Abstract
MicroRNAs are key molecules involved in the regulation of endothelial function. They are important risk factors and biomarkers for the development of hypertension related to endothelial dysfunction. However, the gene expression patterns associated with hypertension development related to endothelial dysfunction have not been fully elucidated. We conducted a case-control study of 65 patients with essential hypertension (EH) and 61 controls without EH. Plasma levels of miR-122 and its target protein high-affinity cationic amino acid transporter 1 (CAT-1) were measured by qRT-PCR and ELISA, respectively. miR-122 expression in plasma of patients with EH was significantly higher than that of the control group (p = 0.001), while CAT-1 expression in patients with EH was significantly lower than that in the control group (p = 0.018). miR-122 expression in plasma of young patients with EH was significantly higher than that in young people without EH (p = 0.0004), and CAT-1 expression in plasma of young patients with EH was also significantly lower than that of the control group (p = 0.002). CAT-1 expression in the plasma of young participants was significantly higher than that of individuals aged ≥40 years (p = 0.003), whereas miR-122 expression was significantly lower (p = 0.001). We showed that among patients with EH, the high expression of miR-122 contributed to endothelial dysfunction by suppressing the expression of the CAT-1 protein, which led to a decrease in CAT-1 expression in plasma. Therefore, high expression of miR-122 appears to be a risk factor for endothelial dysfunction in EH, especially in younger patients.
Similar content being viewed by others
Introduction
Essential hypertension (EH) is an important global health challenge due to its high incidence and potential complications. The early diagnosis, treatment, and effective control of hypertension are crucial in preventing cardiovascular, cerebrovascular, and other diseases. However, the molecular mechanisms responsible for the occurrence and development of EH are unclear.
In recent years, the prevalence rate of EH has increased, likely due to improved living conditions as well as an increased pace of life and mental stress. In particular, the prevalence of EH in younger people has increased, although the rates of diagnosis, treatment, and control of EH are lower for younger people than for the older population [1, 2]. EH is a multifactorial disease and there is an urgent need to identify EH at an early stage to prevent the resulting complications.
MicroRNAs (miRNAs) are endogenous, noncoding, single-stranded RNAs of ~22 nucleotides in length. miRNAs repress RNA transcription in a sequence-specific manner and regulate targeted protein-coding gene expression at the posttranscriptional level. A single miRNA can target multiple genes, and a single gene can be targeted by multiple miRNAs. miRNAs represent a complex regulatory network that controls the basic physiological and pathological processes of several cardiovascular diseases, including hypertension [3]. Circulating miRNAs are emerging biomarkers of EH, can provide new insights into its pathological mechanism, and serve as targets for the design of novel therapeutic drugs [3]. Studies have shown that miR-122—a mammalian, liver-specific miRNA—originates from its precursor mRNA, named the “hcr gene,” and can downregulate the expression of high-affinity cationic amino acid transporter-1 (CAT-1) by targeting its 3′ untranslated region (UTR) [4, 5]. Endothelial production of nitric oxide (NO) is dependent on the transport of its substrate l-arginine via CAT-1. miR-122 can, therefore, regulate arginine transport and consequently affect NO synthesis by affecting the expression of the CAT-1 protein [6, 7]. One study has shown that impaired endothelium-dependent NO-mediated vasodilation is a key feature of EH and may precede the increase in blood pressure (BP) [8, 9].
The relative expression of miR-122 and CAT-1 in the plasma of patients with EH has not been reported. In our case-control study, we investigated the relationship between plasma-circulating levels of miR-122, CAT-1, and EH. We also determined whether the plasma-circulating level of miR-122 was associated with an increased risk of EH and whether it could be a molecular biomarker for screening and early diagnosis of EH.
Materials and methods
Study design
A total of 126 subjects were selected from inpatients, outpatients, and volunteers at the Fuwai Hospital PUMC and CAMS (Beijing, China) from May to December 2017. This cohort comprised 65 patients with EH (46 males and 19 females) and 61 without EH (53 males and 8 females). The EH and non-EH groups were divided into “young” subgroups (18–39 years) and “old” subgroups (≥40 years), for a total of four subgroups (young EH, young non-EH, old EH, and old non-EH).
Sample collection
Samples of whole blood were collected at Fuwai Hospital, PUMC, and CAMS (Beijing, China). Blood samples were prepared by isolating plasma, stored at −80 °C, and subsequently analyzed for the expression of miR-122 and CAT-1.
The diagnosis of EH was based on three BP measurements over 140/90 mmHg without the use of antihypertensive drugs. These criteria are in accordance with the recommendations by the guidelines set by the Chinese government for the prevention and treatment of hypertension. Patients with new-onset and well-controlled EH were included in the study. Of the patients with EH, ten were newly diagnosed, 49 had been treated recently, and the remaining six had not been assessed adequately. The duration of disease in patients with EH was 3–360 months.
None of the study participants had secondary hypertension, severe diseases of the liver, kidney or blood system, cardiovascular disease, systemic infection, connective tissue disease, malignant tumors, thyroid disease, severe depression, dementia, chronic inflammatory diseases, mental illness, or a history of drug addiction. In addition, none of the participants was pregnant or lactating.
Blood was drawn from a superficial brachial vein into an anticoagulant vacuum tube containing sodium citrate (Vacutainer; BD Biosciences, San Jose, CA, USA) via a 21-G needle taking care to avoid stasis, hemolysis, or contamination by tissue fluids or exposure to glass.
Plasma isolation
Plasma was separated from whole blood and centrifuged at 1000 × g for 15 min at 4 °C to remove dead cells. Pellets were discarded, and the supernatant was transferred to a new collection tube and centrifuged at 10000 × g for 15 min at 4 °C. Finally, the supernatant was discarded, and the pellets were resuspended in 1 mL of phosphate-buffered saline and centrifuged at 10000 × g for 15 min at 4 °C. Then, the pellets were stored in liquid nitrogen for further analyses.
RNA extraction and quantitative reverse transcription-polymerase chain reaction (RT-PCR) to measure miR-122 expression in plasma
RNA was extracted from plasma using a TRIzol kit (Invitrogen, Carlsbad, CA, USA). The purity and concentration of the extracted RNA was determined by ultraviolet analysis (Nanodrop 2000; Thermo Scientific, Rockford, IL, USA). miR-122–5p (accession number: MIMAT0000421) primers were used for reverse transcription (PrimeScript RT Reagent kit with gDNA Eraser; TaKaRa Biotechnology, Shiga, Japan). miR-122 expression in plasma was analyzed by real-time PCR (SYBR Premix ExTaq; TaKaRa Biotechnology). The primer used for reverse transcription for hsa-miR-122–5p was CAGTGCAGGGTCCGAGGTCAGAGCCACCTGGGCAATTTTTTTTTTTCAAACA. The PCR forward primer for hsa-miR-122–5p was AACACGCTGGAGTGTGACAAT, and the reverse primer was CAGTGCAGGGTCCGAGGT. Semiquantitative RT-PCR consisted of an initial denaturation at 95 °C for 15 s, 45 cycles at 95 °C for 5 s, and 60 °C for 30 s. Real-time PCR was performed using a previously tested primer set and SYBR Master Mixture according to the manufacturer’s instructions (TaKaRa Biotechnology) for the TP800 Real-Time PCR instrument (TaKaRa Biotechnology).
CAT-1 biochemical assay
CAT-1 was detected by an enzyme-linked immunosorbent assay (ELISA) kit (Human Cationic Amino Acid Transporter 1 ELISA) according to the manufacturer’s instructions (Biofine, China).
Statistical analyses
Continuous variables are presented as the mean ± SD or as the median within the interquartile range. The normality of the data was evaluated using the Shapiro–Wilk test and confirmed using Q–Q plots of the data against a normal distribution. Appropriate transformations (e.g., log, square-root, 1/x, exp, squaring, cubing, or Box-Cox transformations) were performed for the variable if a significant departure from normality was observed. Differences between mean values that had a normal distribution were compared using two-way ANOVA (stratified by age groups), whereas nonparametric tests (Kruskal–Wallis rank sum test) were used if the assumption of normality or homogeneity of variance were not met after data transformation. Post hoc analyses were undertaken using Tukey’s honest significant difference test or pairwise Mann–Whitney U-tests with the Bonferroni correction to adjust p values, as appropriate. Categorical variables are expressed as frequencies and percentages, whereas testing for differences was performed by the chi-square test or Fisher’s exact test. Spearman correlation analysis was undertaken to ascertain the correlation between CAT-1 expression, miR-122 expression, systolic blood pressure (SBP), and diastolic blood pressure (DBP). The area under the receiver operating characteristic curve (AUC), sensitivity, and specificity were used to assess the performance of CAT-1 and miR-122 as indicators for diagnosing hypertension. The optimal cutoff value for the predicted probabilities of hypertension and for distinguishing hypertension cases from non-hypertension cases was chosen using the maximal Youden’s Index. The 95% confidence interval of the AUC, sensitivity, and specificity was calculated using bootstrap methods with 1000 replicates for each number. P < 0.05 was considered significant. All analyses were performed in R v2.15.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics of the study cohort
Data were collected from 61 non-EH group participants and 65 patients with EH. There were no significant differences regarding age (45 ± 14.16 vs. 45 ± 12.11 years, p = 0.774). The SBP (p < 0.001), DBP (p < 0.001), and pulse pressure (p < 0.001) of the EH group were significantly higher than those of the non-EH group. The relative expression of miR-122 (p = 0.001) and CAT-1 (p = 0.018) in plasma varied significantly between the EH and non-EH groups. The clinical characteristics of the study subjects are summarized in Table 1.
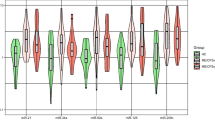
We also performed a subgroup analysis of the relative expression of miR-122 and CAT-1 in the plasma of all cohorts (Table 2 and Fig. 1). CAT-1 expression in younger subjects was significantly higher than that in older subjects (p = 0.003). miR-122 expression in younger subjects was significantly lower than that in older subjects (p = 0.001; Table 3).
Expression of miR-122 and CAT-1 in plasma and correlation with BP
There was no significant correlation between plasma levels of miR-122 or CAT-1 and BP in the entire 126-subject cohort and the old subgroup. However, there was a close correlation between plasma CAT-1 levels and SBP (r = 0.388, p < 0.05) as well as DBP (r = 0.384, p < 0.05) among young participants. Further analyses revealed a close relationship between the relative expression of miR-122 and CAT-1 in plasma for the entire cohort (r = 0.266, p < 0.05). No significant correlation was found between the indicators mentioned above in old participants (r = 0.103, p > 0.05), although there was a close correlation in young participants (r = 0.322, p = 0.016).
Diagnostic accuracy of miR-122 and CAT-1
We also assessed the prognostic value of the expression of miR-122 and CAT-1 as effective markers of EH, both individually and in combination. The AUC for the expression of miR-122, CAT-1, and the combination of miR-122 and CAT-1 for all participants was 0.68, 0.62, and 0.69, respectively. The AUC for the expression of miR-122, CAT-1, and miR-122 plus CAT-1 in old participants was 0.61, 0.55, and 0.63, respectively. In young participants, the AUC for miR-122 expression, CAT-1 expression, and miR-122 plus CAT-1 expression was 0.79, 0.75, and 0.85, respectively (Fig. 2, Table 4).
Discussion
miRNAs are short, noncoding, single-stranded RNA molecules that typically have a regulatory effect on gene expression by inhibiting mRNA translation. Studies have suggested that miRNAs are the key regulators of various pathophysiological processes, including the proliferation, differentiation, apoptosis, survival, and activation of cells, and morphogenesis. miRNAs also play an important role in the pathogenesis and development of hypertension and affect the renin–angiotensin–aldosterone system, vascular endothelial dysfunction, and vascular smooth muscle [10]. Maintaining homeostatic expression of miRNAs that have key regulatory functions in specific cells represents a potential new avenue for hypertension treatment [11].
Studies have shown that miR-122 can regulate arginine transport and, consequently, have an impact on NO synthesis by affecting the CAT-1 protein [6, 7, 12]. Bhattacharyya et al. showed that the activity of CAT-1 mRNA in human Huh7 cells is controlled by miR-122 and that CAT-1 expression can be upregulated by inhibiting miR-122 expression [13]. Yang et al. reported that altered expression of the type-1 CAT-1 coding gene SLC7A1 results in physiologically relevant changes in NO production and endothelial function [6, 7]. Chang et al. found that miR-122 can act as a specific suppressor to negatively regulate the stability of CAT-1 mRNA [4]. Furthermore, Yang et al. showed that hypertensive people could have lower levels of SLC7A1 expression, resulting in endothelial dysfunction [6]. Cengiz et al. found that in patients with “white coat hypertension,” plasma expression of miR-21, miR-122, miR-637, and let-7e was upregulated significantly [13]. Recently, Zhou et al. found that miR-122 expression in the plasma of hypertensive African green monkeys was significantly higher than that of normotensive African green monkeys [14]. Several established miR-122 targets, including cyclin G1, ADAM10, IGF1R, SRF, and Wnt1, have been shown to be involved in hepatocarcinogenesis, epithelial–mesenchymal transition, angiogenesis, and vascular remodeling [15].
A link between CAT-1 expression and hypertension was demonstrated by Konstantinidis et al. They found that overexpression of endothelial CAT-1 prevents oxidative stress and increases arterial pressure in response to inhibition of superoxide dismutase in mice [16]. Schlaich et al. demonstrated that l-arginine transport is impaired in hypertension, but differences in the expression of CAT-1 mRNA and protein in peripheral blood mononuclear cells were not detected [8]. Rajapakse et al. indicated that l-arginine is also an important determinant of renal NO production, NO-dependent function, and long-term regulation of arterial BP [17]. They also suggested that impairments in l-arginine transport could lead to the development of hypertension [18].
Our findings in patients with clinical EH support the data from other studies. We found that CAT-1 expression in plasma was reduced significantly in patients with EH. This observation suggests that young patients with EH show marked dysfunction with regard to NO synthesis (specifically using arginine transported by CAT-1). These data also suggest that CAT-1 may have a crucial role in the early stage of EH, which is associated with vascular endothelial dysfunction.
Furthermore, we found that CAT-1 expression in plasma was inversely correlated with miR-122 expression in plasma, particularly in younger patients. However, there was no significant correlation between CAT-1 expression, miR-122 expression, and BP in the overall cohort or older group. Interestingly, we found a significant relationship between CAT-1 expression in plasma, SDP, and DBP in younger participants. The ROC analyses further supported the notion that miR-122 and CAT-1 can be considered biomarkers of endothelial dysfunction in young patients with EH.
Binding of miR-122 to the 3′UTR of CAT-1 has been shown to lead to decreased metabolism of l-arginine and NO in vascular endothelial cells, resulting in dysfunction of vascular endothelial cells, which is an important cause of hypertension. We confirmed the relationship between miR-122 expression, CAT-1 expression, and EH in the present study.
Our study involved a small cohort. Further research with more patients and controls is needed to evaluate the importance of the altered expression of miR-122 and CAT-1 in EH. In this way, a potential method for the clinical diagnosis of EH and therapeutics based on these results can be designed.
Conclusions
Studying the dysregulation of NO synthesis in endothelial cells is an important step in understanding endothelial dysfunction. Few scholars have focused on the expression of miR-122 and CAT-1 in EH, and studies have been limited to cellular and animal experiments.
We showed that among young patients with EH, high expression of miR-122 contributed to endothelial dysfunction by suppressing the expression of the CAT-1 protein, leading to a decrease in CAT-1 expression in plasma. Furthermore, we hypothesize that high expression of miR-122 is a critical risk factor in endothelial dysfunction in EH, especially in young patients.
References
Moon JY, Park KJ, Hwangbo Y, Lee MR, Yoo BI, Won JH, et al. A trend analysis of the prevalence, awareness, treatment, and control of hypertension by age group. J Prev Med Public Health. 2013;46:353–9.
Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017;70:736–42.
Romaine SPR, Charchar FJ, Samani NJ, Tomaszewski M. Circulating microRNAs and hypertension-from new insights into blood pressure regulation to biomarkers of cardiovascular risk. Curr Opin Pharm. 2016;27:1–7.
Chang J, Nicolas E, Marks D, Sander C, Lerro A, Buendia MA, et al. miR-122, a mammalian liver-specific miRNA, is processed from hcr mRNA and may downregulate the high affinity cationic amino acid transporter CAT-1. RNA Biol. 2005;1:106–13.
Valdmanis PN, Kim HK, Chu K, Zhang F, Xu J, Munding EM, et al. miR-122 removal in the liver activates imprinted microRNAs and enables more effective microRNA mediated gene repression. Nat Commun. 2018;9:5321.
Yang Z, Venardos K, Jones E, Morris BJ, Dusting JC, Kaye DM. Identification of a novel polymorphism in the 3′UTR of the contribution to hypertension and endothelial dysfunction. Circulation. 2007;115:1269–74.
Yang Z, Kaye DM. Mechanistic insights into the link between a polymorphism of the 3´UTR of the SLC7A1 gene and hypertension. Hum Mutat. 2009;30:328–33.
Schlaich MP, Parnell MM, Ahlers BA, Finch S, Marshall T, Zhang WZ, et al. Impaired L-arginine transport and endothelial function in hypertensive and genetically predisposed normotensive subjects. Circulation. 2004;110:3680–86.
Chin-Dusting JP, Willems L, Kaye DM. L-Arginine transporters in cardiovascular disease: a novel therapeutic target. Pharm Ther. 2007;116:428–36.
Klimczak D, Jazdzewski K, Kuch M. Regulatory mechanisms in arterial hypertension: role of microRNA in pathophysiology and therapy. Blood Press. 2017;1:2–8.
Li X, Wei Y, Wang Z. microRNA-21 and hypertension. Hypertens Res. 2018;41:649–61.
Coulouarn C, Factor VM, Andersen JB, Durkin ME, Thorgeirsson SS. Loss of miR-122 expression in liver cancer correlates with suppression of the hepatic phenotype and gain of metastatic properties. Oncogene. 2009;40:3526–36.
Cengiz M, Karatas OF, Koparir E, Yavuzer S, Ali C, Yavuzer H, et al. Differential expression of hypertension-associated microRNAs in the plasma of patients with white coat hypertension. Medicine. 2015;13:e693.
Zhou X, Wang J, Fa Y, Ye H. Signature microRNA expression profile is associated with spontaneous hypertension in African green monkey. Clin Exp Hypertens. 2019;3:287–91.
Naveed A, ur-Rahman S, Abdullah S, Naveed MA. A concise review of microRNA exploring the insights of microRNA regulations in bacterial, viral and metabolic diseases. Mol Biotechnol. 2017;59:518–29.
Konstantinidis G, Head GA, Evans RG, Nguyen-Huu TP, Venardos K, Croft KD, et al. Endothelial cationic amino acid transporter-1 overexpression can prevent oxidative stress and increases in arterial pressure in response to superoxide dismutase inhibition in mice. Acta Physiol. 2014;4:845–53.
Rajapakse NW, Mattson DL. Role of L-arginine in nitric oxide production in health and hypertension. Clin Exp Pharm Physiol. 2008;3:249–55.
Rajapaksea NW, Mattson DL. Role of cellular L-arginine uptake and nitric oxide production on renal blood flow and arterial pressure regulation. Curr Opin Nephrol Hypertens. 2013;1:45–50.
Acknowledgements
We thank Dr Jianxing Yu and Prof. Jingmei Jiang for their help with statistical assessments.
Funding
This work was supported by grants from the CAMS Initiative for Innovative Medicine (2016-I2M-3–006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Ethics Committee at the Institute of Microcirculation at the Chinese Academy of Medical Sciences (CAMS; Beijing, China) and Peking Union Medical College (PUMC; Beijing, China). The study adhered to the tenets of the Declaration of Helsinki as well as applicable Chinese laws.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, HG., Zhang, QJ., Li, BW. et al. The circulating level of miR-122 is a potential risk factor for endothelial dysfunction in young patients with essential hypertension. Hypertens Res 43, 511–517 (2020). https://doi.org/10.1038/s41440-020-0405-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-0405-5
Keywords
This article is cited by
-
miRNA-ome plasma analysis unveils changes in blood–brain barrier integrity associated with acute liver failure in rats
Fluids and Barriers of the CNS (2023)
-
Impact of Nutritional Epigenetics in Essential Hypertension: Targeting microRNAs in the Gut-Liver Axis
Current Hypertension Reports (2021)
-
Plasma microRNA levels in childhood IgA vasculitis
Clinical Rheumatology (2021)
-
Roles of MicroRNA-122 in Cardiovascular Fibrosis and Related Diseases
Cardiovascular Toxicology (2020)