Abstract
Objective
To investigate histopathological conjunctival changes associated with topical netarsudil 0.02%.
Methods
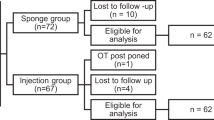
Observational comparative case series. Histopathological analysis of conjunctival specimens taken from adult patients undergoing glaucoma surgery. Inflammation score was graded by three independent pathologists.
Results
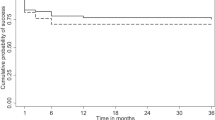
29 samples were included for analysis. Mean age was 72.4 years and 44.8% were female. Most patients underwent trabeculectomy with mitomycin C (22/29, 76%) while the remainder underwent tube shunt surgery, and one patient underwent insertion of an experimental NT-501 intravitreal implant. All patients were taking ≥2 topical IOP lowering medications, and 12 patients (41.3%) were using topical netarsudil, with mean duration 26.8 months. Compared to those on other glaucoma medications, patients taking netarsudil had significantly thicker conjunctival epithelium (mean 90.1 µm vs 43.2 µm, p = 0.03) and a trend toward higher epithelial cell thickness count (mean 7.7 cells thick vs. 4.9 cells thick, p = 0.07), both of which remained significant and trending respectively when adjusted for confounders (p = 0.02 and p = 0.06). All netarsudil treated samples demonstrated inflammation (graded score ≥0.5) compared to 64.7% of those not on netarsudil (p = 0.03). There were no significant differences in any histopathological parameters in patients who had ceased netarsudil prior to analysis (n = 7) compared to those who had never taken netarsudil (p > 0.05 for all).
Conclusion
Conjunctiva treated with netarsudil may be more likely to demonstrate inflammation compared to those treated with other combinations of glaucoma medications. These findings may have surgical implications and additional studies correlating clinical outcomes are required.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Serle JB, Katz LJ, McLaurin E, Heah T, Ramirez-Davis N, Usner DW, et al. Two phase 3 clinical trials comparing the safety and efficacy of netarsudil to timolol in patients with elevated intraocular pressure: Rho kinase elevated IOP treatment trial 1 and 2 (ROCKET-1 and ROCKET-2). Am J Ophthalmol. 2018;186:116–27.
Tokushige H, Inatani M, Nemoto S, Sakaki H, Katayama K, Uehata M, et al. Effects of topical administration of y-39983, a selective rho-associated protein kinase inhibitor, on ocular tissues in rabbits and monkeys. Investig Ophthalmol Vis Sci. 2007;48:3216–22.
Wang RF, Williamson JE, Kopczynski C, Serle JB. Effect of 0.04% AR-13324, a ROCK, and norepinephrine transporter inhibitor, on aqueous humor dynamics in normotensive monkey eyes. J Glaucoma. 2015;24:51–54.
Rao PV, Pattabiraman PP, Kopczynski C. Role of the Rho GTPase/Rho kinase signaling pathway in pathogenesis and treatment of glaucoma: Bench to bedside research. Exp Eye Res. 2017;158:23–32.
Kazemi A, McLaren JW, Kopczynski CC, Heah TG, Novack GD, Sit AJ. The effects of netarsudil ophthalmic solution on aqueous humor dynamics in a randomized study in humans. J Ocul Pharm Ther. 2018;34:380–6.
Okumura N, Kinoshita S, Koizumi N. Application of Rho kinase inhibitors for the treatment of corneal endothelial diseases. J Ophthalmol. 2017;2017:2646904.
Lindstrom RL, Lewis AE, Holland EJ, Sheppard JD, Hovanesian JA, Senchyna M, et al. Phase 2, randomized, open-label parallel-group study of two dosing regimens of netarsudil for the treatment of corneal edema due to Fuchs corneal dystrophy. J Ocul Pharm Ther. 2022;38:657–63.
Kusuhara S, Nakamura M. Ripasudil hydrochloride hydrate in the treatment of glaucoma: safety, efficacy, and patient selection. Clin Ophthalmol. 2020;14:1229–36.
Singh IP, Fechtner RD, Myers JS, Kim T, Usner DW, McKee H, et al. Pooled efficacy and safety profile of netarsudil ophthalmic solution 0.02% in patients with open-angle glaucoma or ocular hypertension. J Glaucoma. 2020;29:878–84.
Francis BA, Du LT, Najafi K, Murthy R, Kurumety U, Rao N, et al. Histopathologic features of conjunctival filtering blebs. Arch Ophthalmol. 2005;123:166–70.
Broadway D, Grierson I, Hitchings R. Adverse effects of topical antiglaucomatous medications on the conjunctiva. Br J Ophthalmol. 1993;77:590–6.
Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. I. The conjunctival cell profile. Arch Ophthalmol. 1994;112:1437–45.
Sherwood MB, Grierson I, Millar L, Hitchings RA. Long-term morphologic effects of antiglaucoma drugs on the conjunctiva and Tenon’s capsule in glaucomatous patients. Ophthalmology. 1989;96:327–35.
Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma. 2001;10:237–49.
Baudouin C, Garcher C, Haouat N, Bron A, Gastaud P. Expression of inflammatory membrane markers by conjunctival cells in chronically treated patients with glaucoma. Ophthalmology. 1994;101:454–60.
Dogan AS, Orhan M, Soylemezoglu F, Irkec M, Bozkurt B. Effects of topical antiglaucoma drugs on apoptosis rates of conjunctival epithelial cells in glaucoma patients. Clin Exp Ophthalmol. 2004;32:62–66.
Leary KA, Lin KT, Steibel JP, Harman CD, Komaromy AM. Safety and efficacy of topically administered netarsudil (Rhopressa) in normal and glaucomatous dogs with ADAMTS10-open-angle glaucoma (ADAMTS10-OAG). Vet Ophthalmol. 2021;24:75–86.
Hu E, Lee D. Rho kinase as potential therapeutic target for cardiovascular diseases: opportunities and challenges. Expert Opin Ther Targets. 2005;9:715–36.
Blondeau P, Rousseau JA. Allergic reactions to brimonidine in patients treated for glaucoma. Can J Ophthalmol. 2002;37:21–26.
Yeh PH, Cheng YC, Shie SS, Lee YS, Shen SC, Chen HS, et al. Brimonidine related acute follicular conjunctivitis: onset time and clinical presentations, a long-term follow-up. Medicine. 2021;100:e26724.
Funding
KS is a consultant for: Alcon, Allergan, Glaukos, Ivantis, Santen and Sight Sciences. The sponsor or funding organisations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
MTS was responsible for the study design, recruitment, data analysis and drafting of the manuscript. CC, JL and DSM were responsible for the histopathological protocol and review, and approval of the final manuscript. KS was responsible for the study conception, design, oversight and approval of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, M.T., Charoenkijkajorn, C., Lin, J.H. et al. Conjunctival histopathological changes associated with netarsudil 0.02%. Eye 39, 3278–3283 (2025). https://doi.org/10.1038/s41433-025-04063-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-025-04063-y