Abstract
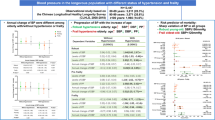
We investigated the association of systolic blood pressure (SBP) level with physical frailty and cognitive function in community-dwelling older Japanese. Using the ‘Septuagenarians, Octogenarians, Nonagenarians Investigation with Centenarians’ survey as the baseline, we performed a cross-sectional analysis of people aged 70 ± 1 (n = 1000), 80 ± 1 (n = 978), and 90 ± 1 (n = 272) years. Medical histories and medications were collected via interviews conducted by medical professionals. Blood pressure (BP), grip strength, gait speed, and cognitive function were examined on site. Trend analysis and multiple regression analysis were used to determine the association of the SBP level with physical frailty and cognitive function. The principal finding was that the association of SBP with physical frailty and cognitive function varied depending on characteristics such as age, physical and cognitive function, and antihypertensive medication use. A lower SBP level was associated with a higher prevalence of physical frailty only among 80-year-olds who were on antihypertensive medication. A significant association was found between higher SBP and lower cognitive function among 70-year-olds, while among 90-year-olds, the opposite was found. No association was found among participants who were 80 years old or among participants of all ages without antihypertensive medication. Our finding that an inverted association between SBP and geriatric syndrome exists suggests that the treatment of older patients must be individualized to prevent geriatric syndrome.
Similar content being viewed by others
Introduction
The prevalence of hypertension increases with age: 66.5% of people aged 65–74 years, 75.7% of those aged 75–84 years, and 78.1% of those aged ≥85 years have hypertension [1, 2]. Despite its high prevalence and high morbidity, the optimal level to which blood pressure (BP) should be lowered in older adults remains controversial due to inconsistent evidence concerning the association between high or low BP control and adverse outcomes [3, 4]. A recent randomized controlled trial (RCT), the SPRINT study, reported a positive association between strictly controlled BP (systolic BP < 120 mmHg) and reduced outcome events [5]. Odden et al. reported an association between strict lowering of BP and increased risk of mortality and other events [3]. Staessen et al. reported that the higher the age of the patient, the less evidence there was for the preventive effects of antihypertensive treatment on cardiovascular diseases [6].
Aside from these conflicting results, older populations have varying physical and mental functions. While some individuals are robust, others are frail, with cognitive decline or dementia, or are bedridden. In several previous studies, it was reported that the relationship between blood pressure and mortality differs depending on walking speed [3, 7]. Odden et al. reported that hypertension was associated with decreased mortality in older adults who could not complete the 6 m walk [3]. They speculated that in older adults with a low walking speed, which is characteristic of frailty, elevated BP may be necessary for maintaining the perfusion of vital organs. A review by Novak et al. reported that both hypertension and hypotension affect brain perfusion and worsen cognitive outcomes in older people [8]. However, antihypertensive treatment decisions for older people are based on evidence extrapolated from drug trials in more robust patient groups with fewer physiological deficits [9, 10]. In addition, many frail older people have multiple chronic comorbidities, such as renal impairment and postural hypotension [11]; thus, they are prescribed many medications [10] although those comorbidities may be worsened by BP-lowering medications. Therefore, for the older population, it is important to clarify the optimal BP control taking into account the subpopulation’s characteristics.
As described above, numerous studies have investigated the optimal control for high BP to prevent a cardiovascular event or mortality [12]; however, studies addressing quality-of-life outcomes, such as the prevention of geriatric syndrome, are still scarce. If the goal of treatment in older people is to achieve healthy longevity, it is very important to investigate the association of BP level with physical frailty and cognitive function, which are common and important geriatric syndrome symptoms, to determine the optimal BP.
The purpose of this study was to investigate the association of SBP level with physical frailty status and cognitive function among 70-, 80-, and 90-year-old community-dwelling Japanese individuals.
Methods
Study population
The present cross-sectional analysis was based on the baseline survey of the ongoing prospective cohort study called the ‘Septuagenarians, Octogenarians, Nonagenarians Investigation with Centenarians’ (SONIC) study [13]. The narrow age ranges (69–71, 79–81, and 89–91 years) were designed to exclude age as a confounder. Participants were randomly selected for the SONIC study using an invitation-type survey through the local residential registries from four areas in Japan. A detailed description of the study design and protocol has been published elsewhere [13,14,15].
Overall, 1000 participants (men, 479; women, 521) aged 69–71 years, 973 participants (men, 457; women, 516) aged 79–81 years, and 272 participants (men, 123; women, 149) aged 89–91 years completed the baseline survey in 2010, 2011, and 2012, respectively. We excluded participants with dementia (as determined from the medical history and medication information) from the analysis of cognitive function.
The SONIC study was approved by the Ethics Review Board of Osaka University Graduate School of Medicine, Dentistry, and Human Sciences and the Tokyo Metropolitan Institute of Gerontology (approval numbers 266, H22-E9, 22 018, and 38, respectively). Written informed consent was obtained from all participants.
Assessment of medical factors
We collected information on the patients’ medical history of chronic diseases (e.g., hypertension, diabetes, coronary heart disease, or cerebrovascular disease) and medications through interviews and medication notebook inspections that were conducted by trained medical doctors and nurses. Height, weight, and BP were measured at the survey venue. BP in the left and right arms was measured twice by either a physician or a trained nurse using a standard mercury sphygmomanometer or electronic monitor while the participant was sitting on a chair after at least a few minutes of rest. We used the averaged blood pressures of each mean in the right and left arms. Hypertension was defined as systolic BP (SBP) ≥140 mmHg or diastolic BP (DBP) ≥90 mmHg or as having received antihypertensive treatment [16]. We categorized SBP levels as follows: SBP: ≤119, 120–139, 140–159, ≥160 mmHg. Venous blood samples for the measurement of plasma glucose, plasma lipids, and other biochemical indicators were collected at site. Diabetes was defined as a fasting plasma glucose concentration of ≥7.0 mmol/L (126 mg/dL), a casual plasma glucose concentration of ≥11.1 mmol/L (200 mg/dL), HbA1c ≥6.5%, or current use of medication for diabetes [17].
Physical frailty
Physical frailty was assessed by grip strength and gait speed based on the Cardiovascular Health Study criteria (Supplementary Table 1) [18]. Grip strength was measured twice by the dominant hand using a Smedley hand dynamometer (Model YD-100; Yagami, Ltd., Tokyo, Japan) with the participants sitting with their arms held against their body. The mean of the two measurement values was calculated and used in the analyses. Gait speed was measured by the 8-feet gait speed test. The test was repeated twice, and the mean speed was used in the analyses. The physical frailty value was categorized into a binary variable. Pre-physical frailty or physical frailty was defined as 1, and nonfrailty was defined as 0.
Assessment of cognitive function
Cognitive function was assessed using the Japanese version of the Montreal Cognitive Assessment (MoCA-J) by trained geriatricians and psychologists [19]. The MoCA is a brief cognitive screening tool for detecting mild cognitive impairment in older people [19, 20]. Total MoCA scores range from 0 to 30, with higher scores reflecting higher cognitive function. We used the MoCA-J total score with adjustment for education level as an indicator of cognitive function.
Statistical analysis
Descriptive data are presented as means for consecutive variables and as percentages for categorical variables. Student’s t-test was used to compare continuous variables between the two groups, and the chi-square test was used for categorical variables. Among the three groups, one-way analysis of variance for continuous variables and multiple comparison tests for categorical variables were used with Bonferroni corrections as post hoc analysis. To examine the relationship between SBP and physical frailty, multiple logistic regression analysis was used, while multiple linear regression analysis was used for SBP and the MoCA-J score, with or without adjustment for potential confounders. Tests for trends in associations were evaluated using the following trend analyses: the Cochran-Armitage Test for categorical variables and the Jonckheere-Terpstra Test for continuous variables. P-values < 0.05 were considered significant. All statistical analyses were performed using SPSS Statistics 25.0 (IBM Japan, Tokyo, Japan).
Results
Characteristics of the study population
The characteristics of the 2235 participants are shown in Table 1. There were significant differences in all variables between the participants in the three age groups. Among participants with antihypertensive medication, SBP and DBP among those 70 years old and DBP among those 90 years old were significantly lower. MoCA-J scores among 70-year-olds taking antihypertensive medication were significantly lower than in those without antihypertensive medication. The opposite was observed in the 80- and 90-year-olds. In the comparison between participants with and without physical frailty, those with frailty showed significantly lower DBPs and serum-albumin levels; furthermore, the proportions of participants with cardiovascular diseases (CVD) and diabetes mellitus (DM) were higher (Table 2).
Associations of physical frailty with SBP
Among 80-year-old participants with antihypertensive medication, lower SBP levels were associated with a higher prevalence of physical frailty by the Cochran-Armitage trend test (p < 0.01). This result was not found in 70- and 90-year-olds (Fig. 1). This relationship remained significant after adjusting for confounders (sex, albumin, CVD, DM) by multiple logistic regression (Table 3). No such association was found among individuals without antihypertensive medication in any age group.
Associations of cognitive function with SBP
Cognitive function among participants with antihypertensive medication, based on SBP classification by age group, is shown in Fig. 2. In this analysis, we excluded participants with dementia. The number of excluded participants was one septuagenarian, 16 octogenarians, and 23 nonagenarians. A significant association was found between higher BP and lower cognitive function in the 70-year-old group. No association was found in the 80-year-old group. Moreover, among 90-year-olds, lower SBP was associated with lower cognitive function, which was opposite to the finding in 70-year-olds. No association was found among participants without antihypertensive medication. The association of higher SBP with lower cognitive function for 70 years persisted after adjustment for potential confounding factors, including stroke, DM, dyslipidemia, and current smoking (Table 4). When we analyzed the participants with and without antihypertensive medication together, we found an independent association of higher SBP at 70 years old and lower SBP at 90 years old with lower cognitive function and no association at 80 years old (data not shown). We subsequently conducted the same analysis as above, stratified by physical frailty status, based on antihypertensive medication use. We found an association of higher SBP with lower cognitive function only among non-physically frail 70-year-old individuals who were on antihypertensive medication (data not shown).
Discussion
The principal finding of the present study was that the association of SBP with physical frailty and cognitive function varied depending on characteristics such as age, physical and cognitive function, and antihypertensive medication use. A lower SBP level was associated with a higher prevalence of physical frailty only among 80-year-olds taking antihypertensive medications (Fig. 1). Among 70-year-old individuals on antihypertensive medication, a significant association was found between higher SBP and lower cognitive function, while among those 90 years old, the opposite was found. There was no association among participants aged 80 years and among participants of all ages without antihypertensive medication (Fig. 2). These findings of age-specific relationships between SBP and geriatric syndromes among a large community-dwelling older population including 90-year-old individuals are the novelty of this research.
From our results, we can infer that the association between SBP levels and frailty (including cognitive function) differs depending on age, antihypertensive medication use, and functional status. Furthermore, the association of SBP differs between physical frailty and cognitive frailty. In prior studies of participants with a mean age of 70 years, findings showed a negative effect of higher BP on physical or cognitive functions and that BP-lowering treatment reduces cardiovascular risk [12, 21, 22]. It has also been reported that antihypertensive drug treatment is associated with a lower incidence of dementia among people in their 70 s [23]. In addition to these findings among 70-year-olds, most of the results observed among the very old population or among patients with a functionally declined status revealed an association of low BP with low cognitive function, risk of stroke, and mortality, which were opposite relationships to those observed for individuals in their 70s [24,25,26,27,28,29]. Moreover, the risk of mortality was exaggerated in people with frailty compared to robust participants [29]. The present investigation agrees with those previous studies. On the other hand, recent studies, such as the SPRINT study, have reported that strict BP control (SBP <120 mmHg) reduces mild cognitive impairment. We assume that this is due to the different functional status of the participants, such that differential patterns of association emerged depending on the subgroups.
The mechanisms linking lower SBP with physical frailty prevalence or declined cognitive function among the very old population are not fully clear; however, from previous studies, there are some speculations. First, a higher BP control level may have a favorable effect on muscle strength because it ensures skeletal muscle blood flow in people in their 90 s or older as well as in functionally declined individuals, such as frail older adults [30]. With regard to cognitive function, higher BP is associated with an increased risk of white-matter lesions in people in their 60 s and 70s [4, 31]. In addition, cerebrovascular damage due to vascular risk factors directly triggers vascular dementia, and vascular risk factors also increase the risk of neurodegenerative Alzheimer’s disease [32]. In contrast, Corrada et al. reported a reduced risk of dementia in people aged ≥90 years with hypertension who reported the onset of hypertension after the age of 80 years, suggesting that adequate cerebral perfusion may help maintain normal cognition [33]. This may be due to a sufficient nutritional supply to fuel the brain’s high metabolic activity [34, 35]. Second, since frail or very older people tend to be prescribed multiple medications [10], this polypharmacy may affect their functional status both physically and cognitively, either directly or via the adverse effects of dizziness or falling [36,37,38]. Regarding the fact that no relationship was found in the 80 s age range, we speculated that there was no consistent age characteristic due to the mixture of robust and frail subjects. Such functional differences among individuals in both cognitive and physical function may have affected the results. In contrast, in subjects in their 90 s, the present results were obtained because the participants’ cognitive and physical functions, such as frailty (91.7% were frail, Table 1) or low cognitive function, were somewhat consistent. The results of participants without antihypertensive medications were interpreted as showing no association between blood pressure and cognitive function. We speculated that these individuals were originally normotensive or had white coat hypertension, which may not have had a strong influence on physical and cognitive functions. Another possibility is that the 90-year-old patients had a small sample size, so that the difference was not detected.
The present study has several limitations. First, the subjects participated voluntarily in the investigation, so we cannot exclude the possibility that they were a group of older people with high health literacy compared to that in the general population. It is also probable that the study participants were relatively healthy and showed lower rates of mild cognitive impairment or dementia than the general older population. Thus, there is the possibility that we are seeing a survival effect, especially in the 80- and 90-year-olds. In addition, selection bias may have affected the results by the potential absence of data for participants who did not participate in the study because they were not able to visit the survey site by themselves. The participation ratio was 23.2% in the 70-year-old group, 18.0% in the 80-year-old group, and 13.8% in the 90-year-old group. Therefore, future research using home-visit interviews is required. Second, we could not infer a causal relationship due to the cross-sectional study design. Although we adjusted for cardiovascular comorbidities in the multivariate analysis, it is possible that participants with a history of cardiovascular disease with strictly controlled BP may already be frail. Third, we could not determine the potential risk of polypharmacy and types of antihypertensive medications. Fourth, the results of cognitive function were not based on the cutoff value but the continuous score; thus, this difference would not emerge in a clinical setting. However, the significance of differences was noteworthy and may provide important evidence of the relationship between SBP and cognitive function. Fifth, in this research, we did not distinguish whether the subjects’ decline in cognitive function was due to cerebrovascular disease or Alzheimer’s disease. As the number of people with dementia was very small in our community-based study, it is probable that this issue would not be clear even if an MRI were performed.
In conclusion, the present study showed that the patterns of association of the SBP level with physical frailty and cognitive function differ depending on antihypertensive medication use, functional status, and age group in the older population. Our finding that an inverted association between SBP and geriatric syndrome exists suggests that in the real world, where the older population has a smaller proportion of robust individuals, the treatment of older patients must be individualized to prevent geriatric syndrome. Our results imply that among older people, those who have declined functionality or are over 90 years old may do better to avoid strict lowering of the SBP. However, in robust older people such as those who are 70 years old, it is important to control hypertension to delay or prevent cognitive impairments. Further longitudinal and interventional studies are needed to clarify the appropriate lower limit of BP in older populations.
References
McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol A. 2009;64A:256–63.
Williamson JD, Pajewski NM, Auchus AP, et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. Jama 2019;321:553–61.
Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172:1162–8.
Den Heijer T, Launer LJ, Prins ND, Van Dijk EJ, Vermeer SE, Hofman A, et al. Association between blood pressure, white matter lesions, and atrophy of the medial temporal lobe. Neurology. 2005;64:263–7.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged >/=75 years: a randomized clinical trial. JAMA. 2016;315:2673–82.
Staessen JA, Fagard R, Thijs L, Celis H, Birkenhäger WH, Bulpitt CJ, et al. Subgroup and per-protocol analysis of the randomized European Trial on isolated systolic hypertension in the elderly. Arch Intern Med. 1998;158:1681–91.
Odden MC, Covinsky KE, Neuhaus JM, Mayeda ER, Peralta CA, Haan MN. The association of blood pressure and mortality differs by self-reported walking speed in older Latinos. J Gerontol A Biol Sci Med Sci 2012;67:977–83.
Novak V, Hajjar I. The relationship between blood pressure and cognitive function. Nat Rev Cardiol 2010;7:686–98.
Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA 2007;297:1233–40.
Hubbard RE, O’Mahony MS, Woodhouse KW. Medication prescribing in frail older people. Eur J Clin Pharm. 2013;69:319–26.
Kamide K, Kabayama M. Implications of blood pressure variations in older populations. Hypertension Res: Off J Jpn Soc Hypertension. 2019;42:19–25.
Briasoulis A, Agarwal V, Tousoulis D, Stefanadis C. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studies. Heart 2014;100:317.
Gondo Y, Masui Y, Kamide K, Ikebe K, Arai Y, Ishizaki T SONIC Study: a longitudinal cohort study of the older people as part of a centenarian study. In: Pachana NA, editor. Encyclopedia of geropsychology. Singapore: Springer Science+Business Media; 2016.
Ikebe K, Gondo Y, Kamide K, Masui Y, Ishizaki T, Arai Y, et al. Occlusal force is correlated with cognitive function directly as well as indirectly via food intake in community-dwelling older Japanese: from the SONIC study. PLoS ONE. 2018;13:e0190741.
Ryuno H, Kamide K, Gondo Y, Nakama C, Oguro R, Kabayama M, et al. Differences in the association between high blood pressure and cognitive functioning among the general Japanese population aged 70 and 80 years: The SONIC study. Hypertens Res. 2016;39:557–63.
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus, Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A. 2001;56:M146–57.
Fujiwara Y, Suzuki H, Yasunaga M, Sugiyama M, Ijuin M, Sakuma N, et al. Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr Gerontol Int. 2010;10:225–32.
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Hajjar I, Lackland DT, Cupples LA, Lipsitz LA. Association between concurrent and remote blood pressure and disability in older adults. Hypertension. 2007;50:1026–32.
Launer LJ, Masaki K, Petrovitch H, Foley D, Havlik RJ. The association between midlife blood pressure levels and late-life cognitive function: the Honolulu-Asia aging study. JAMA. 1995;274:1846–51.
Forette F, Seux ML, Staessen JA, Thijs L, Birkenhäger WH, Babarskiene MR, et al. Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet. 1998;352:1347–51.
Aparicio LS, Thijs L, Boggia J, Jacobs L, Barochiner J, Odili AN, et al. Defining thresholds for home blood pressure monitoring in octogenarians. Hypertension 2015;66:865–73.
Benetos A, Labat C, Rossignol P, Fay R, Rolland Y, Valbusa F, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE Study. JAMA Intern Med 2015;175:989–95.
Peters R, Beckett N, Forette F, Tuomilehto J, Clarke R, Ritchie C, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7:683–9.
Molander L, Gustafson Y, Lovheim H. Low blood pressure is associated with cognitive impairment in very old people. Dement Geriatr Cogn Disord. 2010;29:335–41.
Mossello E, Pieraccioli M, Nesti N, Bulgaresi M, Lorenzi C, Caleri V, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175:578–85.
Sabayan B, van Vliet P, de Ruijter W, Gussekloo J, de Craen AJ, Westendorp RG. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus Study. Stroke. 2013;44:15–20.
Taekema DG, Maier AB, Westendorp RG, Craen AJ. Higher blood pressure is associated with higher handgrip strength in the oldest old. Am J Hypertens. 2011;24:83–9.
Gianaros PJ, Greer PJ, Ryan CM, Jennings JR. Higher blood pressure predicts lower regional grey matter volume: Consequences on short-term information processing. Neuroimage. 2006;31:754–65.
Takeda S, Rakugi H, Morishita R. Roles of vascular risk factors in the pathogenesis of dementia. Hypertension Res: Off J Jpn Soc Hypertension. 2020;43:162–7.
Corrada MM, Hayden KM, Paganini-Hill A, et al. Age of onset of hypertension and risk of dementia in the oldest-old: The 90+ Study. Alzheimers Dement 2017;13:103–10.
Cunnane SC, Nugent S, Roy M, Courchesne-Loyer A, Croteau E, Tremblay S, et al. Brain fuel metabolism, aging and Alzheimer’s disease. Nutrition. 2011;27:3–20.
Korf ES, Scheltens P, Barkhof F, de Leeuw FE. Blood pressure, white matter lesions and medial temporal lobe atrophy: closing the gap between vascular pathology and Alzheimer’s disease? Dement Geriatr Cogn Disord. 2005;20:331–7.
Klein D, Nagel G, Kleiner A, Ulmer H, Rehberger B, Concin H, et al. Blood pressure and falls in community-dwelling people aged 60 years and older in the VHM&PP cohort. BMC Geriatr. 2013;13:50.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–60.
Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588–95.
Acknowledgements
We are grateful to all SONIC participants who participated in these studies. We appreciate all the staff involved in the SONIC study, especially Yumiko Aoshima, Tae Matsue, and Yasuyo Takamine for their secretarial work and support.
The members of the SONIC Study Group
Toshiaki Sekiguchi10, Kentaro Tanaka10, Kazuya Taira10, Tomoko Noma10, Werayuth Srithumsuk10, Nonglak Klinpudtan10, Naoko Wada10, Atsuko Higuchi10, Serina Yokoyama11, Satomi Maeda11, Motonori Nagasawa11, Taku Fujimoto11, Shinichi Sato12, Yoshiko Ishioka13, Megumi Tabuchi14, Kennichi Matsuda15, Taiji Ogawa15, Masahiro Kitamura15, and Yoshinobu Maeda15
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
M.K. received a grant (16K12336, 19K11138), and K.K. has received a grant (15K08910, 19K07888) from JSPS KAKENHI.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Other author contributors are listed in the Acknowledgments section.
Supplementary information
Rights and permissions
About this article
Cite this article
Kabayama, M., Kamide, K., Gondo, Y. et al. The association of blood pressure with physical frailty and cognitive function in community-dwelling septuagenarians, octogenarians, and nonagenarians: the SONIC study. Hypertens Res 43, 1421–1429 (2020). https://doi.org/10.1038/s41440-020-0499-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-0499-9
Keywords
This article is cited by
-
Association between systolic blood pressure trajectories and successful aging in middle-aged and elderly Chinese individuals: a longitudinal study
BMC Public Health (2025)
-
Association between salt intake and blood pressure among community-dwelling older adults based on their physical frailty status
Hypertension Research (2025)
-
Office and home blood pressure and their difference according to frailty status among community-dwelling older adults: the NOSE study
Hypertension Research (2025)
-
Hypertension facilitates age-related diseases. ~ Is hypertension associated with a wide variety of diseases?~
Hypertension Research (2024)
-
Pulse pressure tells the story of sarcopenia
Hypertension Research (2024)