Abstract
We investigated changes in blood pressure (BP) and metabolic adverse effects, especially elevation of uric acid (UA), after treatment with a thiazide-like diuretic (TD) in patients with essential hypertension. Furthermore, the role of genetic factors in the elevation of UA by TD was assessed by a 500 K SNP DNA microarray. The subjects included 126 hypertensive patients (57 women and 69 men, mean age 59 ± 12 years) who registered for the GEANE (Gene Evaluation for ANtihypertensive Effects) study. After one month of the nontreatment period, TD, indapamide, angiotensin II receptor antagonist valsartan, and Ca channel blocker amlodipine were administered to all patients for 3 months each in a randomized crossover manner. BP, renal function, serum UA level, and electrolytes were measured at baseline and at the end of each treatment period. Single nucleotide polymorphisms (SNPs) associated with UA elevation after treatment with indapamide were investigated by a genome-wide association study (GWAS). Indapamide significantly decreased both office and home BP levels. Treatment with indapamide also significantly reduced the estimated glomerular filtration rate and serum potassium and increased serum UA. Patients whose UA level increased more than 1 mg/dl showed significantly higher baseline office SBP and plasma glucose and showed greater decline in renal function compared with those who showed less UA increase (<1 mg/dl). Some SNPs strongly associated with an increase in UA after treatment with indapamide were identified. This study is the first report on SNPs associated with UA elevation after TD treatment. This information may be useful for the prevention of adverse effects after treatment with TD.
Similar content being viewed by others
Introduction
The blood pressure (BP) control status of hypertensive patients remains insufficient [1]. The mean salt intake still exceeds 10 g/day in Japan [2], and salt-sensitive hypertension is frequent. Thus, thiazide diuretics are recommended as the first-line antihypertensive drugs or as a combination therapy to achieve target BP levels in the Japanese guidelines for hypertension (JSH 2014) [3] and the recent AHA/ACC [4] and ESH/ESC guidelines for hypertension [5]. Antihypertensive treatment with thiazide diuretics reduces cardiovascular risk [6, 7]; however, the adverse effects of diuretics, including electrolyte abnormalities such as hypokalemia and unfavorable disorders on metabolic parameters, such as impaired glucose tolerance and hyperuricemia, are frequently observed. An elevation of uric acid (UA) not only leads to gout but also the development and progression of renal disease and cardiovascular diseases [8,9,10].
A genome-wide association study (GWAS) is a useful approach to identify causative genes and gene polymorphisms of target diseases. Some single nucleotide polymorphisms (SNPs) associated with hypertension were clarified by GWAS [11]. Investigations of SNPs targeted for the effectiveness of antihypertensive drugs, including diuretics, calcium channel blockers (CCB), and angiotensin II receptor blockers (ARB), have improved the ability to predict antihypertensive responses [12, 13]. Regarding hyperuricemia, genetic determinants related to serum UA levels have also been identified [14,15,16]. However, there are limited studies investigating the genetic backgrounds associated with hyperuricemia induced by thiazide diuretics.
The purpose of the present study was to investigate factors, including genetic the background, associated with elevated UA after treatment with a thiazide diuretic in patients with essential hypertension.
Methods
The subjects were 126 hypertensive patients (57 women and 69 men, mean age 59 ± 12 years) who registered for the GEANE (Gene Evaluation for ANtihypertensive Effects of drugs) study. The GEANE study was a multicenter clinical trial registry in Japan (UMIN-CRT-C000000119) that utilized an open random crossover protocol to examine the antihypertensive effects of valsartan (angiotensin II receptor antagonist; ARB), indapamide (thiazide-like diuretic; DIU), and amlodipine (Ca channel blocker, CCB) (Fig. 1). After one month of the nontreatment period, indapamide (1 → 2 mg/day), valsartan (40 → 80 mg/day), and amlodipine (2.5 → 5 mg/day) were administered to all patients for 3 months each in a randomized crossover manner. In the GEANE study, the order of drug prescription for each patient was decided by an automatic randomization system in the administrative office. BP, renal function, UA, and electrolytes were measured at baseline and at the end of each treatment period. Office BP was measured twice with a mercury sphygmomanometer by a doctor while the patients were quietly seated at the end of each period, and the averaged values were used for analysis. Home BP was measured in the sitting position by the patients once in the early morning and evening (before retiring). The average values of home BP during the last 3 days at the end of each period were used for statistical analysis. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) formula (for men, 194 × serum creatinine levels−1.094 × age−0.287; for women, 194 × serum creatinine levels−1.094 × age−0.287 × 0.739 [17]). SNPs associated with UA level after treatment with indapamide were investigated. Samples in the GEANE study were genotyped by the Affymetrix Genome-Wide Human Array 5.0 at the Research Institute of the National Cerebral and Cardiovascular Research Center. In this study, we investigated the association between elevation of UA after treatment with a thiazide-like diuretic and SNPs genotyped in the GEANE study. The GEANE study was approved by the Ethical Review Committee of the National Cardiovascular Center and other collaborated institutes. Written informed consent was obtained from each study participant.
Statistical analysis
Values are presented as the mean ± standard deviation (SD). Differences in variables were compared by either a paired t-test or analysis of variance. A chi-square test was also utilized when appropriate. P values <0.05 were considered significant. All calculations for clinical data analysis were performed using a standard statistical package (JMP 10; SAS Institute, Cary, NC, USA).
For genetic analysis, the data were examined using the PLINK 1.07 software (the Center for Human Genetic Research, Massachusetts General Hospital, and the Broad Institute of Harvard & MIT) in the following two evaluation models: (i) the case-control (responder–nonresponder) SNP association study by the cut-off definition as follows: patients with UA > 1 mg/dl after indapamide administration are defined as the drug-induced UA elevation. (ii) Linear regression for postmedication UA with SNPs and premedication UA as covariates. Finally, 290,698 SNPs were genotyped by the 500 K DNA microarray. The statistically significant level, p < 1.72 × 10−7 (0.05/290,698 SNPs), is significant by Bonferroni’s correction. We considered a p value of <10−5 as a statistically acceptable level based on the previous genome-wide association study (GWAS) by the Wellcome Trust Case Control Consortium (WTCCC), in which the same DNA microarray was used in the present study [11].
Results
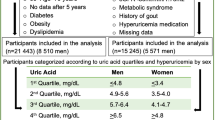
The clinical characteristics and biochemical parameters of the subjects in the control periods are shown in Table 1. The mean age was 58 ± 12 years, and 55% of the patients were male. Table 2 shows the change in the clinical characteristics and biochemical parameters after treatment with indapamide. The office, morning home, and evening home BPs decreased from 156 ± 14/93 ± 9 to 134 ± 14/84 ± 10 mmHg, from 145 ± 11/89 ± 11 to 131 ± 12/82 ± 10 mmHg, and from 140 ± 12/86 ± 10 to 130 ± 13/80 ± 11 mmHg after treatment with indapamide (p < 0.01, respectively). Indapamide was effective both in lowering office and home BPs. Treatment with indapamide significantly reduced eGFR and serum potassium and increased serum total cholesterol and UA levels (Table 2).
Patients whose UA level increased more than 1 mg/dl (n = 73) tended to be male and showed significantly higher baseline office systolic BP and plasma glucose compared with those who showed less UA increase (<1 mg/dl, n = 53) (Table 3). In addition, patients whose UA level increased more than 1 mg/dl showed a greater decline in renal function (Fig. 2).
Figure 3 shows the result of the Manhattan plots from the GWAS, indicating that SNPs associated with UA level increased more than 1 mg/dl after treatment with indapamide. The SNP shown in red is particularly strongly relevant, and rs17067290 is located on chromosome 4. Genotypes with the T allele showed a higher prevalence of UA elevation >1.0 mg/dl by odds ratio 8.4 than other genotypes, although there was no significant association with p value 5.94 × 10−6 (>1.72 × 10−7). In addition, two SNPs, rs2429085 and rs2072883, are located on chromosomes 5 and 22, respectively, and UA levels after treatment with indapamide were markedly different among three genotypes in rs2429085, A/A (from 5.88 ± 1.25 to 8.24 ± 2.28 mg/dl), A/G (from 5.52 ± 1.46 to 6.74 ± 1.88 mg/dl) and G/G (from 5.64 ± 1.52 to 6.60 ± 1.78 mg/dl), in rs2072883 of cytoskeleton-related genes, tubulin tyrosine ligase-like family, member 1 (TTLL1), C/C (from 5.20 ± 1.10 to 9.15 ± 1.93 mg/dl), C/T (from 5.33 ± 1.34 to 6.56 ± 1.94 mg/dl) and T/T (from 5.70 ± 1.50 to 6.80 ± 1.86 mg/dl) (Fig. 4). As shown in Fig. 4, rs2072883 showed a significant difference in UA elevation after taking indapamide among genotypes in the recessive model adjusted by pre-UA level with a p value of 1.32 × 10−7 (<1.72 × 10−7). Furthermore, there was a significant association of this SNP with UA elevation after indapamide administration adjusted by sex and eGFR with a p value of 8.49 × 10-8.
Manhattan plots in associated SNPs with serum uric acid levels among genotypes after the addition of indapamide in the recessive model. rs2429085 (Ch 5: red circle) had a possible association with an increase in UA after the addition of indapamide with nonsignificant p value of 5.28 × 10−5. The rs2072883 (Ch 22: red circle) had a significant association with an increase in UA after the addition of indapamide with the lowest p value of 1.32 × 10−7, which is less than the p value <1.72 × 10−7 by Bonferroni correction
Discussion
In the GEANE study, a standard dose of indapamide was effective in lowering BPs; however, adverse effects on potassium, UA, glucose and lipid metabolism, and renal function were demonstrated. In addition, some SNPs associated with an increase in UA after treatment with indapamide were identified by a GWAS investigating ~500 K SNPs.
Indapamide has been reported to reduce stroke and major cardiovascular events, to decrease left ventricular mass and to reduce microalbuminuria [18,19,20]. There is no difference in the antihypertensive effects between high-dose and low-dose diuretics; however, metabolic adverse effects often occur in a dose-dependent manner [3, 21,22,23]. Thus, JSH 2014 recommended low-dose usage of thiazide-like diuretics [3]. In addition, even the low dose of diuretics has been reported to increase UA levels [23, 24]. An increased UA level has been associated not only with gout attack but also with the development and progression of renal disease and the risk of cardiovascular diseases [6,7,8, 25]. However, an increase in UA less than 1 mg/dl was associated with a hazard ratio of 0.58 for coronary events compared with those with UA increase more than 1 mg/dl [26].
Although the exact mechanism of diuretic-induced hyperuricemia remains unknown, hydrochlorothiazide (HCTZ) may increase UA levels through diverse mechanisms, including impairment of UA secretion secondary to volume depletion, inhibition of UA efflux by multidrug resistance protein 4 and increasing UA reuptake through direct effects on organic anion transporters [24, 27, 28].
Some genetic predictors of metabolic adverse effects, such as triglyceride or total cholesterol elevations, were analyzed in hypertensive patients treated with diuretics [28]. Similarly, several novel gene regions (LUC7L2, COX18/ANKRD17, FTO, PADI4, and PARD3B) in African Americans and one region (GRIN3A) in Caucasians [29] were associated with HCTZ-induced UA elevations in the PEAR study; however, to our knowledge, there is no pharmacogenomic study on diuretic-induced UA elevations in East Asian or Japanese hypertensives. In the present study, three SNPs associated with an increase in UA after treatment with indapamide were suggested. First, rs17067290, out of a specific gene, was associated with a frequency of UA elevation >1 mg/dl after indapamide treatment, as shown in Fig. 3. Regarding the other two SNPs, rs2429085 was located in the sparc/osteonectin, cwcv and kazal-like domains proteoglycan 1 (SPOCK1) gene, and rs2072883 indicated a significant difference in the recessive model. This SNP is located in the tubulin tyrosine ligase-like family member 1 (TTLL1) gene, as shown in Fig. 4. Regarding SPOCK1, proteoglycans, which consist of a core protein and covalently linked glycosaminoglycans, are components of the extracellular matrix. SPOCK encodes a member of a novel Ca2+-binding proteoglycan family. Polyglutamylases, such as TTLL1, catalyze polyglutamylation, a reversible posttranslational protein modification that results in the addition of polyglutamate chains to the C termini of tubulins and other proteins. Polyglutamylases also add glutamate side chains to glutamate residues within the primary protein sequence. We could not clearly explain the role of these two gene variations in SPOCK1 and TTLL1 in UA elevation after indapamide treatment. Functional investigation should be necessary.
The study limitations are as follows: because this study was a crossover design using three antihypertensive drugs, recruitment of subjects was not easy even in a multicenter study. This was the main reason for the relatively small sample size and the lack of a replication study in this study. As described in the statistical analysis, the p value was very low at <1.72 × 10−7 (0.05/290698 SNPs) after Bonferroni correction. Only rs2072883 met this significant p value level even after adjustment by confounding factors. Other presented SNPs are potential susceptible signals.
Taken together, the present study results indicate that diuretic treatment, such as indapamide, may increase serum UA levels in patients with higher office BP and metabolic abnormalities, especially in patients with specific genetic polymorphisms presented in this study. We should use diuretics for hypertensive patients with attention to the risk of hyperuricemia and gout.
In conclusion, office and home BP levels decreased after treatment with indapamide. The increase in UA due to indapamide was prominent in patients with high BP or plasma glucose and was associated with the decline in renal function. A possibility that some SNPs associate with an increase in UA after treatment with a thiazide-like diuretic was suggested.
References
Miura K, Nagai M, Ohkubo T. Epidemiology of hypertension in Japan: where are we now? Circ J. 2013;77:2226–31.
Ministry of Health, Labour and Welfare: National Health and Nutrition Survey Japan 2013, Ministry of Health, Health, Labour and Welfare, 2013 (in Japanese).
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. Hypertens Res. 2014;37:253–390.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Mancia G1, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Psaty BM, Smith NL, Siscovick DS, Koepsell TD, Weiss NS, Heckbert SR, et al. Health outcomes associated with antihypertensive therapies used as first-line agents. A systematic review and meta-analysis. JAMA. 1997;277:739–45.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–64.
Feig DI, Johnson RJ. Hyperuricemia in childhood primary hypertension. Hypertension. 2003;42:247–52.
Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999;131:7–13.
OhtaY TsuchihashiT, Kiyohara K, Oniki H. Increased uric acid promotes the decline of renal function in hypertensive patients-a 10-years observational study. Intern Med. 2013;52:1467–72.
Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3000 shared controls. Nature. 2007;447:661–78.
Kamide K, Asayama K, Katsuya T, Ohkubo T, Hirose T, Inoue R, et al. HOMED-BP study group: Genome-wide response to antihypertensive medication using home blood pressure measurements: a pilot study nested within the HOMED-BP study. Pharmacogenomics. 2013;14:1709–21. GEANE study group
Turner ST, Bailey KR, Fridley BL, Chapman AB, Schwartz GL, Chai HS, et al. Genomic association analysis suggests chromosome 12 locus influencing antihypertensive response to thiazide diuretic. Hypertension. 2008;52:359–65.
Turner ST, Schwartz GL, Chapman AB, Boerwinkle E. WNK1 kinase polymorphism and blood pressure response to a thiazide diuretic. Hypertension. 2005;46:758–65.
Masuo K, Katsuya T, Fu Y, Rakugi H, Ogihara T, Tuck ML. Lys418Asn polymorphism of the alpha2-adrenoceptor gene relates to serum uric acid levels but not to insulin sensitivity. Hypertension. 2005;46:144–50.
Stark K, Reinhard W, Neureuther K, Wiedmann S, Sedlacek K, Baessler A, et al. Association of common polymorphisms in GLUT9 gene with gout but not with coronary artery disease in a large case-control study. PLoS ONE. 2008;3:1–9.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Collaborators developing the Japanese equation for estimated GFR: Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–41.
Gosse P, Sheridan DJ, Zannad F, Dubourg O, Guéret P, Karpov Y, et al. Regression of left ventricular hypertrophy in hypertensive patients treated with indapamide SR 1.5 mg versus enalapril 20 mg: the LIVE study. J Hypertens. 2000;18:1465–75.
Marre M, Puig JG, Kokot F, Fernandez M, Jermendy G, Opie L, et al. Equivalence of indapamide SR and enalapril on microalbuminuria reduction in hypertensive patients with type 2 diabetes: the NESTOR Study. J Hypertens. 2004;22:1613–22.
Pickkers P, Hughes AD, Russel FG, Thien T, Smits P. Thiazide-induced vasodilation in humans is mediated by potassium channel activation. Hypertension. 1998;32:1071–6.
Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. Br Med J. 2003;326:1427–31.
Carlsen JE, Køber L, Torp-Pedersen C, Johansen P. Relation between dose of bendrofluazide, antihypertensive effect, and adverse biochemical effects. Br Med J. 1990;300:975–8.
Ueda S, Morimoto T, Ando S, Takishita S, Kawano Y, Shimamoto K, et al. DIME Investigators: A randomised controlled trial for the evaluation of risk for type 2 diabetes in hypertensive patients receiving thiazide diuretics: Diuretics In the Management of Essential hypertension (DIME) study. BMJ Open 2014;4:e004576 https://doi.org/10.1136/bmjopen-2013-004576.
Savage PJ, Pressel SL, Curb JD, Schron EB, Applegate WB, Black HR, et al. Influence of long-term, low-dose, diuretic-based, antihypertensive therapy on glucose, lipid, uric acid, and potassium levels in older men and women with isolated systolic hypertension: The Systolic Hypertension in the Elderly Program. SHEP Cooperative Research Group. Arch Intern Med. 1998;158:741–51.
Verdecchia P, Schillaci G, Reboldi G, Santeusanio F, Porcellati C, Brunetti P. Relation between serum uric acid and risk of cardiovascular disease in essential hypertension. The PIUMA study. Hypertension. 2000;36:1072–8.
Franse LV, Pahor M, Di Bari M, Shorr RI, Wan JY, Somes GW, et al. Serum uric acid, diuretic treatment and risk of cardiovascular events in the Systolic Hypertension in the Elderly Program (SHEP). J Hypertens. 2000;18:1149–54.
Jutabha P, Anzai N, Kitamura K, Taniguchi A, Kaneko S, Yan K, et al. Human sodium phosphate transporter 4 (hNPT4/SLC17A3) as a common renal secretory pathway for drugs and urate. J Biol Chem. 2010;285:35123–32.
Vandell AG, McDonough CW, Gong Y, Langaee TY, Lucas AM, Chapman AB, et al. Hydrochlorothiazide-induced hyperuricaemia in the pharmacogenomic evaluation of antihypertensive responses study. J Intern Med. 2014;276:486–97.
Acknowledgements
The GEANE study was supported by grants-in-aid from the Ministry of Health, Labor and Health. There is no conflict of interest for all authors in the GEANE study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ohta, Y., Kamide, K., Hanada, H. et al. Genetic factors associated with elevation of uric acid after treatment with thiazide-like diuretic in patients with essential hypertension. Hypertens Res 43, 220–226 (2020). https://doi.org/10.1038/s41440-019-0356-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-019-0356-x