidney disease. Diabetes Res Clin Pr. 2020;168:108373.
Ghamdi AHA. Clinical predictors of diabetic retinopathy progression; a systematic review. Curr Diabetes Rev. 2020;16:242–7.
Shinojima A, Lee D, Tsubota K, Negishi K, Kurihara T. Retinal diseases regulated by hypoxia—basic and clinical perspectives: a comprehensive review. J Clin Med. 2021;10:5496.
Li Y, Yu Y, VanderBeek BL. Anaemia and the risk of progression from non-proliferative diabetic retinopathy to vision threatening diabetic retinopathy. Eye. 2020;34:934–41.
Taderegew MM, Tewodros G, Abera TA, Woldeamanuel GG. Anemia and its associated factors among type 2 diabetes mellitus patients attending Debre Berhan referral hospital, North-East Ethiopia: a cross-sectional study. J Blood Med. 2020;11:47–58.
Faghir-Ganji M, Abdolmohammadi N, Nikbina M, Amanollahi A, Ansari-Moghaddam A, Rozhan R, et al. Prevalence of anemia in patients with diabetes mellitus: a systematic review and meta-analysis. Biomed Environ Sci. 2024;37:96–107.
Li X, Chen M. Correlation of hemoglobin levels with diabetic retinopathy in US adults aged ≥40 years: the NHANES 2005–2008. Front Endocrinol. 2023;14:1195647.
Wang J, Xin X, Luo W, Wang R, Wang X, Si S, et al. Anemia and diabetic kidney disease had joint effect on diabetic retinopathy among patients with type 2 diabetes. Invest Ophthalmol Vis Sci. 2020;61:25.
AlFalasi SM, Abdouli KA, Aldashti NA. Association of anemia and diabetic retinopathy among patients with type 2 diabetes mellitus: retrospective cross-sectional study. Cureus. 2024;16:e67995.
Dziedziak J, Zaleska-Żmijewska A, Szaflik JP, Cudnoch-Jędrzejewska A. Impact of arterial hypertension on the eye: a review of the pathogenesis, diagnostic methods, and treatment of hypertensive retinopathy. Med Sci Monit. 2022;28:e935135.
Liu L, Quang ND, Banu R, Kumar H, Tham Y-C, Cheng C-Y, et al. Hypertension, blood pressure control and diabetic retinopathy in a large population-based study. PLOS One. 2020;15:e0229665.
Liu Y, Li J, Ma J, Tong N. The threshold of the severity of diabetic retinopathy below which intensive glycemic control is beneficial in diabetic patients: estimation using data from large randomized clinical trials. J Diabetes Res. 2020;2020:8765139.
Shiferaw WS, Akalu TY, Desta M, Kassie AM, Petrucka PM, Assefa HK, et al. Glycated hemoglobin A1C level and the risk of diabetic retinopathy in Africa: a systematic review and meta-analysis. Diabetes Metab Syndr. 2020;14:1941–9.
Park JY, Hwang JH, Kang MJ, Sim HE, Kim JS, Ko KS. Effects of glycemic variability on the progression of diabetic retinopathy among patients with type 2 diabetes. Retina. 2021;41:1487–95.
Wermine K, Gotewal S, Song J, Huang LG, Corona KK, Chokshi SN, et al. Patterns of antibiotic administration in patients with burn injuries: a TriNetX study. Burns. 2024;50:52–8.
Hoskins M, Sefick S, Zurca AD, Walter V, Thomas NJ, Krawiec C. Current utilization of interosseous access in pediatrics: a population-based analysis using an EHR database, TriNetX. Int J Emerg Med. 2022;15:65.
Yendewa GA, Olasehinde T, Mulindwa F, Salata RA, Mohareb AM, Jacobson JM. Chronic hepatitis B and COVID-19 clinical outcomes in the United States: a multisite retrospective cohort study. Open Forum Infect Dis. 2025;12:ofaf013.
Ho CN, Sun CK, Wu JY, Chen JY, Chang YJ, Chen IW, et al. Association of vitamin D deficiency with post-stroke depression: a retrospective cohort study from the TriNetX US collaborative networks. Front Nutr. 2023;10:1236233.
Chen IW, Yu TS, Lai YC, Yang CP, Yu CH, Hung KC. Association between vitamin D deficiency and clinical outcome in patients with COVID-19 in the post-Omicron phase. Front Nutr. 2025;12:1583276.
Min J, Zeng T, Roux M, Lazar D, Chen L, Tudzarova S. The role of HIF1α-PFKFB3 pathway in diabetic retinopathy. J Clin Endocrinol Metab. 2021;106:2505–19.
Han N, Xu H, Yu N, Wu Y, Yu L. MiR-203a-3p inhibits retinal angiogenesis and alleviates proliferative diabetic retinopathy in oxygen-induced retinopathy (OIR) rat model via targeting VEGFA and HIF-1α. Clin Exp Pharm Physiol. 2020;47:85–94.
Atef MM, Shafik NM, Mostafa HY, Mohamed WM, Amal S, Shafik HM, et al. The evolving role of long noncoding RNA HIF1A-AS2 in diabetic retinopathy: a cross-link axis between hypoxia, oxidative stress and angiogenesis via MAPK/VEGF-dependent pathway. Redox Rep. 2022;27:70–8.
Yang J, Liu Z. Mechanistic pathogenesis of endothelial dysfunction in diabetic nephropathy and retinopathy. Front Endocrinol. 2022;13:816400.
Theuerle JD, Al-Fiadh AH, Amirul Islam FM, Patel SK, Burrell LM, Wong TY, et al. Impaired retinal microvascular function predicts long-term adverse events in patients with cardiovascular disease. Cardiovasc Res. 2020;117:1949–57.
Del Pinto R, Mulè G, Vadalà M, Carollo C, Cottone S, Agabiti Rosei C, et al. Arterial hypertension and the hidden disease of the eye: diagnostic tools and therapeutic strategies. Nutrients. 2022;14:2200.
Takahashi T, Iwasaki A. Sex differences in immune responses. Science. 2021;371:347–8.
Bradshaw JL, Vasini B, Mabry S, Hefley BS, Wilson EN, Gardner JJ, et al. Chronic intermittent hypoxia modulates corneal fibrotic markers and inflammatory cytokine expression in a sex-dependent manner. Exp Eye Res. 2025;255:110358.
Author information
Authors and Affiliations
Contributions
Kuo-Chuan Hung and Li-Chen Chang: Conceptualisation, Methodology, Software; Ying-Jen Chang and Chih-Wei Hsu: Data curation; Ming Yew and I-Wen Chen: Visualisation, Investigation; Jheng-Yan Wu: Supervision; I-Wen Chen: Software, Validation; Kuo-Chuan Hung and I-Wen Chen: Writing- Original draft preparation; Kuo-Chuan Hung and I-Wen Chen: Writing- Reviewing and Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The use of TriNetX in this study was approved by the Institutional Review Board of Chi Mei Medical Center (No. 11403-E01).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hung, KC., Chang, LC., Chang, YJ. et al. Association between haemoglobin levels and the risk of diabetic retinopathy in adults with type 2 diabetes: a retrospective cohort study using the TriNetX network. Eye 39, 2822–2829 (2025). https://doi.org/10.1038/s41433-025-03982-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-03982-0