Abstract
Isolated systolic hypertension (ISH), defined as systolic blood pressure (SBP) ≥140 mmHg and diastolic BP (DBP) <90 mmHg, is a common type of hypertension among young men. This study aimed to investigate the clinical characteristics, central blood pressure, and arterial stiffness of young and middle-aged Japanese individuals with ISH. A total of 432 male participants, aged 18–49 years, were classified into six subgroups: optimal BP (SBP <120 mmHg and DBP <80 mmHg), high-normal BP (SBP 120–129 mmHg and DBP <80 mmHg), high-BP (SBP 130–139 mmHg and/or DBP 80–89 mmHg), ISH (SBP ≥140 mmHg and DBP <90 mmHg), isolated diastolic hypertension (IDH) (SBP <140 mmHg and DBP ≥90 mmHg), and systolic and diastolic hypertension (SDH) (SBP ≥140 mmHg and DBP ≥90 mmHg). Participants with ISH had a greater body mass index (BMI) and waist circumference than the optimal BP participants but were more likely to be physically active than the IDH and SDH participants. The central SBP of the ISH subgroup was higher than that of the optimal/high-normal/high-BP subgroups and lower than that of the SDH subgroup. The carotid–femoral pulse wave velocity (cfPWV) of the ISH subgroup was higher than that of the optimal and high-normal BP subgroups and lower than that of the SDH subgroup after adjusting for age, heart rate, BMI, and physical activity. These differences disappeared after further adjustment for central mean arterial pressure. In conclusion, the central SBP of Japanese men with ISH was greater than that of Japanese men with optimal/high-normal/high-BP, but the progression of arterial stiffness was unclear.
Similar content being viewed by others
Introduction
Isolated systolic hypertension (ISH), defined as systolic blood pressure (SBP) ≥140 mmHg and diastolic blood pressure (DBP) <90 mmHg, is a predominant form of hypertension in older people [1]. Large artery stiffening is the most important determinant of ISH in older people [2]. In fact, ISH in older people was shown to be associated with cardiovascular diseases and mortality [3]. However, ISH is also a common type of hypertension among the young population, particularly in men [1, 4, 5]. ISH in the young population seems to be a heterogeneous condition and has different pathological mechanisms than ISH in older people. For example, some studies have reported that ISH in the young population was observed in tall men who are active in sports and are nonsmokers [6, 7]. In contrast, the National Health and Nutrition Examination Survey study showed that obesity, male sex, smoking, and low educational attainment were associated with ISH among 5685 people aged 18–39 years [8]. The clinical significance of ISH in the young population also remains unclear, but central blood pressure may be useful to assess the risk of ISH in the young population. Some studies have reported that the brachial SBP of ISH in the young population might be disproportionately elevated relative to normal central SBP through physiological mechanisms so that ISH in the young population can be described as pseudo or spurious ISH [6, 7]. In this context, the high brachial SBP of ISH in the young population is considered a harmless condition. In fact, the usefulness of measuring central blood pressure of the young population with ISH has been described in the European Society of Cardiology (ESC)/European Society of Hypertension (ESH) Guidelines for the management of arterial hypertension [9]. However, two studies showed that the central SBP of young individuals with ISH was higher than that of young individuals with normal brachial BP defined as <130/85 mmHg [10] or <140/90 mmHg [11]. Furthermore, increased arterial stiffness has been documented in the contexts of ISH in the young population, indicating that ISH in the young population can be considered a harmful condition associated with increased cardiovascular risk [10].
The inconsistent findings may be attributable to differences in study population characteristics, including age, race, and comorbidities. Most of the previous studies in this field were conducted in European countries and the US. Therefore, we aimed to investigate the clinical characteristics, central blood pressure, and arterial stiffness in young and middle-aged patients with ISH in Japan.
Methods
Participants
The study candidates were 18- to 49-year-old industrial and nonindustrial workers from two companies and students from two universities in Chiba Prefecture in Japan. They participated in an annual health check-up via their organization and were asked to participate in this study on their physical check-up day between January 2017 and March 2019. Furthermore, people with ISH, isolated diastolic hypertension (IDH), and systolic and diastolic hypertension (SDH), defined later, were asked to participate again after the check-up day. We included participants not receiving anti-hypertension drugs and who did not have a previous diagnosis of secondary hypertension. Participants were classified into six subgroups based on their blood pressure levels according to the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019): (1) optimal BP (SBP <120 mmHg and DBP <80 mmHg), (2) high-normal BP (SBP 120–129 mmHg and DBP <80 mmHg), (3) high-BP (SBP 130–139 mmHg and/or DBP 80–89 mmHg), (4) ISH (SBP ≥140 mmHg and DBP <90 mmHg), (5) IDH (SBP <140 mmHg and DBP ≥90 mmHg), and (6) SDH (SBP ≥140 mmHg and DBP ≥90 mmHg). Furthermore, for the sensitivity analysis, participants were classified into five subgroups based on their blood pressure levels according to the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) hypertension guidelines: (1) normal BP (SBP <120 mmHg and DBP <80 mmHg), (2) elevated BP (SBP 120–129 mmHg and DBP <80 mmHg), (3) ISH (SBP ≥130 mmHg and DBP <80 mmHg), (4) IDH (SBP <130 mmHg and DBP ≥80 mmHg), and (5) SDH (SBP ≥130 mmHg and DBP ≥80 mmHg) [12]. Height, weight, and laboratory findings (HbA1c, total cholesterol, high-density lipoprotein cholesterol, uric acid, and creatinine) measured for the health check-up were used. Body mass index (BMI) was calculated as weight (kg) divided by the square of the height (m). Alcohol consumption (drinking or not), smoking status (smoking or not), and physical activity (performing exercise three times or more per week) were assessed using a questionnaire. A total of 432 participants underwent measurements of waist circumference (WC), hip circumference (HC), central blood pressure, and carotid–femoral pulse wave velocity (cfPWV) after providing informed consent. WC was measured at the midpoint between the bottom of the rib cage and the top of the iliac crest in the standing position at the end of expiration. HC was measured in centimeters at the widest portion of the buttocks with the tape horizontal. Measurements were performed while the patients were standing. The waist hip ratio (WHR) was calculated by dividing the WC by the HC. The institutional ethics committee approved the study protocol. Written informed consent was obtained from each participant.
Measurement of hemodynamic indices
A SphygmoCor XCEL (AtCor Medical, Sydney, Australia), which is a validated cuff-based oscillometric device, was used to measure brachial SBP, brachial DBP, central aortic SBP, central aortic DBP, central aortic mean arterial pressure (MAP), heart rate, and cfPWV [13,14,15]. Central aortic MAP was measured automatically by this device. Blood pressure amplification was defined as brachial SBP minus central aortic SBP. Pulse pressure (PP) amplification was defined as brachial PP/central aortic PP. Blood pressure measurements were performed at rest for ≥5 min in the seated position in an automated manner. CfPWV was measured as an index of arterial stiffness at rest for ≥5 min in the supine position by a single experienced examiner. The intraclass correlation coefficient of intraobserver reproducibility was 0.93. Two repeated measurements were obtained and averaged to determine BP indices and cfPWV.
Statistical analysis
All data were analyzed using STATA 15.1 software (College Station, TX, USA). All continuous values are expressed as the mean ± standard deviation (SD), and categorical variables are reported as percentages. Normally distributed continuous variables were assessed by the t-test, and nonnormally distributed continuous variables were assessed by the Mann–Whitney U test. Pearson’s Chi-square test was used to analyze all categorical variables. CfPWV was adjusted for age, heart rate, BMI, and physical activity in the analysis of covariance. Further adjustments for central aortic MAP were performed. The results are shown as adjusted values and 95% confidence intervals. All p values are two-tailed. Multiple comparisons were performed between the ISH group and the other five or four subgroups. Thus, using the Bonferroni procedure, p values <0.01 or 0.125 were considered statistically significant.
Results
The baseline demographic characteristics and laboratory findings of the six BP subgroups are presented in Table 1. The participants with ISH were younger than those with high-BP, IDH, and SDH. There was no significant difference in height or WHR, but the ISH participants had greater BMI and WC than participants with optimal BP. The SDH participants were more likely to smoke than the ISH participants (p = 0.03). The participants with IDH and SDH were less likely than the ISH participants to be physically active. The laboratory findings did not show any significant differences among the six subgroups.
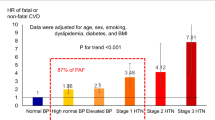
Table 2 shows the means of blood pressure, heart rate, and cfPWV of the six subgroups. The brachial SBP of the ISH participants was significantly lower than that of the SDH participants and greater than that of participants of the other four subgroups. The ISH participants had the largest blood pressure amplification, defined as brachial SBP minus aortic SBP, among the six subgroups, but the aortic SBP of the ISH participants was higher than those of the optimal, high-normal, and high-BP participants. The aortic SBP of the ISH participants was lower than that of the SDH participants. The unadjusted values of cfPWV of the ISH participants were significantly lower than those of the IDH and SDH participants and higher than those of the participants with normal BP. After adjustment for age, heart rate, BMI, and physical activity, the cfPWV values of the ISH participants were significantly lower than those of the SDH participants and higher than those of the participants with normal BP and high-normal BP (Fig. 1a). However, after further adjustment for central aortic MAP, the cfPWV values were comparable among the six groups (Fig. 1b). A sensitivity analysis of the five subgroups classified according to ACC/AHA hypertension guidelines also showed similar findings (Supplementary Table 1, Supplementary Fig. 1).
Adjusted pulse wave velocity of the six subgroups defined by the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). a Pulse wave velocity values adjusted for age, heart rate, body mass index, and physical activity. b Pulse wave velocity values adjusted for age, heart rate, body mass index, physical activity, and central aortic mean arterial pressure. BP blood pressure, ISH isolated systolic hypertension, IDH isolated diastolic hypertension, SDH systolic and diastolic hypertension
Discussion
To the best of our knowledge, this is the first study investigating the characteristics, central blood pressure, and cfPWV of young and middle-aged Japanese individuals with ISH. The participants with ISH had higher BMI and WC than the optimal BP participants, which is in line with previous findings. The central aortic SBP of the ISH subgroup was higher than that of the optimal, high-normal BP, and high-BP subgroups but lower than that of the SDH participants. The unadjusted cfPWV of the ISH subgroup was higher than that of the optimal BP subgroup and lower than that of the IDH and SDH subgroups. However, inconsistent with a previous study, there was no difference in cfPWV among all subgroups after adjustment for age, heart rate, BMI, physical activity, and aortic MAP.
High BMI and metabolic abnormalities have often been observed in young individuals with ISH [8, 16, 17]. Previous studies have suggested that insulin resistance and high salt intake contribute to the pathogenesis of ISH in children and young adults by enhancing sympathetic activity and renin-angiotensin system activity [1, 18, 19]. Although the insulin levels and salt intake data were not available, the ISH participants in this study also had higher BMI and WC. Metabolic disturbances of young individuals with ISH in Japan may contribute to a gradual increase in arterial stiffness and brachial and central aortic SBP. However, the participants with ISH had healthy behaviors, including not smoking and exercising, as opposed to the participants with SDH who were more likely to smoke and be physically inactive. This finding is consistent with the characteristics of ISH in the young population found in a previous observational study—being active in sports and nonsmokers [7]. These inconsistent characteristics, high BMI and WC but physically active nonsmokers, suggest that ISH in young Japanese men is also a heterogeneous condition.
The levels of central SBP in ISH remain controversial. BP amplification of some young individuals with ISH may be abnormally high, which leads to the concept of spurious ISH arising from disproportionately elevated brachial BP and normal central BP [6, 7]. However, the central SBP of young individuals with ISH was actually higher than that of young individuals with normal brachial BP, defined as <130/85 mmHg [10] or <140/90 mmHg [11], in several studies, including the ones describing spurious ISH [6, 7]. The findings of the present study also suggested that the high brachial SBP of the participants with ISH was amplified from an already elevated central SBP, which supports the ‘true hypertension’ view of ISH in the young population [1, 20, 21]. However, as reiterated in this article, ISH in the young population seems to be a heterogeneous condition, and some ISH individuals have been shown to have central SBP as low as that of individuals with normal BP [11]. It may be helpful to classify ISH in the young population according to the individual’s central SBP level.
High stroke volume and increased arterial stiffness were reported to contribute to high SBP and low DBP resulting in ISH characterized by high PP [10]. The Enigma Study and the Anglo-Cardiff Collaborative Trial demonstrated that young individuals with ISH had a higher stroke volume than those with normal BP [10, 20]. Elevation of stroke volume in young individuals is considered an early phase of hypertension and gradually transforms to sustained hypertension characterized by elevated peripheral vascular resistance [21, 22]. Thus, measurement of stroke volume could be helpful to clarify the mechanism and clinical significance of ISH in young Japanese people, but unfortunately, it was not performed in this study. On the other hand, we measured cfPWV as an index of arterial stiffness. However, our findings indicate that arterial stiffness is not a major determinant of the BP pattern in ISH (i.e., high SBP and low DBP resulting in high PP) because the unadjusted values of cfPWV of the ISH participants were lower than those of the SDH participants who showed high SBP and low DBP, resulting in lower PP. This is consistent with the findings that the contribution of arterial stiffness to PP is small in the young population and increases after the fifth decade [22, 23].
In this study, the differences in cfPWV between the ISH group and the optimal BP/SDH subgroups remained significant even after adjustment for age, heart rate, BMI, and physical activity. However, the differences disappeared after further adjustment for central aortic MAP. PWV is essentially dependent on the vessel distending pressure (MAP). Thus, PWV, as a surrogate index of arterial stiffness, depends on or is confounded by blood pressure levels. However, high blood pressure also results in the stiffening of arteries because of the pressure load on the wall of the arteries [23]. Thus, we could not differentiate the effects of blood pressure on the arterial stiffness of the BP subgroups in this study. However, McEniery et al. reported that after adjusting for MAP and sex, the cfPWV of the ISH group was higher than that of the normotensive participants defined as SBP <130 mmHg and DBP <85 mmHg [10]. They did not include age as a confounder because they used age-matched controls. The differences in race and age distribution between their study population (university population in the UK aged 17–27 years) and ours (university population and employees in Japan aged 18–49 years) may be the reason for this inconsistency. Long-term observational studies are required to accurately determine the cardiovascular disease risk associated with ISH in young Japanese individuals.
Our study has potential limitations. First, the small sample size and inclusion process of this study limited the generalizability of our findings. Although we asked people with ISH, IDH, and SDH to participate in this study during the check-ups and after the check-up day, the number of ISH participants was small because of the low prevalence of ISH. Second, we did not include women because of the low prevalence of ISH. Thus, it remains unclear whether the findings of this study are applicable to Japanese women. Third, stroke volume, which was a major determinant of central PP, was not measured in this study. Finally, BP measurements were obtained on a single occasion, although the Japanese hypertension guidelines recommend measuring BP at least twice to make a diagnosis.
In conclusion, our findings suggest that ISH in young and middle-aged Japanese men is a heterogeneous condition. The BMI and WC of the ISH participants were greater than those of the optimal BP participants and were comparable to those of the IDH and SDH groups. However, the ISH participants were more likely to be physically active than the IDH and SDH participants. Furthermore, the central aortic SBP of the ISH participants was lower than that of the SDH participants. The unadjusted values of cfPWV of the ISH participants were also lower than those of the IDH and SDH participants, but the differences disappeared after adjustment for covariates including aortic mean MAP. Although the progression of arterial stiffness was not clear, considering the heterogeneity of the characteristics of the young individuals with ISH, risk stratification among them may be helpful to predict future cardiovascular events. Central blood pressure may be one of the indices to assess the risk of ISH, but further studies are needed to elucidate its usefulness.
References
Palatini P, Rosei EA, Avolio A, Bilo G, Casiglia E, Ghiadoni L, et al. Isolated systolic hypertension in the young: a position paper endorsed by the European Society of Hypertension. J Hypertens. 2018;36:1222–36.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
Izzo JL Jr., Levy D, Black HR. Clinical advisory statement. Importance of systolic blood pressure in older Americans. Hypertension. 2000;35:1021–4.
Mallion JM, Hamici L, Chatellier G, Lang T, Plouin PF, De Gaudemaris R. Isolated systolic hypertension: data on a cohort of young subjects from a French working population (IHPAF). J Hum Hypertens. 2003;17:93–100.
Saladini F, Fania C, Mos L, Mazzer A, Casiglia E, Palatini P. Office pulse pressure is a predictor of favorable outcome in young- to middle-aged subjects with stage 1 hypertension. Hypertension. 2017. https://doi.org/10.1161/HYPERTENSIONAHA.117.09516.
O’Rourke MF, Vlachopoulos C, Graham RM. Spurious systolic hypertension in youth. Vasc Med. 2000;5:141–5.
Mahmud A, Feely J. Spurious systolic hypertension of youth: fit young men with elastic arteries. Am J Hypertens. 2003;16:229–32.
Grebla RC, Rodriguez CJ, Borrell LN, Pickering TG. Prevalence and determinants of isolated systolic hypertension among young adults: the 1999-2004 US National Health And Nutrition Examination Survey. J Hypertens. 2010;28:15–23.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
McEniery CM, Yasmin, Wallace S, Maki-Petaja K, McDonnell B, Sharman JE, et al. Increased stroke volume and aortic stiffness contribute to isolated systolic hypertension in young adults. Hypertension. 2005;46:221–6.
Saladini F, Santonastaso M, Mos L, Benetti E, Zanatta N, Maraglino G, et al. Isolated systolic hypertension of young-to-middle-age individuals implies a relatively low risk of developing hypertension needing treatment when central blood pressure is low. J Hypertens. 2011;29:1311–9.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–e248.
Shoji T, Nakagomi A, Okada S, Ohno Y, Kobayashi Y. Invasive validation of a novel brachial cuff-based oscillometric device (SphygmoCor XCEL) for measuring central blood pressure. J Hypertens. 2017;35:69–75.
Nakagomi A, Shoji T, Okada S, Ohno Y, Kobayashi Y. Validity of the augmentation index and pulse pressure amplification as determined by the SphygmoCor XCEL device: a comparison with invasive measurements. Hypertens Res. 2018;41:27–32.
Butlin M, Qasem A, Battista F, Bozec E, McEniery CM, et al. Carotid-femoral pulse wave velocity assessment using novel cuff-based techniques: comparison with tonometric measurement. J Hypertens. 2013;31:2237–43. discussion 2243
Julius S, Jamerson K, Mejia A, Krause L, Schork N, Jones K. The association of borderline hypertension with target organ changes and higher coronary risk. Tecumseh blood pressure study. JAMA. 1990;264:354–8.
Strazzullo P, Barba G, Cappuccio FP, Siani A, Trevisan M, Farinaro E, et al. Altered renal sodium handling in men with abdominal adiposity: a link to hypertension. J Hypertens. 2001;19:2157–64.
Campanozzi A, Avallone S, Barbato A, Iacone R, Russo O, De Filippo G, et al. High sodium and low potassium intake among Italian children: relationship with age, body mass and blood pressure. PLoS ONE. 2015;10:e0121183.
Rocchini AP, Key J, Bondie D, Chico R, Moorehead C, Katch V, et al. The effect of weight loss on the sensitivity of blood pressure to sodium in obese adolescents. N. Engl J Med. 1989;321:580–5.
McEniery CM, Franklin SS, Wilkinson IB, Cockcroft JR. Isolated systolic hypertension in the young: a need for clarity. J Hypertens. 2013;31:1911–3.
McEniery CM, Franklin SS, Cockcroft JR, Wilkinson IB. Isolated systolic hypertension in young people is not spurious and should be treated: pro side of the argument. Hypertension. 2016;68:269–75.
Lund-Johansen P. Twenty-year follow-up of hemodynamics in essential hypertension during rest and exercise. Hypertension. 1991;18:Iii54–61.
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for Improving and standardizing vascular research on arterial stiffness: a scientific statement from the American Heart Association. Hypertension. 2015;66:698–722.
Acknowledgements
This study was supported by JSPS KAKENHI (grant number JP17K15986) and a research grant from MSD (Tokyo, Japan). We are grateful to Kumiko Hiruta for her assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
YK received lecture fees from Amgen Astellas BioPharma, Sanofi, Daiichi Sankyo, Bristol-Myers Squibb, and Boehringer Ingelheim. YK received research grants from Medtronic, Daiichi Sankyo, Abbott Vascular Japan, Boston Scientific, Terumo, Win International, Otsuka Pharmaceutical, Pfizer, Boehringer Ingelheim, Astellas Pharma, Takeda Pharmaceutical, and Japan Lifeline.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nakagomi, A., Imazeki, F., Nishimura, M. et al. Central blood pressure and pulse wave velocity in young and middle-aged Japanese adults with isolated systolic hypertension. Hypertens Res 43, 207–212 (2020). https://doi.org/10.1038/s41440-019-0364-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-019-0364-x