Abstract
Background
Patients that have a hydrophilic intraocular lens (IOL) inserted during cataract surgery are more likely to develop posterior capsular opacification (PCO) and require YAG laser posterior capsulotomy than those with hydrophobic IOLs. This study aimed to examine the cost implications of hydrophilic and hydrophobic IOL usage in NHS-funded cataract services in England and estimate the cost saving of increased hydrophobic IOL usage.
Methods
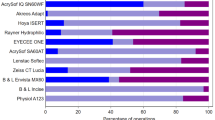
The cost of IOLs and YAG laser posterior capsulotomy was determined using NHS Spend Comparison Service data and Payment by Results tariffs. Data from the National Ophthalmology Database (NOD) audit was used to estimate PCO rates and the proportion of cataract cases that used hydrophilic and hydrophobic IOLs in England during the 2022 NHS year.
Results
The cumulative cost per case of purchasing an IOL and YAG laser posterior capsulotomy treatment over the 9-year period following cataract surgery was £148.73 (£96.83–£199.12) for hydrophilic IOLs and £107.58 (£62.99–£150.05) for hydrophobic IOLs. Of the cataract cases performed in England during the 2022 NHS year that were reported to the NOD, 52% used hydrophilic IOLs and 46% used hydrophobic IOLs. If all cases that used hydrophilic IOLs in England during the 2022 NHS year had instead used hydrophobic IOLs, the reduced need for YAG laser posterior capsulotomies could have saved around £13.0 million (£10.7 million–£15.6 million).
Conclusions
Hydrophilic IOLs remain popular amongst NHS-funded cataract services in England. Increasing hydrophobic IOL usage could be an effective strategy for lowering PCO rates while generating recurrent annual financial savings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Access to the data from Royal College of Ophthalmologists’ National Ophthalmology Database cataract audit can be accessed by application from appropriate academic or clinical organisations to noa.project@rcophth.ac.uk, however, preparation of the data would require a fee to cover full costs of extracting and preparing the necessary data for the intended purpose from the National Ophthalmology Database.
References
Donachie PHJ, Barnes B, Olaitan M, Buchan JC. National Ophthalmology Database Audit: seventh annual report of the National Cataract Audit. https://nodaudit.org.uk/sites/default/files/2024-05/NOD%20Cataract%20Audit%207th%20Annual%20Report%202024_1.pdf (2024).
Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114:1670–8.
Centre for Health and the Public Interest. Out of Sight—Understanding the Hidden Impact of Cataract Outsourcing on NHS Finances. https://static1.squarespace.com/static/665df1b730af0f34e4f4503b/t/67b4a33e57ec611c42e7ac3c/1739891519007/CHPI-OutOfSight-ReportVol1-Nov24-HighRes.pdf (2024).
Buchan JC, Norman P, Shickle D, Cassels-Brown A, MacEwen C. Failing to plan and planning to fail. Can we predict the future growth of demand on UK Eye Care Services?. Eye. 2019;33:1029–31.
UK Ophthalmology Alliance. How to choose an intraocular lens (IOL) in an NHS eye unit. https://uk-oa.co.uk/wp-content/uploads/2019/02/Procuring-IOLs-1-December-2018.pdf (2018).
Ting DSJ, Tatham AJ, Donachie PHJ, Buchan JC. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 16, influence of remuneration model on choice of intraocular lens in the UK. Eye. 2023;37:3854–60.
Donachie PHJ, Barnes BL, Olaitan M, Sparrow JM, Buchan JC. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: Report 9, risk factors for posterior capsule opacification. Eye. 2022;37:1633–9.
Zhao Y, Yang K, Li J, Huang Y, Zhu S. Comparison of hydrophobic and hydrophilic intraocular lens in preventing posterior capsule opacification after cataract surgery: an updated meta-analysis. Medicine. 2017;96:e8301.
Tokko HA, et al. Factors associated with the development of posterior capsule opacification requiring yttrium aluminum garnet capsulotomy. Optom Vis Sci. 2019;96:492–9.
Ekemiri K, et al. Global burden of fall and associated factors among individual with low vision: a systematic-review and meta-analysis. PLoS ONE. 2024;19:e0302428.
Xu S, et al. Social engagement and cognitive impairment among nursing home residents: the role of sensory impairment. Arch Gerontol Geriatr. 2024;122:105397.
Nguyen H, et al. Associations between vision impairment and vision-related interventions on crash risk and driving cessation: systematic review and meta-analysis. BMJ Open. 2023;13:e065210.
Cullin F, Busch T, Lundström M. Economic considerations related to choice of intraocular lens (IOL) and posterior capsule opacification frequency—a comparison of three different IOLs. Acta Ophthalmol. 2014;92:179–83.
Kossack N, et al. German claims data analysis to assess impact of different intraocular lenses on posterior capsule opacification and related healthcare costs. J Public Health. 2018;26:81–90.
Raulinajtys-Grzybek M, Grabska-Liberek I, Opala A, Słomka M, Chrobot M. Budget impact analysis of lens material on the posterior capsule opacification (PCO) as a complication after the cataract surgery. Cost Eff Resour Alloc. 2020;18:19.
National Institute for Health and Care Excellence. NICE guideline [NG77—cataracts in adults: management. https://www.nice.org.uk/guidance/ng77/chapter/recommendations (2017).
National Institute for Health and Care Excellence. NICE process and methods [PMG36]—NICE health technology evaluations: the manual. https://www.nice.org.uk/process/pmg36/chapter/economic-evaluation-2#the-reference-case-framework (2022).
Office for National Statistics. Life tables, principal projection, UK (2022-based edition of this dataset). https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/lifetablesprincipalprojectionunitedkingdom.
NHS England. 2023/25 NHS Payment Scheme: 2024/25 prices workbook. https://www.england.nhs.uk/publication/2023-25-nhs-payment-scheme/ (2023).
Georgiou A, Ruston J, Haque S, Woollard A. Accuracy and remunerative implications of clinical coding in elective plastic surgery. Bulletin. 2022;104:190–4.
Medical Research Council, NHS Health Research Authority. Do I need NHS REC review? https://www.hra-decisiontools.org.uk/ethics/ (2020).
Fight for Sight. Time to Focus. https://www.fightforsight.org.uk/media/voaj1bxm/time-to-focus-report.pdf (2020).
Auffarth G, LaHood B. Letter to the editor—hydrophilic acrylic IOLs. EuroTimes. 2023;28:5. https://www.escrs.org/eurotimes-articles/hydrophilic-acrylic-iols/.
Grzybowski A, Zemaitiene R, Markeviciute A, Tuuminen R. Should we abandon hydrophilic intraocular lenses?. Am J Ophthalmol. 2022;237:139–45.
Nanavaty MA. Hydrophobic versus hydrophilic acrylic intraocular lenses within public sector based on the type of funding contacts: the debate continues. Eye. 2023;37:3712–3.
Brézin AP, et al. Incidence of Nd:YAG laser capsulotomy following cataract surgery: a population-based nation-wide study—FreYAG1 study. BMC Ophthalmol. 2023;23:417.
Acknowledgements
We acknowledge with thanks the contribution of Professor John Sparrow who provided diligent clinical and academic oversight and leadership of the RCOphth NOD over many years to bring it to its current stature. It is with gratitude that we remember our friend and colleague Robert Johnston, who sadly died in September 2016. Without his inspirational vision, determination and career long commitment to quality improvement in ophthalmology, this work would not have been possible. We acknowledge the support of the hospitals that participated in this National Ophthalmology Database Audit study and thank our medical and non-medical colleagues for the considerable time and effort devoted to conscientious electronic data collection as they go about caring for their patients.
Funding
The RCOphth National Ophthalmology Database Cataract Audit is currently funded through participation fees from centres as well as unrestricted financial contributions from Alcon and Bausch and Lomb.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design and data collection. JM produced first draft and final manuscript. All authors offered comments and agreed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Malcolm, J., Donachie, P.H.J., Hernández, R. et al. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 20, the hidden cost of intraocular lens choices for National Health Service funded cataract surgery in England. Eye 39, 3142–3147 (2025). https://doi.org/10.1038/s41433-025-04033-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04033-4