Abstract
Reservoir placement for the inflatable penile prosthesis has evolved over time with surgical safety and functional outcomes driving innovative changes. This state of the art review describes contemporary placement options for the inflatable penile prosthesis reservoir, including traditional space of Retzius placement and other alternate reservoir placements. The space of Retzius remains a familiar location for virgin placements while submuscular placement has gained popularity for its versatility and lower risk of visceral injury. The lateral retroperitoneal location can be considered for a patient with a hostile pelvis. A comparison of complications and functional outcomes highlights benefits and drawbacks of each location. This review aims to equip the prosthetic urologist with modern techniques and a surgical armamentarium that can address any reservoir placement.
Similar content being viewed by others
Introduction
The inflatable penile prosthesis (IPP) remains the gold standard surgical management for erectile dysfunction [1]. The device as known today contains three components– cylinders, pump, and reservoir. Of these, the pump and cylinders are “patient facing” and receive much attention in sizing and positioning. The reservoir remains hidden and unnoticed. Still, reservoir placement is the surgical step that gives implanters appropriate pause, due to potentially devastating complications associated with a reservoir placement gone awry.
The introduction of the IPP in 1973 by F. Brantley Scott and colleagues revolutionized management of erectile dysfunction [2]. Since that time, incremental changes have resulted in the device as known today, boasting high patient satisfaction [3,4,5,6] and device longevity [7,8,9]. With the introduction of lockout valves, a new frontier for reservoir placement was born [10]. Subsequently, manufacturers have adapted the shapes of their reservoirs to limit palpability in alternate locations (Fig. 1). These innovations decreased the risk of auto-inflation and laid the foundation for alternative reservoir placements beyond the traditional space of Retzius location.
a Coloplast Cloverleaf reservoir comes in 2 sizes (75 cc and 125 cc) approved for retropubic and ectopic placement (used with permission from Coloplast Corporation). b Boston Scientific AMS Conceal reservoir (left) compared to the AMS Spherical reservoir (right). AMS spherical is made in both 65 cc and 100 cc sizes, the AMS Conceal comes in 100 cc size only. (used with permission from Boston Scientific Corporation).
This state of the art review will describe contemporary reservoir placement sites and offer considerations for patient selection and safe placement.
Methods
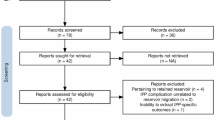
We performed a literature review on November 8, 2024 utilizing Medline/PubMED and Embase databases from 1981 to 2024 including search terms Inflatable Penile Prosthesis, Reservoir, and Complications. This resulted in 204 English language articles which were reviewed for content by the authors. Ultimately 81 articles pertaining to IPP reservoir location and complications were identified and reviewed in depth in order to summarize the contemporary literature pertaining to IPP reservoirs. A subset of these articles with observational or comparative clinical data was compiled for narrative comparison by reservoir location.
Approach considerations and risks of reservoir placement
Complications and safety
When selecting a reservoir location, two features warrant consideration: safety and functionality. The first of these, safety, has been the primary impetus for the development of alternative reservoir locations. Any prosthetic surgeon is acutely aware of the proximity of the pelvic viscera and vasculature to a trans-inguinal reservoir (Fig. 2). This was objectively demonstrated by Henry and colleagues who documented distances between the external inguinal ring and pelvic structures in 28 cadavers. The bladder lays 5–8 cm medially when empty and just 2–4 cm medial when full. The iliac vein was located 2.5–4 cm laterally [11]. After abdominal surgery, scar tissue may alter these relationships or bring bowel closer to the inguinal ring as well.
The true incidence of pelvic visceral injury after reservoir placement is difficult to ascertain, in part because most IPPs are placed by low volume implanters (<5 implants/year) and are not likely accurately represented in the current body of academic literature [12]. One contemporary series of 872 cases reported a rate of 0.5–1.9% depending on the approach utilized [13]. A separate series of 536 patients reported 2–5% reservoir related complications depending on approach [14].
Meanwhile, case series have reported intraoperative injury to the bladder [15,16,17,18], bowel [19], and pelvic vasculature [19, 20]. Bladder injuries, if recognized, have been managed successfully with closure of the cystotomy and repositioning of a fresh reservoir to the contralateral side [16, 17] (Fig. 3). Vascular complications may include venous compression resulting in lower extremity swelling, venous thromboembolic complications [20,21,22,23,24], or gross hemorrhage necessitating emergent vascular repair, typically requiring a larger counter incision and vascular surgery consultation.
Functionality and innovation
While these intraoperative complications are of paramount concern to surgeons, equally important from a patient perspective is the postoperative, functional outcome. One of the earliest examples of alternate reservoir location was a response to a functional problem. German surgeons in the 1990s regularly placed reservoirs intraperitoneally to avoid capsule formation associated with autoinflation [25].
Autoinflation refers to the unintentional transfer of fluid from the reservoir to the cylinders which results in unwanted cylinder inflation. This is typically due to the formation of a restrictive capsule around the reservoir, reservoir placement in a high pressure location, or stress induced by patient activity. With a historical prevalence as high as 11% [10], the introduction of lockout valves lowered contemporary rates to 1.3–3% [10, 26].
The lockout valve was first introduced in 2000, within the reservoir of the Mentor Alpha 1 device. (Mentor Corporation, Santa Barbara, CA, USA) [10]. Mentor was later purchased by Coloplast Corporation (Humlebaek, Denmark) which currently maintains a lockout valve within their cloverleaf reservoir. American Medical Systems (AMS, Minnetonka, MN, USA), now Boston Scientific (Marlborough, MA, USA), introduced a lockout valve in the pump of their device in 2006 [26]. The development of lockout valves permitted higher ambient pressure on the system and ushered in the latest evolution of IPP surgery- alternate reservoir placement (ARP).
The appeal of ARP, typically submuscular and separated from the pelvic viscera by the transversalis fascia, lay in the avoidance of injury to pelvic structures. Theoretically, this movement away from the pelvic viscera and towards the abdominal wall could increase the functional risks of reservoir palpability, herniation, or revision. To better accommodate ARP, device companies responded with low profile reservoirs: conceal (2010, Boston Scientific) and cloverleaf (2011, Coloplast). In 2015, the FDA granted Coloplast changes to labeling to indicate ectopic (alternate) reservoir placement [27]. A number of ARP techniques have now been described and are employed with increasing frequency by prosthetic urologists. The remainder of this review will describe contemporary IPP reservoir placement options and compare the safety and functionality outcomes reported with each (Table 1).
Contemporary reservoir placement options
Orthotopic / space of retzius
Traditionally, prosthesis reservoirs were placed in the retropubic Space of Retzius (SOR), which presumably avoided the risk of injury to intraperitoneal structures and provided a low pressure environment that reduced risk of auto-inflation. This was first described in 1973 with entrance into the retropubic space via the external ring and inguinal canal or via direct suprapubic cut down [26]. Numerous modified techniques to enter this space have been described, including finger dissection and blunt penetration of the transversalis fascia, or more sharply using scissors or a nasal speculum [28].
As previously discussed, the proximity of pelvic viscera and vasculature to the SOR constitutes the primary risk of reservoir placement. This risk is increased by contemporary pelvic surgeries such as prostatectomy, cystectomy, and renal transplant which may alter or obliterate the SOR [29]. A retrospective review of SOR reservoir placements in 115 patients with prior prostatectomy reported no visceral or vascular complications and concluded that SOR placement after prostatectomy remained safe, though potentially more challenging due to scar tissue [30]. Meanwhile, cystectomy opens the pelvis to abdominal contents, resulting in higher reservoir placement risk. A handful of studies have examined reservoir placement following cystectomy with all avoiding the SOR and opting for submuscular [31] or lateral retroperitoneal locations [32].
SOR remains a familiar, functional, and popular location for reservoir placement. In the author’s practice this location remains an appropriate option for IPP placement without prior pelvic surgery, hernia repairs, or altered anatomy. In such cases, we prefer ARP. For very thin patients, the SOR location is preferred due to a lower risk of palpability [33] (Table 2).
Alternate reservoir placement / submuscular
ARP has become increasingly popular with efforts to reduce the risk of visceral and vascular complications during prosthesis placement. A recent systematic review included 70 articles and over 9500 patients, of which, 67% underwent ARP. There were no statistical differences in safety, efficacy, or patient satisfaction between SOR and ARP reservoir location [34].
Admittedly, the submuscular space is a more nuanced location to navigate compared to SOR and as such learning appropriate technique is important for replicable outcomes. (Fig. 4) This was demonstrated by a cadaveric study performed by Ziegelmann et al. [35]. Following high submuscular (HSM) reservoir placement, 20 cadavers were assessed for true reservoir landing location. Twenty percent of reservoirs were found unintentionally located within the SOR, retroperitoneum, or peritoneal cavity. In clinical practice, Gross et al. identified 2 cases of intraperitoneal placement in their series of 2687 virgin IPP patients, both patients had a low BMI (<18.5) and a history of tobacco use [33].
Several ARP techniques have been described over the decades, however the most common is submuscular placement (Fig. 5). This was originally described by Wilson et al. in 2002 and is accomplished through either a lower abdominal counter incision or through the inguinal ring by placing the reservoir in the space anterior to the transversalis fascia and below the rectus muscle [10]. A HSM location traditionally positions the reservoir approximately 7–8 cm above the inguinal ring is thought to decrease palpability and risk of herniation [36, 37]. Placement into this location is most commonly aided by a long grasping clamp passed through the ring both to develop the space and then place the reservoir [38] (Fig. 6).
High submuscular placement involves identification of the external inguinal ring, anterior traction on the ring with a deaver, passage of the ring clamp through the ring– below the deaver and above the transversalis fascia to create a space, passage of the reservoir into this space, and finally filling.
ARP above the transversalis fascia decreases the risk of catastrophic visceral and vascular complications. In a retrospective review of 872 prosthetic cases, HSM placement was associated with a deep pelvic injury rate of 0.5% compared to 1.9% for SOR placement (p = 0.14) [13]. Other studies have reported a complete absence of visceral or vascular injuries with HSM placement [37, 39]. Further, Baumgarten et al. described a modified “Five Step Technique” to ensure accurate placement above the transversalis fascia, far from the external ring and found that this technique reduced rates of reservoir herniation from 5.3% to 1% [37]. A separate review of 2687 patients found a reservoir herniation rate of 0.09% in the SOR group vs 1.34% in ARP patients (p > 0.05) [28]. Similarly, a prospective multicenter study of 744 patients reported a reservoir hernia rate of 0.5% in SOR vs, 1% in ARP [39].
Measures to reduce herniation risk have included a purse string suture prophylactically placed at the inguinal ring [39], low transfascial fixation in which reservoir tubing is passed through the external fascia [40], and Tubing, Hitch, and Lasso, Intussusception Anchor which tacks the tubing to the fascia using a permanent suture and an extra tubing collar [41]. Another reliable method to avoid reservoir herniation is avoidance of the inguinal ring by way of a counter incision, Van Dyke et al. reported no herniations in cases utilizing a counter incision compared to 2.8% herniation rate in transinguinal HSM cases [42].
Another concern with more superficial submuscular placement of a reservoir is palpability of the device and detriment to patient satisfaction (Fig. 7). In reality, ARP may be associated with some palpability but in many cases it does not seem to significantly contribute to patient bother. In a retrospective review of 158 HSM implants, 80% were not palpable, 16% were minimally palpable by patient report and 20% were palpable to the surgeon. Overall, they reported a 1.3% revision rate due to bothersome palpability [43].
In a 2015 study, patients that underwent HSM reservoir placement reported 85.9% of patients were satisfied and there were no reported issues with palpability or autoinflation in either group [39]. Further, Osmonov et al. demonstrated an 88% satisfaction rate in the HSM group versus an 81% satisfaction with SOR (p < 0.001). Interestingly, 64.3% of the HSM group reported palpability immediately after surgery, which decreased to 20% 3 months after surgery [44]. Other high volume implant institutions have performed ARP with flat reservoirs and report minimal palpability with patient satisfaction rates as high as 94% [13, 45]. Stember et al. published their outcomes of ARP in 2239 patients and found that 3.4% of patients reported a palpable reservoir, though revision rate for palpability was only 0.4% [46]. With these data in mind, the European Society for Sexual Medicine has issued statements that ectopic reservoir placement can be considered an alternate method of reservoir placement during IPP and that device palpability does not appear to be associated with revision rates [47].
Revision rates for ARP compared to SOR reservoirs appear favorable [39, 48]. Baumgarten et al. published a study of 733 patients that underwent either HSM or SOR reservoir placement and the HSM group had a 2.3% revision rate for hernias and delayed bowel obstruction vs 4.6% revision rate in SOR group for one bladder erosion, two vascular injuries, and three herniations (p = 0.22) [37]. Similarly, Hernandez et al. published their 5-year multi-institutional experience in 2019 that analyzed 612 patients that underwent HSM placement versus 362 patients with reservoir placement in SOR, and noted no significant difference in rates of revision (p = 0.44) [49].
Counter incision use in ARP
In settings of altered anatomy or obscured inguinal rings, a counter incision (CI) is an alternative approach to HSM placement. A lower quadrant incision is carried down to fascia which is opened followed by spreading of the rectus muscle to identify the submuscular space.
Grimberg et al. reported on a cohort of 534 patients, of which 51 (9.5%) underwent CI for reservoir placement. CI had a higher median operative time with similar rates of infection, hematoma, and device malfunction [50]. A separate retrospective study compared a CI technique to a transinguinal approach in 456 virgin IPP patients. Only 7.5% of their cohort required a CI with operating time being significantly longer in the CI group, but with similar rates of infection, postoperative morphine requirements, and outpatient narcotic prescriptions. There were no reservoir herniations or vascular injuries in either group [42].
Lateral retroperitoneal and other less common locations
The lateral retroperitoneal (LR) approach requires an incision just medial to the anterior superior iliac spine where the external fascia is entered, abdominal wall musculature spread, and underlying peritoneum swept medially to identify a landing space overlying the psoas muscle. In this way, it is similar to access for retroperitoneoscopic surgery. LR placement was described in 2010 with 29 patients following radical prostatectomy. This series demonstrated no complications or injuries, similar operative time as controls, and no infections or mechanical failures at 28 months of follow up [51]. The experience of Loh-Doyle et al. with IPP placement after radical cystectomy has solidified this ARP location as a potential tool for difficult cases [32]. In their largest series, they retrospectively reviewed LR placement in 266 patients and found no statistical difference in intraoperative RP-related outcomes compared to SOR, but did have one reported intraoperative bowel injury in the LR group. Both groups had 1 patient with palpability or pain at the reservoir insertion site [52].
Less commonly, subcutaneous reservoir placement has been employed [53]. Mykoniatis et al. briefly discussed the utilization of subcutaneous reservoir placement in men with higher BMIs and a thick abdominal fat layer to provide appropriate concealment of the reservoir [54]. In 2016, Garber et al. published a retrospective series that looked at palpability and herniation rates following subcutaneous reservoir placement in 8 patients and found that 87.5% of patients and surgeons were unable to palpate the reservoirs, though average BMI in this cohort was 39 kg/m2 [55]. Though it is a possible ARP location, its use in contemporary implants is limited with submuscular position typically being a readily available alternative.
ARP techniques are appropriate options in patients with prior pelvic or inguinal surgeries and are now preferred by many high-volume implant surgeons. In 2013, Karpman et al. surveyed 95 urologists, of which 81% were experienced implant surgeons. The majority agreed that robotic prostatectomies make orthotopic reservoir placement more difficult and the capacity to perform ARP is advantageous and should be included in physician training courses [56]. A separate survey of HSM reservoir perceptions completed by 25 urologists from 8 states reported that HSM reservoir placement was overall safer (p < 0.001) with a lower risk of visceral (p < 0.001) and vascular (p < 0.001) complications, a short learning curve (p = 0.008), and easily reproducible (p = 0.002). Sixty-eight percent of surveyed surgeons preferred HSM placement, with an increase to 78% when adjusted for high-volume implanter responses only [57]. Still others have suggested that ARP in the submuscular space should now be the default location of choice for prosthetic surgeons due to its favorable safety profile [25, 38].
Conclusions
Contemporary reservoir placement locations include orthotopic/space of Retzius and alternate reservoir placement in the submuscular or lateral retroperitoneal space. Each approach has merits; knowledge and familiarity with each will equip the prosthetic surgeon to deploy reservoirs in such a way as to maximize both safety and functional outcome.
References
Hatzichristodoulou G. Surgical therapy as constant future gold standard for penile disorders. Int J Impot Res. 2020;32:1. https://doi.org/10.1038/s41443-019-0164-5.
Scott FB, Bradley WE, Timm GW. Management of erectile impotence. Use of implantable inflatable prosthesis. Urology. 1973;2:80–2.
Vakalopoulos I, Kampantais S, Ioannidis S, Laskaridis L, Dimopoulos P, Toutziaris C, et al. High patient satisfaction after inflatable penile prostheses implantation correlates with female partner satisfaction. J Sex Med. 2013;10:2774–81.
Beirnaert J, Pinar U, Benarroche D, Akakpo W, Rouprêt M. Evaluation of patient satisfaction using the validated French version of the SSIPI questionnaire after inflatable penile implantation. J Sex Med. 2023;21:67–71.
La J, Loeb CA, Barham DW, Miller J, Chung E, Gross MS, et al. Satisfaction rates of inflatable penile prosthesis in men who have sex with men are high. Int J Impot Res. 2023;35:564–8.
Cinar NB, Saribacak A, Atwater BL, Gross MS, Wilson SK, Culha M. Patient satisfaction study for the new Rigicon Infla10 inflatable penile prosthesis including single surgeon safety and outcomes data. J Sex Med. 2025;22:344–8.
Miller LE, Khera M, Bhattacharyya S, Patel M, Nitschelm K, Burnett AL. Long-term survival rates of inflatable penile prostheses: systematic review and meta-analysis. Urology. 2022;166:6–10.
Dhar NB, Angermeier KW, Montague DK. Long-term mechanical reliability of AMS 700CX/CXM inflatable penile prosthesis. J Urol. 2006;1761:2599–601.
Wilson SK, Delk JR, Salem EA, Cleves MA. Long-term survival of inflatable penile prostheses: single surgical group experience with 2,384 first-time implants spanning two decades. J Sex Med. 2007;41:1074–9.
Wilson SK, Henry GD, Delk JR, Cleves MA. The mentor Alpha 1 penile prosthesis with reservoir lock-out valve: effective prevention of auto-inflation with improved capability for ectopic reservoir placement. J Urol. 2002;168:1475–8.
Henry G, Hsiao W, Karpman E, Bella AJ, Carrion R, Jones L, et al. A guide for inflatable penile prosthesis reservoir placement: pertinent anatomical measurements of the retropubic space. J Sex Med. 2014;11:273–8.
Oberlin DT, Matulewicz RS, Bachrach L, Hofer MD, Brannigan RE, Flury SC. National practice patterns of treatment of erectile dysfunction with penile prosthesis implantation. J Urol. 2015;193:2040–4.
Pagliara TJ, Viers BR, Scott J, Morey AF. Extended experience with high submuscular placement of urological prosthetic balloons and reservoirs: refined technique for optimal outcomes. Urol Pract. 2018;5:293–8.
Kavoussi M, Cook GS, Nordeck SM, Dropkin BM, Joice GA, Badkhshan S, et al. Radiographic assessment of inflatable penile prosthesis reservoir location variability in contemporary practice. J Sex Med. 2021;18:2039–44.
Schardein JN, Trussell JC. Reservoir induced bladder rupture: a complication of inflatable penile prosthesis revision surgery. Can J Urol. 2021;28:10946–52.
Garber BB, Morris A. Intravesical penile implant reservoir: case report, literature review, and strategies for prevention. Int J Impot Res. 2013;25:41–4.
Kramer AC, Chason J, Kusakabe A. Report of two cases of bladder perforation caused by reservoir of inflatable penile prosthesis. J Sex Med. 2009;6:2064–7.
Abboudi H, Bolgeri M, Nair R, Chetwood A, Symes A, Thomas P. “A reservoir within a reservoir” - An unusual complication associated with a defunctioned inflatable penile prosthesis reservoir. Int J Surg Case Rep. 2014;5:758–60.
Clavell-Hernández J, Shah A, Wang R. Non-infectious reservoir-related complications during and after penile prosthesis placement. Sex Med Rev. 2019;7:521–9.
Cui T, Terlecki R, Mirzazadeh M. Infrequent reservoir-related complications of urologic prosthetics: a case series and literature review. Sex Med. 2015;3:334–8.
Selph JP, McKim SE, Langston JP, Carson CC. Deep venous thrombosis as a complication of reservoir placement in post-prostatectomy erectile dysfunction and urinary incontinence prosthetic surgery. Sex. Med Rev. 2014;2:59–63.
da Justa DG, Bianco FJ, Ogle A, Dhabuwala CB. Deep venous thrombosis due to compression of external iliac vein by the penile prosthesis reservoir. Urology 2003;61:462.
Deho’ F, Henry GD, Marone EM, Sacca’ A, Chiesa R, Rigatti P, et al. Severe vascular complication after implantation of a three‐piece inflatable penile prosthesis. J Sex Med. 2008;5:2956–9.
Brison D, Ilbeigi P, Sadeghi-Nejad H. Reservoir repositioning and successful thrombectomy for deep venous thrombosis secondary to compression of pelvic veins by an inflatable penile prosthesis reservoir. J Sex Med. 2007;42:1185–7.
Perito P, Wilson S. The history of nontraditional or ectopic placement of reservoirs in prosthetic urology. Sex Med Rev. 2016;4:190–3.
Hakky T, Lentz A, Sadeghi-Nejad H, Khera M. The evolution of the inflatable penile prosthesis reservoir and surgical placement. J Sex Med. 2015;12:464–7.
Pastuszak AW, Lentz AC, Farooq A, Jones L, Bella AJ. Technological improvements in three-piece inflatable penile prosthesis design over the past 40 years. J Sex Med. 2015;12:415–21.
Van Dyke M, Baumgarten AS, Ortiz N, Hudak SJ, Morey AF. State of the reservoir: current concepts of penile implant reservoir placement and potential complications. Curr Urol Rep. 2021;22:20.
Levine LA, Hoeh MP. Review of penile prosthetic reservoir: complications and presentation of a modified reservoir placement technique. J Sex Med. 2012;9:2759–69.
Lane BR, Abouassaly R, Angermeier KW, Montague DK. Three-piece inflatable penile prostheses can be safely implanted after radical prostatectomy through a transverse scrotal incision. Urology 2007;70:539–42.
Falcone M, Pucci L, Garaffa G, Cocci A, Gillo A, Capece M, et al. An outcomes analysis of penile prosthesis implantation following radical cystoprostatectomy and urinary diversion: a multicentric retrospective cohort study. Int J Impot Res. 2020;32:126–32.
Loh-Doyle J, Patil MB, Sawkar H, Wayne K, Boyd SD. 3-piece inflatable penile prosthesis placement following radical cystoprostatectomy and urinary diversion: technique and outcomes. J Sex Med. 2018;15:907–13.
Gross MS, Stember DS, Garber BB, Perito PE. A retrospective analysis of risk factors for IPP reservoir entry into the peritoneum after abdominal wall placement. Int J Impot Res. 2017;29:215–8.
Atwater B, Krug A, Gross MS, Marty-Roix R, Chapin L, Morey AF. A review of the safety and efficacy of inflatable penile prosthesis ectopic reservoir placement. Sex Med Rev. 2025;13:20–32.
Ziegelmann MJ, Viers BR, Lomas DJ, Westerman ME, Trost LW. Ectopic penile prosthesis reservoir placement: an anatomic cadaver model of the high submuscular technique. J Sex Med. 2016;13:1425–31.
Morey AF, Cefalu CA, Hudak SJ. High submuscular placement of urologic prosthetic balloons and reservoirs via transscrotal approach. J Sex Med. 2013;10:603–10.
Baumgarten AS, Kavoussi M, VanDyke ME, Ortiz NM, Khouri RK, Ward EE, et al. Avoiding deep pelvic complications using a “Five-Step” technique for high submuscular placement of inflatable penile prosthesis reservoirs. BJU Int. 2020;126:457–63.
Wilson SK, Simhan J, Osmonov D. Should occasional implanters learn ectopic placement of IPP reservoirs? Int J Impot Res. 2020;32:371–8.
Karpman E, Brant WO, Kansas B, Bella AJ, Jones LA, Eisenhart E, et al. Reservoir alternate surgical implantation technique: preliminary outcomes of initial PROPPER study of low profile or spherical reservoir implantation in submuscular location or traditional prevesical space. J Urol. 2015;193:239–44.
Khoei A, Racik N, Bansal U, Flores F, Khera M. The low submuscular reservoir placement with transfascial fixation for inflatable penile prostheses. J Sex Med. 2022;19:1309–12.
Yang D, Heslop D, Houlihan M, Helo S, Ziegelmann M, Köhler TS. The tubing, hitch and lasso, intussusception anchor (THALIA) technique: a novel approach to fixate the penile implant reservoir. J Sex Med. 2021;18:224–9.
VanDyke ME, Kavoussi M, Langford BT, Badkhshan S, Nealon SW, Franzen BP, et al. Increasing role of counterincision for high submuscular penile prosthesis reservoir placement. J Sex Med. 2023;20:205–9.
Chung PH, Morey AF, Tausch TJ, Simhan J, Scott JF. High submuscular placement of urologic prosthetic balloons and reservoirs: 2-year experience and patient-reported outcomes. Urology 2014;84:1535–40.
Osmonov D, Chomicz A, Tropmann-Frick M, Arndt KM, Jünemann KP. High-submuscular vs. space of Retzius reservoir placement during implantation of inflatable penile implants. Int J Impot Res. 2020;32:18–23.
Baumgarten AS, Kavoussi M, Ortiz NM, Khouri RK, Ward EE, Hudak SJ, et al. High submuscular IPP reservoir placement: the “Five-Step” technique. Urology 2020;145:298.
Stember DS, Garber BB, Perito PE. Outcomes of abdominal wall reservoir placement in inflatable penile prosthesis implantation: a safe and efficacious alternative to the space of Retzius. J Sex Med. 2014;11:605–12.
Osmonov D, Christopher AN, Blecher GA, Falcone M, Soave A, Dahlem R, et al. Clinical Recommendations From the European Society for Sexual Medicine Exploring Partner Expectations, Satisfaction in Male and Phalloplasty Cohorts, the Impact of Penile Length, Girth and Implant Type, Reservoir Placement, and the Influence of Comorbidities and Social Circumstances. J Sex Med. 2020;17:210–37.
Capoccia EM, Phelps JN, Levine LA. Modified inflatable penile prosthesis reservoir placement into space of retzius: comparing outcomes in men with or without prior pelvic surgery. J Sex Med. 2017;14:968–73.
Hernández JC, Trost L, Köhler T, Ring J, Traweek R, Alom M, et al. Emerging complications following alternative reservoir placement during inflatable penile prosthesis placement: a 5-year multi-institutional experience. J Urol. 2019;201:581–6.
Grimberg D, Wang S, Carlos E, Nosé B, Harper S, Lentz AC. Counter incision is a safe and effective method for alternative reservoir placement during inflatable penile prosthesis surgery. Transl Androl Urol. 2020;9:2688–96.
Hartman RJ, Helfand BT, McVary KT. Outcomes of lateral retroperitoneal reservoir placement of three-piece penile prosthesis in patients following radical prostatectomy. Int J Impot Res. 2010;22:279–83.
Loh-Doyle JC, Lin JS, Doumanian LR, Patil MB, Boyd SD. Outcomes of alternative reservoir placement in the lateral retroperitoneum during inflatable penile prosthesis placement. Urology 2021;152:35–41.
Smaldone MC, Cannon GM, Benoit RM. Subcutaneous reservoir placement during penile prosthesis implantation. Can J Urol. 2006;13:3351–2.
Mykoniatis I, Osmonov D, Van Renterghem K. A modified surgical technique for reservoir placement during inflatable penile prosthesis implantation. Sex Med. 2020;8:378–82.
Garber BB, Bickell M. Subcutaneous placement of inflatable penile prosthesis reservoirs. Urology. 2016;88:93–6.
Karpman E, Sadeghi-Nejad H, Henry G, Khera M, Morey AF. Current opinions on alternative reservoir placement for inflatable penile prosthesis among members of the Sexual Medicine Society of North America. J Sex Med. 2013;10:2115–20.
Tausch TJ, Morey AF, Zhao LC, Knoll P, Simhan J, Scott JF, et al. High submuscular versus space of Retzius placement of inflatable penile prosthesis reservoirs: results of a surgeon survey. Can J Urol. 2014;21:7465–9.
Author information
Authors and Affiliations
Contributions
Authors SI, JP, FM, and JS all contributed to the following: Conception and design of the work. Drafting and revision of the manuscript. Approval of the final version of the manuscript. Accountability for all aspects of and accuracy of the work presented.
Corresponding author
Ethics declarations
Competing interests
JS is a consultant for Boston Scientific and Coloplast Corporation. SI, JP, and FM declare no competing interests.
Ethical approval
This work is a review of publicly available published data and did not collect any novel human subject data making it exempt from formal ethics committee evaluation. Any patient photos are published with informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ivan, S., Pryor, J., Maffucci, F. et al. Reservoir placement options: a state of the art review. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01082-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41443-025-01082-x
This article is cited by
-
Comment on: reservoir migration in inflatable penile prostheses: a systematic review and development of a clinical decision algorithm
International Journal of Impotence Research (2025)