Abstract
Purpose
To assess prevalence and associations of active central serous chorioretinopathy (CSC) and inactive CSC/pachychoroid pigment epitheliopathy (PPE) in a general population aged 50+ years.
Methods
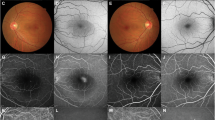
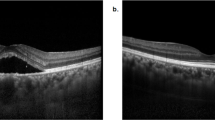
Using optical coherent tomographic images, we assessed CSC lesions in participants of the population-based Beijing Eye Study. We differentiated between active CSC with subretinal fluid, and inactive CSC/PPE with retinal pigment epithelium irregularities and dilated large choroidal vessels and without subretinal fluid.
Results
Out of 6551 eyes, CSC/PPE was detected in 98 eyes (70 participants; 60 (86%) men) (prevalence: 1.5%; 95%CI: 1.1, 1.9), with active CSC (with/without inactive CSC/PPE) in 52 eyes (53%) and inactive CSC/PPE (with/without an active component) in 66 eyes (67%). CSC location was only foveal in 21 (21%) eyes, only extrafoveal in 44 (45%) eyes, and mixed in 33 (34%) eyes. CSC occurred bilaterally in 28 patients (56 (57%) eyes). Both eyes of all CSC patients (also those with unilateral CSC) showed markedly dilated large choroidal vessels. CSC lesion number ranged between 1 and 13 (mean:2.5 ± 2.2) per eye. Higher CSC prevalence was associated with younger age (OR: 0.95; 95%CI: 0.91, 0.99; P = 0.01), male sex (OR: 4.16; 95% CI: 1.92, 9.02; P < 0.001), thicker subfoveal choroid (OR: 1.004; 95% CI: 1.001, 1.007; P = 0.01), and higher prevalences of retinal outer nuclear layer thinning (OR: 4.08; 95% CI: 1.25, 13.3; P = 0.02), intraretinal hyperreflective foci (iHRFs) beyond the ellipsoid zone (OR: 7.11; 95% CI: 3.21, 15.8; P < 0.001), macular hypopigmentations (OR: 1.55; 95% CI: 1.30, 1.85; P < 0.001), and incomplete retinal pigment epithelium and outer retinal atrophy (iRORA) (OR: 12.3; 95% CI: 2.97, 51.1; P < 0.001).
Conclusions
Active CSC and inactive CSC/PPE together were relatively frequent in a general population consisting of Han Chinese from the Beijing region and aged 50+ years. They occurred often multifocal and were often extrafoveally located.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
All data are available upon reasonable request from the corresponding author.
References
Fung AT, Yang Y, Kam AW. Central serous chorioretinopathy: a review. Clin Exp Ophthalmol. 2023;51:243–70.
Khan AH, Lotery AJ. Central serous chorioretinopathy: epidemiology, genetics and clinical features. Annu Rev Vis Sci. 2024;10:477–505.
Kaye R, Chandra S, Sheth J, Boon CJF, Sivaprasad S, Lotery A. Central serous chorioretinopathy: an update on risk factors, pathophysiology and imaging modalities. Prog Retin Eye Res. 2020;79:100865.
Kido A, Miyake M, Tamura H, Hiragi S, Kimura T, Ohtera S, et al. Incidence of central serous chorioretinopathy (2011-2018): a nationwide population-based cohort study of Japan. Br J Ophthalmol. 2022;106:1748–53.
Fakhril-Din Z, Arnold-Vangsted A, Boberg-Ans LC, Anguita R, Desideri LF, van Dijk EHC, et al. Is tobacco consumption a risk factor for central serous chorioretinopathy? A systematic review and meta-analysis. Acta Ophthalmol. 2024 Oct 18. https://doi.org/10.1111/aos.16782. Online ahead of print.
Chen YY, Huang LY, Liao WL, Chou P. Association between central serous chorioretinopathy and risk of depression: a population-based cohort study. J Ophthalmol. 2019;2019:2749296.
Carvalho-Recchia CA, Yannuzzi LA, Negrão S, Spaide RF, Freund KB, Rodriguez-Coleman H, et al. Corticosteroids and central serous chorioretinopathy. Ophthalmology. 2002;109:1834–7.
Kang HG, Woo SJ, Lee JY, Cho HJ, Ahn J, Yang YS, et al. Pathogenic risk factors and associated outcomes in the bullous variant of central serous chorioretinopathy. Ophthalmol Retina. 2022;6:939–48.
Hsu CC, Chen YH, Huang KH, Chen J, Chung CH, Liang CM, et al. The correlation of central serous chorioretinopathy and subsequent cardiovascular diseases of different types: a population-based cohort study. Int J Environ Res Public Health. 2019;16:5099.
Liu PK, Chang YC, Tai MH, Tsai RK, Chong IW, Wu KY, et al. the association between central serious chorioretinopathy and sleep apnea: a nationwide population-based study. Retina. 2020;40:2034–44.
Chang YS, Weng SF, Wang JJ, Jan RL. Increased risk of central serous chorioretinopathy following end-stage renal disease: a nationwide population-based study. Medicine. 2019;98:e14859.
Hsu CC, Chen YH, Huang KH, Chen J, Chung CH, Liang CM, et al. Evaluation of the relationship between central serous chorioretinopathy and liver cirrhosis: a nationwide, population-based study. J Chin Med Assoc. 2021;84:655–63.
Piccolino FC, Fruttini D, Eandi C, Nicolò M, Mariotti C, Tito S, et al. Vigorous physical activity as a risk factor for central serous chorioretinopathy. Am J Ophthalmol. 2022;244:30–37.
Yagi M, Miyake M, Mori Y, Hosoda Y, Takahashi A, Muraoka Y, et al. Natural course of pachychoroid pigment epitheliopathy. Ophthalmol Sci. 2022;2:100201.
Huang YT, Wan L, Cheng YD, Yu TS, Hung YT, Rujikajorn K, et al. Increased risk of glaucoma development in patients with central serous chorioretinopathy: results of a 11-year population-based cohort study. Graefes Arch Clin Exp Ophthalmol. 2023;261:3457–64.
Spaide RF, Fisher YL, Ngo WK, Barbazetto I. Regional scleral thickness as a risk factor for central serous chorioretinopathy. Retina. 2022;42:1231–7.
Spaide RF, Gemmy Cheung CM, Matsumoto H, Kishi S, Boon CJF, van Dijk EHC, et al. Venous overload choroidopathy: a hypothetical framework for central serous chorioretinopathy and allied disorders. Prog Retin Eye Res. 2022;86:100973.
Imanaga N, Terao N, Nakamine S, Tamashiro T, Wakugawa S, Sawaguchi K, et al. Scleral thickness in central serous chorioretinopathy. Ophthalmol Retina. 2021;5:285–91.
Imanaga N, Terao N, Sonoda S, Sawaguchi S, Yamauchi Y, Sakamoto T, et al. Relationship between scleral thickness and choroidal structure in central serous chorioretinopathy. Investig Ophthalmol Vis Sci. 2023;64:16.
Jonas JB, Panda-Jonas S, Xu J, Jonas RA, Wang YX. Prevalence and associations of the three-layer sign in age-related macular degeneration. The Beijing eye study. Acta Ophthalmol. 2025 Sep 19. https://doi.org/10.1111/aos.70004. Online ahead of print. PMID: 40970575
Jonas JB, Wang N, Wang YX, You QS, Xie XB, Yang D, et al. Subfoveal choroidal thickness and cerebrospinal fluid pressure. The Beijing Eye Study 2011. Investig Ophthalmol Vis Sci. 2014;55:1292–8.
Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burke JP. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980–2002. Ophthalmology. 2008;115:169–73.
Schatz H, Madeira D, Johnson RN, McDonald HR. Central serous chorioretinopathy occurring in patients 60 years of age and older. Ophthalmology. 1992;99:63–67.
Spaide RF, Campeas L, Haas A, Yannuzzi LA, Fisher YL, Guyer DR, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996;103:2070–9.
Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol. 2013;58:103–26.
Todd KC, Hainsworth DP, Lee LR, Madsen RW. Longitudinal analysis of central serous chorioretinopathy and sex. Can J Ophthalmol. 2002;37:405–8.
Ersoz MG, Arf S, Hocaoglu M, Sayman Muslubas I, Karacorlu M. Patient characteristics and risk factors for central serous chorioretinopathy: an analysis of 811 patients. Br J Ophthalmol. 2019;103:725–9.
Yoneyama S, Fukui A, Sakurada Y, Terao N, Shijo T, Kusada N, et al. Distinct characteristics of central serous chorioretinopathy according to gender. Sci Rep. 2022;12:10565.
Hanumunthadu D, Van Dijk EHC, Gangakhedkar S, Goud A, Cheung CMG, Cherfan D, et al. Gender variation in central serous chorioretinopathy. Eye. 2018;32:1703–9.
Sahoo NK, Ong J, Selvam A, Brown R, Avdalimov M, Kulkarni A, et al. Gender differences in central serous chorioretinopathy based on the new multimodal imaging classification. Eye. 2024;38:964–7.
Jonas JB, Wang N, Yang D, Ritch R, Panda-Jonas S. Facts and myths of cerebrospinal fluid pressure for the physiology of the eye. Prog Retin Eye Res. 2015;46:67–83.
Vurgese S, Panda-Jonas S, Jonas JB. Scleral thickness in human eyes. PLoS One. 2012;7:e29692.
Fujiwara T, Imamura Y, Margolis R, Slakter JS, Spaide RF. Enhanced depth imaging optical coherence tomography of the choroid in highly myopic eyes. Am J Ophthalmol. 2009;148:445–50.
Li Y, You QS, Wei WB, Xu J, Chen CX, Wang YX, et al. Prevalence and associations of central serous chorioretinopathy in elderly Chinese. The Beijing Eye Study 2011. Acta Ophthalmol. 2016;94:386–90.
Hasan N, Zarnegar A, Jacob N, Sahoo N, Saju S, Zhou A, et al. Clinical characteristics and progression of pachychoroid macular atrophy in central serous chorioretinopathy. Ophthalmol Retina. 2025;9:984–93.
Funding
National Natural Science Foundation of China (82271086). The funder of this study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SP-J, RAJ, JBJ: European patent EP 3 271 392, JP 2021-119187, and U.S. Patent No. US 12,024,557 B2: “Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia; European patent application 23196899.1”. EGFR Antagonists for the treatment of diseases involving unwanted migration, proliferation, and metaplasia of RPE cells.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jonas, J.B., Panda-Jonas, S., Xu, J. et al. Prevalence and associations of central serous chorioretinopathy in a population aged 50+ years. The Beijing Eye Study. Eye (2026). https://doi.org/10.1038/s41433-026-04269-8
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41433-026-04269-8