Abstract
Some studies reported that excessive blood pressure (BP) control was not appropriate for older people, especially from the viewpoint of quality of life and maintaining sufficient blood flow for tissue perfusion. However, the lower limit of the target BP is still unclear, and there has not yet been a sufficient consensus. Therefore, we investigated the associations of BP levels with clinical events in older patients ~85 years old receiving home medical care. A total of 144 patients were included, who were followed for longer than 3 months in the Osaka Home Care Registry study, a prospective cohort study targeting older patients receiving home medical care in Japan. BP levels were divided into lower and higher groups based on the average systolic blood pressure (SBP). The main outcomes were clinical events, including hospitalizations, falls, and deaths during follow-up. As a result, the hospitalization rate in the SBP below 124 mmHg group was significantly higher than that in the SBP over 124 mmHg group. When comparing the clinical events between the two groups only in participants with hypertension, the same results were obtained. Furthermore, in Cox proportional hazards regression models adjusted by age, sex, and current diseases, the SBP below 124 mmHg group showed a significantly higher rate of required hospitalization (hazard ratio: 7.25, 95% confidence interval: 1.79–29.45). Thus, in older and very frail patients requiring home medical care, an SBP level below 124 mmHg could be a predictive marker of clinical events leading to hospitalization.
Similar content being viewed by others
Introduction
Japan has been facing emerging issues of a “super-aging” society. Accordingly, the number of elderly people who have multiple chronic diseases has increased [1]. In particular, older patients who are frail and need a high level of care have difficulties attending hospitals as outpatients. Therefore, there is increasing need for home-based medical care for patients in the intermediate stage after the completion of acute-stage treatments, those with a frail status with physical or cognitive disability, or those with an end-of-life care status.
Hypertension is very common in older patients, affecting more than ~80%. In Japan, approximately half of hypertension patients will be aged 75 years or older by 2055 [2]. Therefore, establishing appropriate blood pressure (BP) management strategies is needed in a super-aged society not only for preventing cardiovascular events but also for maintaining a high quality of life (QOL) and activities of daily living (ADL) because a well-controlled BP has been suggested to increase healthy life expectancy in various studies, such as the Framingham study [3,4,5]. Many observational data on the predictive relationship between systolic blood pressure (SBP) and mortality in very old patients are less consistent. Numerous studies recommended strict BP control in hypertensive patients [6,7,8,9,10]. In the Systolic Blood Pressure Intervention Trial (SPRINT), in people aged ≥ 75 years, the management of SBP with a target of <120 mmHg was associated with a 34% reduction in cardiovascular events and a 33% reduction in all-cause mortality, although 48.3% of strict BP control patients in SPRINT showed serious adverse events [11]. Thus, the most recent US hypertension guideline recommendation for older people with hypertension is SBP < 130 mmHg [12]. Despite the benefits of strict BP control based on SPRINT, many studies have suggested a correlation between low BP and high rates of CV events or mortality in older populations [13,14,15,16,17,18,19]. Some studies reported that excessive BP control was not appropriate for older people, especially from the viewpoint of QOL and maintaining sufficient blood flow for tissue perfusion. Furthermore, there is much uncertainty regarding the target BP in very old individuals, and there are concerns that the excessive lowering of BP in this age group may result in falls [20, 21] or cognitive problems [22, 23], including depressive symptoms [24], which may themselves result in additional morbidity and mortality. In the Japanese Society of Hypertension Guidelines 2014, the treatment target BP should be indicated for patients aged 75 years or older with a BP greater than or equal to 150/90 mmHg in principle. For frail older patients, both the treatment indication and target BP must be individually assessed [25]. However, the lower limit of the target BP is still unclear, and there has not yet been a sufficient consensus. In addition, no previous study has examined the lower limit of the target BP in older people receiving home medical care.
Based on this background, we investigated the associations of BP levels with clinical events (death, hospitalization, and falls) in older patients ~85 years old receiving home medical care.
Participants and methods
Study population
The Osaka Home Care Registry (OHCARE) study is an ongoing prospective cohort study of older patients receiving home medical care in the Osaka and Hyogo Prefectures, typical industrial areas in Western Japan. The aim of the OHCARE study was to investigate factors associated with prognosis and functional decline in older patients receiving home medical care and to establish evidence-based home medical care [26]. The OHCARE study was started in January 2015, and we collected and analyzed information from medical records and visiting nurse records every 6 months. In this study, the baseline survey took place between January 2015 and November 2016. Follow-up evaluations were conducted until July 2017. Eight home medical care clinics that provide home-visiting medical care for patients who have difficulties visiting outpatient clinics because of physical or cognitive disabilities and require medical services in their home or nursing home cooperate with the OHCARE study.
The study population included 144 Japanese patients aged 65 years or older who were followed for longer than 3 months by a home medical care doctor.
Clinical information about hypertension and BP level
The definition of hypertension was fulfilled when a baseline diagnosis of hypertension could be obtained from the medical records or the patients used antihypertensive drugs (angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers (ARBs), diuretics, calcium-channel blockers, renin inhibitors, mineral corticoid receptor r blockers, ARB diuretic combination drugs, ARB calcium-channel blocker combination drugs, α-blockers, or β-blockers).
We used the average BP of five consecutive doctor visits as the baseline BP value. BP was measured at each visit by a home medical doctor or experienced nurse in a routine manner. To evaluate the influence of the BP level on the occurrence of clinical events, we classified patients with controlled SBP into two groups: SBP lower than 124 mmHg and SBP 124 mmHg or higher, based on the average baseline SBP (123.6 mmHg).
Clinical events
All patients were followed up until July 31, 2017. The main outcome of this study was new clinical events during the follow-up period, defined as follows: hospitalization, including general or emergency admission without respite care; new falling event, including all falls during the follow-up period after the initial survey regardless of any injuries or bone fractures; and death over the 3 months after obtaining informed consent for study participation. We collected all event information from medical records and home-visiting nurse records during the follow-up period after the initial survey. Comprehensive assessments were carried out by trained nurses and public health nurses. In addition, data on the details of hospitalization were collected from the medical records obtained during the follow-up survey, and information on the clinical course and detailed medications was provided by the hospital in which the patient was admitted.
Demographic and clinical characteristics
At baseline, we collected information concerning the patients’ demographic characteristics. Disability in basic ADL and instrumental ADL was assessed with the level of care needed and the daily life independence level for dementia. The level of care needed ranged from 0 to 5 based on criteria for long-term care insurance in Japan. People certified as level 0 (assistance required) qualify for a preventive service, and those certified as levels 1 or 2 (care required) require only partial help to carry out basic ADL. People certified as levels 3–5 (care required) are completely dependent on assistance for many ADL. The daily life independence levels for dementia scores [27] are categorized into six groups. Participants assigned to group 3 or higher have “severe” dementia. We defined the presence of comorbidities as a previous history of diabetes mellitus, dyslipidemia, cardiovascular diseases, cerebrovascular diseases, respiratory diseases, bone and joint diseases, or malignant diseases based on the description in the medical records or a medical procedure. Furthermore, for diagnoses including diabetes mellitus, we also regarded participants as “affected (yes)” when they were taking at least one treatment drug or had HbA1c ≥ 6.5%. For diagnoses including dyslipidemia, we also regarded participants as “affected (yes)” when they were taking at least one treatment drug or had LDL cholesterol ≥ 140 mg/dL, TG ≥ 150 mg/dL, or HDL cholesterol ≤ 40 mg/dL.
Statistical analysis
The baseline summary characteristics are reported as the mean with standard deviation (SD) for continuous variables and as numbers with percentages for categorical variables. The distributions of categorical clinical characteristics were compared using the chi-square test or Fisher’s exact test for non-normally distributed variables, and continuous data were compared with independent t-test or the Wilcoxon signed rank test, as appropriate. Time-to-event curves were constructed with the Kaplan–Meier method and compared using the log rank test. Hazard ratios (HRs) and corresponding 95% confidence intervals (CI) were calculated with the Cox proportional hazards model after adjusting the hospitalization risks for age, sex, level of care needed, presence of heart failure, bone and joint diseases, respiratory disease, dementia, pressure sores, serum albumin, and period of receiving home medical care until the survey. All analyses were performed with SPSS version 25.0 (IBM Japan, Tokyo, Japan).
Results
Of the OHCARE study patients as of July 2017, 144 patients who were 65 years old and were followed for longer than 3 months were analyzed. The median follow-up period was 367 days (range: 300–389 days). Regarding the frequency of home-visiting medical care, twice a month was the most frequent rate (64.3%), and the remaining subjects were visited once a month (8.4%) or once a week (18.9%). Twice a week (7.0%) and every day (1.4%) were indicated for patients with serious conditions such as some infectious diseases.
Table 1 presents the clinical characteristics and sociodemographic data of the study subjects at baseline. At baseline, the mean age of the subjects was 84.1 ± 8 years, and there were 55 (38.2%) males. Eighty-one (62.8%) patients in the present study were very frail or bedridden. The mean SBP of the study subjects was 123.6 ± 18 mmHg, and the mean DBP was 67.8 ± 10 mmHg. The rate of patients with hypertension was 70.8%, and the rate of patients taking antihypertensive drugs was 89.2% among hypertensive patients.
Analysis of all participants
Based on the average SBP values collected in the baseline survey, the attributes of the two groups were examined by BP level using an average SBP of 124 mmHg as the cutoff (Table 1). There was no significant difference between the two groups in sex or age. The level of advanced dementia was significantly higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group. The rates of respiratory disease and pressure sores were also significantly higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group.
Table 2 shows the incidence of clinical events and the results of the comparison between the two groups determined by SBP levels. The rates of both hospitalization and falling events did not show any difference based on the BP level. However, when comparing the rates of hospitalization that occurred during the follow-up period, the rate in the SBP below 124 mmHg group (44.4%) was significantly higher than that in the SBP over 124 mmHg group (22.2%). Forty-eight (33.3%) of the patients experienced hospitalization at least once during the follow-up period, and there were 55 total cases when including the number of hospitalizations of patients hospitalized more than once.
Details of the reasons for hospitalization were as follows: 15 cases of pneumonia and 9 cases of unknown infection; infectious events including pneumonia and fever accounted for approximately half (43.6%) of the total hospitalizations, as shown in Table 3. In addition, the difference in incidence between the two groups of BP levels was examined for each reason for hospitalization. For hospitalizations due to pneumonia and any infection, the incidence of hospitalizations was higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group (13.9% vs. 6.9% and 9.7% vs. 2.8%, respectively). The hospitalization rate due to pneumonia or any infection was significantly higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group (p = 0.03).
Analysis of participants with hypertension
Among the subjects, 102 patients (70.8%) suffered from hypertension. In participants with hypertension, the average baseline SBP was 126.0 ± 19 mmHg vs. 117.8 ± 16 mmHg in those without hypertension (p < 0.001). There was no significant difference between the two groups in sex or age. With regard to the certified levels of care needed, the SBP lower than 124 mmHg group (level of care needed ≥ level 3: 63.8%, daily life independence for dementia ≥ level 3: 52.1%) needed more care than the SBP more than or equal to 124 mmHg group (level of care need ≥ level 3: 51.1%, daily life independence for dementia ≥ level 3: 31.9%) and tended to have a higher proportion of patients with severe disability. In addition, the prevalences of heart failure, respiratory disease, and pressure sores were significantly higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group.
Table 2 shows the incidence of clinical events and the results of the comparison by BP level in patients with hypertension. One hundred and six subjects with hypertension showed no difference in incidence between the BP level groups regarding the rates of acute hospitalization and falling events. However, in hospitalizations that occurred during the follow-up period, the rate was significantly higher in the SBP below 124 mmHg group than in the SBP over 124 mmHg group (44.4 vs. 22.2%). In addition, in the analysis of 42 patients without hypertension, no significant difference was found between the two BP level groups in the rate of events in the baseline survey and that during the follow-up period.
Factors of hospitalization in patients with hypertension
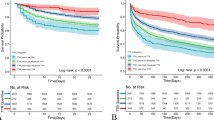
From the results of the clinical events, there was a significant difference in the incidence of hospitalization during follow-up between the two BP level groups. Based on this result, factors related to hospitalization were examined using a Cox proportional hazards model. From the findings of previous studies that examined factors related to hospitalization and death, adjustment factors including sex [28], ADL [29], bone and joint diseases [30], heart failure [31], dementia [32, 33], serum albumin [29, 34], and period of receiving home medical care until the survey [35] were selected. In addition, in this analysis, it was confirmed that there was a significant difference in the presence of hospitalization events between the two groups, so the variables of SBP below 124 mmHg, respiratory disease, and pressure sores, which showed a significant difference on comparison, were used as adjustment variables (Table 4) (Fig. 1). As a result, in patients with hypertension, SBP below 124 mmHg [HR: 7.25, 95% CI: 1.79–29.45], male sex [HR: 6.80, 95% CI: 1.42–32.47], and low serum albumin [HR: 0.29, 95% CI: 0.11–0.80] were independently associated with hospitalization caused by pneumonia or any infections.
Hospitalization avoidance curve based on multivariate Cox regression in patients with hypertension. The analysis was adjusted for age, sex, level of care needed, presence of heart failure, bone and joint diseases, respiratory disease, dementia, pressure sores, serum albumin, and period of receiving home medical care until the survey
Discussion
In Japan, the declining birth rate and aging population are becoming more serious, and the demand for home medical care is markedly increasing. Although some previous studies about BP management focused on hospital and clinical patients, no definite study has established a strategy focused on older patients receiving home medical care. Furthermore, there is no study about optimal BP management in home medical care. Therefore, we tried to clarify the optimal BP level for patients in home medical care.
In our study, we examined the associations between BP levels and clinical events in older patients receiving home-visiting medical care. As a result, although deaths and falling events were not significantly associated with BP, hospitalization events during home care were significantly more frequent in the SBP below 124 mmHg group than in the SBP over 124 mmHg group. Even after adjusting for sex, ADL, and presence of other diseases, SBP below 124 mmHg was independently related to hospitalization events. Similar results were obtained when analyzing only patients with hypertension. The difference in results between death and hospitalization events can be attributed to the finding that more than 90% of the patients receive home-visiting medical care at least twice a month, so that the medical staff could respond promptly even during sudden changes. It was suggested that even if hospitalized, fatal events leading to death could be avoided. Thus, we propose that the SBP level may be a useful biomarker to anticipate clinical events or the progression of geriatric syndrome in older patients with home medical care.
Another previous study suggested that older people in the end-of-life stage may show a declining SBP [36]. The mechanism of BP lowering in older patients is that disabilities lead to low activity and loss of appetite. Thus, these individuals cannot maintain appropriate blood flow for tissue perfusion. Although the mechanism by which the maintenance of BP above 124 mmHg prevents hospitalization in elderly individuals cannot be clarified in this study, we speculate that low BP levels below SBP 124 mmHg may accelerate becoming more frail by low blood perfusion in systematic organs in older patients. Consequently, it is easy for older patients with a BP that is too low to obtain infectious events such as pneumonia or aspiration pneumonia. It was also suggested that maintaining an SBP above 124 mmHg may prevent hospitalization due to geriatric syndrome, including pneumonia, in older patients with home medical care. Therefore, older people with a disability might benefit from maintaining an SBP over 124 mmHg to prevent hospitalization due to an infectious event such as pneumonia.
In addition, regarding the details of the hospitalization events in the present study, there were few cerebral cardiovascular events, and it is characteristic that there were many hospitalizations due to weakness of the whole body triggered by pneumonia and any infection; moreover, hospitalization factors in later-stage elderly patients examined in previous studies also showed similar results [37]. The prevention of lethal cerebral cardiovascular disease events is also important for older patients receiving home medical care, but it is more beneficial to delay the progress of generalized weakness triggered by nonfatal events such as aspiration and infectious diseases.
When investigating the association between BP and clinical events, the influence of the patient’s background, such as current diseases, should be considered. In our study, patients who were frail since the first survey and patients who were obliged to lower BP on a specific disease basis, such as those with heart failure and cerebrovascular diseases, may have been included in the SBP below 124 mmHg group. However, according to the Cox proportional hazards model, SBP below 124 mmHg was an independent factor, and it was suggested that it is an independent risk factor even after adjusting for the effects of ADL and some diseases. In a previous study that examined the relationship between BP lowering and the survival rate in older patients with hypertension aged over 80 years old, the higher the BP level was, the lower the mortality rate even after considering BMI, age, number of antihypertensive drugs, QOL summary score of physical aspects and mental aspects, and Charlson comorbidity index [34]. From this result, it became clear that the survival rate was determined by antihypertensive treatment. However, in another previous study, when the baseline patient condition (MMSE, ADL, serum albumin value, cancer, and cardiac disease) was adjusted for the differences caused by BP levels, the association between BP and mortality disappeared.
As described above, there was no consistent result regarding the association between the antihypertensive treatment of older patients and hospitalization in the previous study. In addition, since the patient background, including the mean BP, in the previous study was different from that in the present study, we cannot compare the two studies accurately. Therefore, we believe that our results should be regarded as a new finding for the home medical care field.
Furthermore, in the previous study that considered the outcomes of pneumonia, which comprised most of the outcomes of our research, and examined related factors, it was considered that COPD, smoking, stroke, and low ADL were factors related to lower respiratory tract infections [38]. In this study, even when considering the influence of respiratory disease, ADL, and other current diseases, the effect of SBP below 124 mmHg remained. Therefore, from the results of this study, an index SBP of 124 mmHg is useful as a biomarker for comprehensively expressing the general condition of older patients receiving home medical care, considering all factors such as sex, age, ADL, and current diseases, which is suggested as a novel finding.
In addition, in response to the results of SPRINT reported in recent years, the newly revised American Heart Association/American College of Cardiology stage classification sets the step-down target BP value as very low. This should be carefully considered when being introduced in Japan, where there are many super-aged patients receiving home medical care. Based on the research evidence in Japan, it is necessary to establish a treatment policy. In particular, in the present study, patients taking antihypertensive drugs and those with a low BP showed more hospitalization events caused by pneumonia or any infections. As mentioned above, it may be possible to consider reducing antihypertensive drugs to avoid excessive BP reduction.
Strengths and limitations
This was a prospective cohort study of older patients receiving home medical care provided by multiple clinics that conduct home-visiting medical care, and we can grasp the current state of home medical care more accurately. In addition, information was obtained from reliable materials such as medical records, and those with medical certificates directly collected the information, which further supports the reliability of the information.
Furthermore, the present study is a unique population-based sample of participants with a mean age of ~85 years. To our knowledge, this is the first study to examine the associations of BP levels with clinical events in older patients receiving home medical care.
In addition, our study is novel in that it targeted not only patients who were hospitalized and outpatients but also older patients receiving home medical care. Our research is important in that the results will contribute to evidence for home medical care that has not yet been developed. Furthermore, we examined the causal relationship between the BP level and events that lead to hospitalization, including disease conditions such as pneumonia and infections, which are frequently observed in older patients and were not examined in previous research.
On the other hand, our study had some limitations. First, the BP measurement method differed depending on clinics, and it was not possible to take into consideration BP fluctuation due to measurement positions. However, the present study focused on prediction in clinical practice and in clinical organizations, and it could be confirmed that more than half of the clinics conducted auscultator measurements using an Aneroid sphygmomanometer, and the measurement posture of patients was almost the same through the baseline and follow-up surveys. The second limitation is the selection bias in the research participants. The studied subjects did not include all patients who were receiving home-visiting care in the cooperating organizations but were limited to only patients who provided consent or patients whose families provided consent. There is a possibility that patients unlikely to provide consent, such as dementia patients living alone, were not included.
Third, information on the dosage and number of tablets of antihypertensive drugs was insufficient. In this study, we obtained information on only the kind of medicine. However, in future surveys, collection items related to dosage and the number of tablets will be added, and it will be necessary to conduct a more accurate study by continuing the follow-up survey.
Conclusion
In home medical care, excessive BP reduction, such as SBP below 124 mmHg, may be related to the occurrence of events leading hospitalizations, and a low SBP level below 124 mmHg may be a marker predicting a general condition leading to hospitalization. Therefore, it was suggested that careful BP management is necessary in older patients requiring long-term care.
References
Ministry of Health, Labor and Welfare. Vital statistics 2017. Tokyo: Ministry of Health, Labor and Welfare; 2017.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Amery A, Brixko P, Clement D, De Schaepdryver A, Fagard R, Forte J, et al. Mortality and morbidity results from the European working party on high blood pressure in the elderly trial. Lancet. 1985;325:1349–54.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the systolic hypertension in the elderly program (SHEP). JAMA. 1991;265:3255–64.
Franco OH, Peeters A, Bonneux L, De Laet C. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–6.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Murakami Y, Hozawa A, Okamura T, Ueshima H. Relation of blood pressure and all-cause mortality in 180000 japanese participants pooled analysis of 13 cohort studies. Hypertension. 2008;51:1483–91.
Fukuhara M, Arima H, Ninomiya T, Hata J, Yonemoto K, Doi Y, et al. Impact of lower range of prehypertension on cardiovascular events in a general population: the Hisayama study. J Hypertens. 2012;30:893–900.
Okayama A, Kadowaki T, Okamura T, Hayakawa T, Ueshima H. Age-specific effects of systolic and diastolic blood pressures on mortality due to cardiovascular diseases among Japanese men (NIPPON DATA80). J Hypertens. 2006;24:459–62.
Angeli F, Reboldi G, Verdecchia P. Hypertension and the J-curve phenomenon: implications for tight blood pressure control. Hypertens Res. 2013;36:109–11.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs. standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years a randomized clinical trial. JAMA. 2016;315:2673–82.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary. Hypertension. 2018;71:1269–324.
Mattila K, Haavisto M, Rajala S, Heikinheimo R. Blood pressure and five year survival in the very old. Br Med J. 1988;296:887–9.
Poortvliet RKE, De Ruijter W, De Craen AJM, Mooijaart SP, Westendorp RGJ, Assendelft WJJ, et al. Blood pressure trends and mortality: the Leiden 85-plus Study. J Hypertens. 2013;31:63–70.
Satish S, Freeman DH, Ray L, Goodwin JS. The relationship between blood pressure and mortality in the oldest old. J Am Geriatr Soc. 2001;49:367–74.
Molander L, Lövheim H, Norman T, Nordström P, Gustafson Y. Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc. 2008;56:1853–9.
Rastas S, Pirttilä T, Viramo P, Verkkoniemi A, Halonen P, Juva K, et al. Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc. 2006;54:912–8.
Van Bemmel T, Gussekloo J, Westendorp RGJ, Blauw GJ. In a population-based prospective study, no association between high blood pressure and mortality after age 85 years. J Hypertens. 2006;24:287–92.
Benetos A, Labat C, Rossignol P, Fay R, Rolland Y, Valbusa F, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern Med. 2015;175:989–95.
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172:1739–44.
Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK. Greater daily defined dose of antihypertensive medication increases the risk of falls in older people—a population-based study. J Am Geriatr Soc. 2014;62:1527–33.
Mossello E, Pieraccioli M, Nesti N, Bulgaresi M, Lorenzi C, Caleri V, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175:578–85.
Peng J, Lu F, Wang Z, Zhong M, Sun L, Hu N, et al. Excessive lowering of blood pressure is not beneficial for progression of brain white matter hyperintensive and cognitive impairment in elderly hypertensive patients: 4-year follow-up study. J Am Med Dir Assoc. 2014;15:904–10.
Boal AH, Smith DJ, McCallum L, Muir S, Touyz RM, Dominiczak AF, et al. Monotherapy with major antihypertensive drug classes and risk of hospital admissions for mood disorders. Hypertension. 2016;68:1132–8.
Putignano E, Calcara L, Monteverde A, Curatolo G, Marchese M, Barbagallo Sangiorgi G. Arterial hypertension in the elderly. Cardiologia. 1994;39:585–9.
Yamamoto M, Kabayama M, Koujiya E, Huang Y, Akiyama M, Higami Y, et al. Factors associated with changes of care needs level in disabled older adults receiving home medical care: prospective observational study by Osaka Home Care Registry (OHCARE). Geriatr Gerontol Int. 2019;19:1198–205.
Ministry of Health, Labor and Welfare. Collection of laws and regulations related to certification for long-term care. Ministry of Health, Labor and Welfare; 2004.
Kuzuya M, Hasegawa J, Enoki H, Izawa S, Hirakawa Y, Hirose T, et al. Gender difference characteristics in the sociodemographic background of care recipients. Nippon Ronen Igakkai Zasshi. 2010;47:461–7. (in Japanese).
Ishizaki T, Kai I. Risk of acute hospitalization among long-term home care patients. Nippon Ronen Igakkai Zasshi. 2000;37:472–8. (in Japanese).
Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997;87:398–403.
Wilson RS, Rajan KB, Barnes LL, Hebert LE, Mendes De Leon CF, Evans DA. Cognitive aging and rate of hospitalization in an urban population of older people. J Gerontol A Biol Sci Med Sci. 2014;69:447–54.
Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association between incident dementia and risk of hospitalization. J Am Med Assoc. 2012;307:165–72.
Motzek T, Werblow A, Tesch F, Marquardt G, Schmitt J. Determinants of hospitalization and length of stay among people with dementia—an analysis of statutory health insurance claims data. Arch Gerontol Geriatr. 2018;76:227–33.
Oates DJ, Berlowitz DR, Glickman ME, Silliman RA, Borzecki AM. Blood pressure and survival in the oldest old. J Am Geriatr Soc. 2007;55:383–8.
Umegaki H, Asai A, Kanda S, Maeda K, Shimojima T, Nomura H, et al. Risk factors for the discontinuation of home medical care among low-functioning older patients. J Nutr Heal Aging. 2016;20:453–7.
Ravindrarajah R, Hazra NC, Hamada S, Charlton J, Jackson SHD, Dregan A, et al. Systolic blood pressure trajectory, frailty and all-cause mortality over 80 years of age. cohort study using electronic health records. Circulation. 2017;135:2357–68.
Morita M. Factors related to the long-term prognosis of home-based medical care subjects. Nippon Ronen Igakkai Zasshi. 2015;52:383–90. (in Japanese).
Sliedrecht A, den Elzen WP, Verheij TJ, Westendorp RG, Gussekloo J. Incidence and predictive factors of lower respiratory tract infections among the very elderly in the general population. The Leiden 85-plus Study. Thorax. 2008;63:817–22.
Acknowledgements
This study was supported by JSPS KAKENHI, Grant Numbers JP19K07888, JP19K11138, and JP17K12506. We sincerely thank all OHCARE study participants for their kind cooperation. We gratefully thank all staff at the cooperating clinics and former OHCARE research group members, Ms. Madoka Fukusaki, Ms. Kazuko Sakanoue, Ms. Takako Inoue, Ms. Ya Huang, and Ms. Yumiko Aoshima, as well as Ms. Tae Matsue for secretarial work.
Funding sources
This study was supported in part by grants-in-aid from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (KK: 2510211, 15K08910; MK: 16K12336; MA: 976771).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethics committee of the Osaka University Graduate School of Medicine (Approval Number: 2014-310).
Informed consent
Written informed consent was obtained from all participants or from a close relative.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koujiya, E., Kabayama, M., Yamamoto, M. et al. Associations of blood pressure levels with clinical events in older patients receiving home medical care. Hypertens Res 44, 197–205 (2021). https://doi.org/10.1038/s41440-020-00538-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-00538-5