Abstract
Hereditary ataxias are classified by inheritance patterns into autosomal dominant, autosomal recessive, X-linked, and mitochondrial modes of inheritance. A large group of adult hereditary ataxias have autosomal dominant inheritance, and autosomal recessive cerebellar ataxias (ARCAs) are rare, with greater diversity in phenotypic and genotypic features. Therefore, comprehensive genetic testing is useful for identifying the genes responsible for ARCAs. We identified two novel pathogenic variants of the SQSTM1 and SYNE1 genes via whole-exome sequencing in patients with ARCAs.
Similar content being viewed by others
Hereditary ataxias are classified into autosomal dominant, autosomal recessive, X-linked, and maternal inheritance types on the basis of their type of inheritance1. The diagnosis of hereditary ataxia can be established on the basis of typical neurological findings, a positive family history, and the exclusion of nongenetic ataxias1. Autosomal recessive cerebellar ataxias (ARCAs) are complex neurodegenerative disorders with highly diverse phenotypes and genotypes2. ARCAs are considered to be early-onset3, unlike the autosomal dominant types, among which the age of onset overlaps1. Various genes have been reported to be responsible for different subtypes of ARCAs, with Friedreich’s ataxia (FRDA gene) and ataxia telangiectasia (ATM gene) being the most common4. Although most ARCAs can be distinguished by unique clinical features, definitive diagnosis is challenging because of overlapping phenotypes5. Therefore, it is necessary to use genetic diagnostic methods to identify the different genes responsible for various ARCAs. Over 90 genes have been reported to be associated with ARCAs6.
Compared with traditional techniques, next-generation DNA sequencing (NGS) techniques are very powerful, affordable, and fast diagnostic tools for determining the genetic causes of neurological disorders such as ataxia7. Recognizing gene defects is a major step in detecting different molecular pathways and is an important prerequisite for the development of effective targeted molecular therapies8. Therefore, this study aimed to identify the genes and mutations associated with autosomal recessive ataxia in two families with consanguineous marriages in Iran. In this study, owing to the diverse phenotypic and genotypic features of patients with ARCAs, whole-exome sequencing (WES, an NGS-based test) was used as an appropriate method for identifying the genetic basis of Mendelian disorders of unknown etiology9,10.
This study was approved by the Ethics Committee of the Ardabil University of Medical Sciences (IR.ARUMS.REC.1402.019), and written consent was obtained from the parents. All parents were phenotypically normal. Pedigrees were drawn, and the patients underwent neurological examinations, laboratory tests, and MRIs. Nongenetic causes were ruled out. A peripheral blood sample was obtained, high-quality DNA was extracted via the standard salting-out method, and sample preparation was performed. An Agilent Human All Exon Kit was used for exome enrichment of total genomic DNA, and paired-end sequencing was performed via an Illumina HiSeq sequencer. The functional annotation of identified variants was performed via the ANNOVAR tool. Neutral and previously reported variants with a frequency of 1% or above were filtered out from further analysis. Whole-exome sequencing revealed two novel variants in the SQSTM1 and SYNE1 genes.
The proband in family I is a 50-year-old female with ataxia who was born in a family with consanguineous marriage (Fig. 1a). The birth measurements were normal. She started to sit, crawl, and walk on time and had normal development until 7 years of age. Symptoms started with speech delay at the age of 7 and a few months later with unsteady gait and ataxia. She has experienced cognitive decline; however, it was categorized as mild. Currently, the patient can walk short distances and eat food without assistance. She follows orders and can communicate with words and small phrases. Vertical gaze palsy is present, but dystonia was not detected. She has not experienced any seizures; however, her brother suffers from intellectual disability and epilepsy with no ataxia. Brain MRI revealed mild cerebellar atrophy.
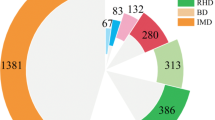
a Pedigree of the proband in Family I. b Sequencing results of Family I (SQSTM1 gene). c Schematic diagram of the sequestosome-1 protein and location of the p.Arg22Pro mutation. d Evolutionary conservation analysis of arginine amino acids in different species (human: Homo sapiens, Orangutan: Pongo abelii, mouse: Mus musculus, rat: Rattus norvegicus, Pig: Sus scrofa, whale: Physeter microcephalus, chicken: Gallus gallus, fish: Gadus morhua, frog: Xenopus laevis, lizard: Anolis carolinensis), e predicted structure of wild-type and mutant proteins via the DynaMut-2 web server.
The WES results revealed that the proband was homozygous for (NM_003900.5) c.65G > C, p.Arg22Pro in the SQSTM1 gene (Fig. 1b, c). This mutation replaces the amino acid arginine with proline. Conservation analysis revealed that the arginine amino acid at this position is highly conserved across ten different species (Fig. 1d). The DynaMut2 web server was used to predict the structure of the wild-type and mutant proteins (Fig. 1c). On the basis of the ACMG guidelines, this variant was categorized as “likely pathogenic” (PM1, PM2, PP3 and PP4). Pathogenic mutations in the SQSTM1 gene are associated with childhood-onset neurodegeneration with ataxia, dystonia, and gaze palsy (NADGP) (OMIM: 617145). This phenotypic spectrum was first defined by Haack et al. in 2016. Previously reported pathogenic variants and their clinical manifestations are listed in Table S1.
The proband in Family II is a 36-year-old woman with ataxia in a family with a consanguineous marriage (Fig. 2a). She was born via normal vaginal delivery. Her sitting, walking, and growth were normal, and she had a normal childhood. The first symptoms started at the age of 25, with difficulty maintaining balance and respiratory distress, and her symptoms worsened over time. Currently, the proband has spasticity of the lower limbs, muscle atrophy, difficulty breathing, and dysarthria. She cannot move or stand without assistance. She can say words and small phrases but not full sentences. Visual symptoms were not present. Brain magnetic resonance imaging (MRI) revealed cerebellar atrophy, and spine and neck MRI results revealed decreased neck lordosis. She has two brothers and one sister with identical symptoms that began in the third decade of their life, and two of them are deceased.
WES revealed a novel homozygous mutation of cytosine to thymine (NM_182961.4): c.21313C > T, p.Arg7105Ter in the SYNE1 gene (Fig. 2b, c), creating a premature stop codon. On the basis of the ACMG guidelines, the Franklin website classified this variant as “pathogenic” (PVS1, PM2 and PP4). Pathogenic mutations in SYNE1 are associated with spinocerebellar ataxia, autosomal recessive 8 (SCAR8) (OMIM: 610743).
Childhood-onset neurodegeneration with ataxia, dystonia, and gaze palsy (NADGP) is a progressive disorder with three characteristics: gait ataxia, cognitive decline, and gaze palsy11. Studies have shown that symptoms usually start between 6 and 15 years of age with ataxia, but in this case, it started with dysarthria. Vertical gaze palsy and dystonia are reported to be common manifestations in these patients11,12; however, dystonia has been reported in only 50% of the cases thus far, and in the current case, dystonia was not detected.
SQSTM1 is located on chromosome 5q35.3 and synthesizes an NM_003900.5 mRNA with 8 exons, which is responsible for synthesizing the sequence-1 protein with 440 amino acids13,14. This protein is responsible for modulating enzyme function through several domain interactions and has an essential role in the degradation of protein molecules15. The PB1 domain is necessary for localization into ubiquitin-containing inclusion bodies and interacts with many other proteins16,17. Recently, it has been shown that the PB1 domain is essential for the formation of stable large multiprotein complexes18. Previous studies have shown that neurodegeneration can be due to defects in autophagy, mitochondrial function, and ubiquitin–proteasomal degradation pathways19. We identified a homozygous mutation, NM_003900.5: c.65G > C, p.Arg22Pro, in the SQSTM1 gene. This mutation replaces the arginine amino acid with proline and is located in the PB1 domain of this protein. The DynaMut2 web server predicted this mutation to be destabilizing (predicted stability change = ΔΔG −0.43 kcal/mol). The arginine amino acid in the wild-type protein has a greater interaction frequency with chain B than the proline amino acid in the mutant protein does, and this change could destabilize the protein structure and change its function. This variant was identified for the first time.
Autosomal recessive spinocerebellar ataxia-8 (SCAR8) is an autosomal recessive and neurodegenerative disorder that often has late onset and slow progression and was first identified in individuals from Beauce in Quebec20,21. This ataxia is usually progressive cerebellar ataxia with rare and mild extracerebellar symptoms in adulthood and leads to gait ataxia, lower and upper motor neuron disease, brainstem dysfunction, and musculoskeletal abnormalities20. Recent studies have suggested that SYNE1 ataxia is a complex multisystemic syndrome that is common worldwide22. In our case, the proband in family II had typical symptoms similar to those of previously reported patients, in addition to the loss of cervical lordosis. There were four individuals in this family with ataxia, and only one of them was genetically assessed; all four had late-onset ataxia.
SYNE1, located on chromosome 6q25.2 and containing 146 exons, is an enormous gene that encodes a 27,708-bp long mRNA, NM_182961.4, that is converted into a protein with 8797 amino acids called nesprin-119,20. As a structural protein of spectrin, this protein is involved in connecting the plasma membrane to the actin cytoskeleton23. Nesprin-1 is expressed in different tissues and significantly expressed in striated muscles and the cerebellum24. The molecular etiology of these symptoms is not fully understood. However, Razafsky et al. proposed that the pathogenicity of these mutations originates from dysfunctions of KASH-LESS variants of the giant Nesprin1 isoform, which is specifically expressed in the central nervous system25. Our proband was homozygous for the pathogenic variant NM_182961.4:c.21313C > T, p.Arg7105Ter in exon 116 of SYNE1, which creates a premature stop codon. Previous studies have shown that nonsense and frameshift mutations in the SYNE1 gene lead to nonsense-mediated decay of the mRNA20,21. This variant was identified for the first time.
HGV database
The relevant data from this Data Report are hosted at the Human Genome Variation Database at https://doi.org/10.6084/m9.figshare.hgv.3433; https://doi.org/10.6084/m9.figshare.hgv.3436.
References
Jayadev, S. & Bird, T. D. Hereditary ataxias: overview. Genet. Med. 15, 673–683 (2013).
Vermeer, S. et al. Autosomal recessive cerebellar ataxias: the current state of affairs. J. Med. Genet. 48, 651–659 (2011).
Palau, F. & Espinós, C. Autosomal recessive cerebellar ataxias. Orphanet J. Rare Dis. 1, 1–19 (2006).
Phang, M. W. L. et al. Therapeutic roles of natural remedies in combating hereditary ataxia: a systematic review. Chin. Med. 16, 1–22 (2021).
Fogel, B. L. & Perlman, S. Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol. 6, 245–257 (2007).
Beaudin, M. et al. The classification of autosomal recessive cerebellar ataxias: a consensus statement from the society for research on the cerebellum and ataxias task force. Cerebellum 18, 1098–1125 (2019).
Sailer, A. & Houlden, H. Recent advances in the genetics of cerebellar ataxias. Curr. Neurol. Neurosci. Rep. 12, 227–236 (2012).
Synofzik, M. & Németh, A. H. Recessive ataxias. Handb. Clin. Neurol. 155, 73–89 (2018).
Hajjari, M. et al. Exome sequencing found a novel homozygous deletion in ADCK3 gene involved in autosomal recessive spinocerebellar ataxia. Gene 708, 10–13 (2019).
Faruq, M. et al. Novel mutations in typical and atypical genetic loci through exome sequencing in autosomal recessive cerebellar ataxia families. Clin. Genet. 86, 335–341 (2014).
Haack, T. B. et al. Absence of the autophagy adaptor SQSTM1/p62 causes childhood-onset neurodegeneration with ataxia, dystonia, and gaze palsy. Am. J. Hum. Genet. 99, 735–743 (2016).
Muto, V. et al. Biallelic SQSTM1 mutations in early-onset, variably progressive neurodegeneration. Neurology 91, e319–e330 (2018).
Kent, W. J. et al. The human genome browser at UCSC. Genome Res. 12, 996–1006 (2002).
The UniProt Consortium. UniProt: the Universal Protein Knowledgebase in 2023. Nucleic Acids Res. 51, D523–D531 (2023).
Ma, S., Attarwala, I. Y. & Xie, X. Q. SQSTM1/p62: a potential target for neurodegenerative disease. ACS Chem. Neurosci. 10, 2094–2114 (2019).
Lamark, T. et al. Interaction codes within the family of mammalian Phox and Bem1p domain-containing proteins. J. Biol. Chem. 278, 34568–34581 (2003).
Wilson, M. I., Gill, D. J., Perisic, O., Quinn, M. T. & Williams, R. L. PB1 domain-mediated heterodimerization in NADPH oxidase and signaling complexes of atypical protein kinase C with Par6 and p62. Mol. Cell. 12, 39–50 (2003).
Alcober‐Boquet, L. et al. The PB1 and the ZZ domain of the autophagy receptor p62/SQSTM1 regulate the interaction of p62/SQSTM1 with the autophagosome protein LC3B. Protein Sci. 33, e4840 (2024).
Vedartham, V. et al. Homozygous sequestosome 1 (SQSTM1) mutation: a rare cause for childhood-onset progressive cerebellar ataxia with vertical gaze palsy. Ophthalmic Genet. 40, 376–379 (2019).
Synofzik, M. et al. SYNE1 ataxia is a common recessive ataxia with major non-cerebellar features: a large multi-centre study. Brain 139, 1378–1393 (2016).
Gros-Louis, F. et al. Mutations in SYNE1 lead to a newly discovered form of autosomal recessive cerebellar ataxia. Nat. Genet. 39, 80–85 (2007).
Coutelier, M. et al. Efficacy of exome-targeted capture sequencing in detecting mutations in known cerebellar ataxia genes. JAMA Neurol. 75, 591–599 (2018).
Nadaf, S. N., Chakor, R. T., Kothari, K. V. & Mannan, A. U. Synaptic nuclear envelope protein 1 (SYNE 1) ataxia with amyotrophic lateral sclerosis-like presentation: a novel synaptic nuclear envelope protein 1 (SYNE 1) gene deletion mutation in India. Ann. Indian Acad. Neurol. 23, 539 (2020).
King, S. J. et al. Nesprin‐1 and nesprin‐2 regulate endothelial cell shape and migration. Cytoskeleton 71, 423–434 (2014).
Razafsky, D. & Hodzic, D. A variant of Nesprin1 giant devoid of KASH domain underlies the molecular etiology of autosomal recessive cerebellar ataxia type I. Neurobiol. Dis. 78, 57–67 (2015).
Author information
Authors and Affiliations
Contributions
B.D. conceived and supervised the study and revised the manuscript. D.M. and M.J. contributed to the laboratory work. D.M., M.J., N.J., H.A., S.D., H.M. and S.A. prepared the manuscript, images, and table. V.A. and R.M. were in charge of the patients’ clinical management and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mokhtari, D., Jahanpanah, M., Jabbari, N. et al. Genetic investigation of patients with autosomal recessive ataxia and identification of two novel variants in the SQSTM1 and SYNE1 genes. Hum Genome Var 11, 35 (2024). https://doi.org/10.1038/s41439-024-00292-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41439-024-00292-x