Abstract
Treatment requests in transgender healthcare are heterogenous and not all transgender and gender-diverse individuals want to undergo the various transition-related medical interventions offered. This study aims to explore demographic and treatment-related predictors associated with different transgender care pathways in a multicenter, multinational clinical setting. In this follow-up study, 539 adult participants from Belgium, Germany, and the Netherlands took part and were categorized as following a ‘traditional’ care pathway (i.e., undergoing all transition-related interventions), an ‘individual’ care pathway (i.e. any course of treatment deviating from the traditional pathway), or ‘no care’ pathway (i.e. not seeking transition-related medical interventions.). We analyzed differences in demographic (e.g., gender identity) and clinical variables (e.g., treatment satisfaction), conducting logistic regression analysis and descriptive subgroup analysis. Participants with a non-binary gender were 6.7 times more likely to follow an individual care pathway, while participants with higher treatment satisfaction were less likely to follow an individual care pathway (Odds Ratio: 0.6). We identified four patterns of individual transgender care pathways, some as a function of the sex assigned at birth. The present study provides valuable insights into demographic and treatment-related predictors associated with different transgender care pathways. Healthcare providers should be aware of individual transgender care pathways and the association with (non)-binary genders to provide tailored transgender healthcare and ensure individualized, high-quality service provision.
Similar content being viewed by others
Introduction
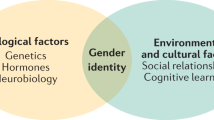
Transgender and gender-diverse (TGD) individuals experience their gender to be different from the sex they were assigned to at birth. They might identify binary as the ‘opposite’ gender (man, woman) or non-binary. Non-binary individuals experience themselves as moving between male and female (e.g., genderfluid), beyond the gender binary (e.g., genderqueer), or do not identify with any kind of gender at all (e.g., agender) [1]. Additionally, non-binary individuals can include a variety of additional cultural and personal experiences, including identities rooted in specific traditions or languages, such as Two-Spirit in some Indigenous cultures. However, all of these concepts are not mutually exclusive, and people might use multiple terms to describe their identity (e.g., genderqueer trans woman). Gender-affirming care for TGD individuals focuses on medical interventions to support a person’s transition to living according to their gender. This includes mental health counseling (e.g., to cope with minority stress) [2], hormone therapy, gender-affirming surgery (e.g., genital reconstructive surgeries), and additional interventions (e.g., hair removal, speech therapy [3], in the following: transition-related interventions [4]). Transition-related medical interventions contribute to lower gender dysphoria and increase mental health and quality of life in TGD individuals [5,6,7,8,9,10]. A transgender healthcare pathway is the individual course of various medical interventions a person follows to help them transition into their gender socially and physically. Historically, the expectation of a linear course of treatment, where TGD individuals undergo most or all transition-related interventions, ending with gender-affirming genital surgery, has dominated transgender healthcare [11,12,13,14]. However, not all TGD individuals want to follow a ‘traditional’ care pathway [13, 15,16,17]. Following such individual care pathways, some TGD individuals, for example, only access hormone treatment or single surgical procedures (e.g., mastectomy) but do not desire gender-affirming genital surgery [15] (Fig. 1). Data from the U.S. indicate that overall, about 11% of TGD individuals undergo gender-affirming genital surgery, while 80% of those who underwent some kind of gender-affirming procedure had gender-affirming genital surgery [18]. It is important to notice that undergoing gender-affirming genital surgery is also influenced by how legal gender recognition is regulated in a country. In several European countries, undergoing these procedures was or still is a mandatory requirement for changing one’s name or gender on birth certificates and other official documents [19].
Reasons for not undergoing gender-affirming genital surgery appear to be manifold and include non-binary gender identities [15, 20], a significant lowering of gender dysphoria by other interventions, fear of medical complications [21, 22], limited genital dysphoria [13], and general barriers to transgender healthcare (affordability, lack of insurance coverage, discrimination by healthcare providers) [23,24,25,26].
There is still limited research investigating what individual characteristics of TGD individuals and circumstantial factors of transgender healthcare contribute to the variety of individual care pathways. By exploring demographic and treatment-related predictors associated with individual and traditional care pathways, this study aims to contribute to a more comprehensive picture of individual treatment requests of TGD individuals.
Methods
Study design
The present analysis is part of a follow-up study carried out within the European Network for the Investigation of Gender Incongruence (ENIGI) [27]. The study was developed as a paper-pencil and web-based survey to investigate adult TGD individuals at three specialized clinics (Amsterdam, Ghent, Hamburg). At baseline, the study’s goal was to include all individuals older than 17 years of age who attended one of the clinics. Therefore, no additional inclusion criteria needed to be defined. At follow-up, the goal was to include all participants who participated at baseline within the study period of interest. Exclusion criteria were the lack of sufficient information regarding treatment or incomplete questionnaire data. TGD individuals who completed the assessment protocol (people who gave informed consent and filled out the ENIGI baseline questionnaires and a series of standardized questionnaires handed out at the initial counseling session) between 2007 and 2009 were contacted between July and September 2013 (follow-up 1). TGD individuals who completed the assessment protocol between 2011 and 2013 were contacted between September 2017 and April 2018 (follow-up 2). The 2010 cohort was excluded to obtain similar follow-up periods. The local ethics committees approved the initial and the follow-up studies (Amsterdam: METc 2008.108 (A2017.342); Ghent: 2013/153; Hamburg: 12/2017-PTK-HH).
Participants
Participants were invited by phone, e-mail, or regular mail to fill out an online follow-up survey. All participants gave informed consent. A total of 1089 TGD individuals were invited for the study. 550 individuals (response rate: 50.51%) both consented and filled out the survey (Amsterdam, n = 295; Ghent, n = 157; Hamburg, n = 98). Of these 550 participants, 11 participants were excluded because we lacked sufficient information concerning their treatment. Therefore, 539 participants were included in the final analysis.
Measures
Biographical data (e.g., age) and clinical information (e.g., gender) were assessed by a self-developed questionnaire. The sex assigned at birth was assessed by the clinical records. Participants were asked to indicate their gender (male, female, trans woman, trans men, in between, other) and specify their answer by free text if necessary. Afterward, we categorized gender as binary (woman, trans woman, man, trans man) or non-binary (in between, non-binary gender identity specified in the ‘other’ option). Participants were asked what transition-related medical interventions they had received. Due to inconsistencies and missing information in the self-report data, information on transition-related interventions was also retrieved from clinical records. Inconsistencies were resolved by checking clinical records. All participants were asked if they intended to seek further transition-related interventions. Based on the treatment data, we constructed a polytomous (divided into more than two parts or categories) outcome of belonging to a “traditional transgender care pathway (TCP)”, an “individual transgender care pathway (ICP)”, and a “no transgender care pathway (NCP)”. By being assigned to the TCP group, a participant undergoes or plans to undergo hormone treatment, top surgery (breast augmentation, mastectomy), surgery of the internal sex organs (i.e., gonads), and surgery of the external sex organs (i.e., vagina, vulva, and penis). An ICP is defined as any course deviating from the traditional treatment pathway (e.g., a person who receives hormone therapy and underwent surgery of the internal sex organs, but not of the external sex organs). Participants from the NCP group have or had no intentions of undergoing any transition-related medical interventions (Fig. 1).
Treatment satisfaction and satisfaction with physical appearance were assessed using 5-point Likert scales. If complications occurred, participants were asked to specify these. Traumatic events (e. g. serious physical injuries), chronic health concerns, medication besides hormones, and hospitalization for mental health concerns were asked using yes-no questions. A detailed description of the measures and references to the questionnaires used can be found in the supplementary material.
Statistical analysis
IBM SPSS Statistics, version 27, was used for statistical analyses. We conducted bivariate analyses across each of the basic demographics and clinical information to examine significant associations with the primary outcome of interest (belonging to one of the transgender care pathways). All statistical comparisons were made between all three groups (TCP, ICP, NCP) and between the ICP and the TCP group separately. χ2 tests were calculated to assess differences in categorical variables. Cramer V was calculated to measure the strength of the relationship. As the data did not fit the assumptions for parametric statistics (i.e., homogeneity of variance), Kruskal-Wallis-tests and Mann-Whitney U-tests were calculated to determine differences between the groups in continuous variables. The Dunn’s-test was used for post-hoc pairwise comparisons. Comparisons between the countries were also calculated and can be found in the supplementary material. To create a prediction model of belonging to one of the care pathways (ICP, TCP), we conducted logistic regression analyses. The NCP group was excluded from the regression analysis due to the small number of cases. We entered all covariates that showed statistical significance in the bivariate analyses. The covariates were entered block-wise in the model (Demographics, treatment-related predictors). In case of missing data, participants were excluded listwise. We bootstrapped confidence intervals of the regression weights based on 5000 samples. Hosmer & Lemeshow, Cox & Snell, and Nagelkerke R2 were used as coefficients of determination. We conducted diagnostics on all relevant variables to check the assumptions for logistic regression models (e.g., independence of errors, incomplete information from the predictors). Cohens f2 was calculated as an effect size measure for the logistic regression model. To deal with the problem of multiple comparisons, a Bonferroni correction [28] was adopted with the statistical significance set for a p-value less than 0.002 (0.05 divided by 28).
Finally, we performed a descriptive subgroup analysis of the ICP group, assessing the participants’ different individual treatment pathways and associated demographic factors (sex assigned at birth, non-binary gender).
Results
The total sample consisted of 539 participants. Two hundred fifty individuals were assigned to the TCP group, 262 to the ICP group, 27 to the NCP group. Demographic characteristics of the sample and differences between the groups are presented in Table 1. Regarding certainty about one’s gender, post-hoc Dunn’s-test found that the NCP group felt less certain about their gender than both the TCP group (z = 167.6, p = 0.000) and the ICP group (z = 166.3, p = 0.000). For satisfaction with physical appearance, post-hoc Dunn’s-test found that only the TCP group and the NCP group differed but did not survive Bonferroni correction (z = 154.4, p = 0.043). The NCP group felt less satisfied with their physical appearance than the TCP group.
Due to the small number of participants in the NCP group, calculations were repeated, comparing only the ICP and the TCP group. Comparing the ICP group against the TCP group, participants from the ICP group were more likely to have an income around the poverty threshold, whereas participants from the TCP group were more likely to have an income above the poverty threshold (χ2 (2, N = 495) = 11.3; p = 0.001). Individuals with non-binary gender identity were more frequent in the ICP group (χ2 (1, N = 512) = 13.4; p = 0.000). Also, the ICP group reported significantly lower treatment satisfaction (z = −3.47, p = 0.001; Table 1). No relevant differences in demographics were discovered between the three research sites. Participants from Belgium reported a higher number of traditional treatment pathways (see supplementary material).
A logistic regression model (Table 2) found that non-binary gender identity and treatment satisfaction significantly predicted group membership. Participants with a non-binary gender were 6.7 times more likely to belong to the ICP group. Participants with higher treatment satisfaction were less likely to belong to the ICP group (OR: 0.6). The model showed a small effect (f2 = 0.11). Collinearity diagnostics did not show significant multicollinearity concerns for any of the variables in the model.
Four subgroups were detected within the ICP group and are summarized in Table 3.
Discussion
In the present study, we explored demographic and clinical factors associated with individual and traditional transgender care pathways in a large multinational clinical sample of TGD individuals. Participants from Belgium reported a higher number of traditional treatment pathways. However, it is important to notice that the Belgian research site is also the one that has the longest experience with phalloplasty, which might cause individuals to consider this procedure more easily and inform themselves about it. How specific procedures offered by a center/country shape how people design their care path should be a main topic of future research as we still know very little about this potential interaction. Participants with a non-binary gender were 6.7 times more likely to undergo an individual transgender care pathway. This result is in line with previous research, reporting that non-binary TGD individuals are less likely to undergo transition-related medical interventions, especially gender-affirming genital surgery [15, 16, 29]. Prior research found that the primary sex anatomy, especially the presence or absence of a penis, contributes significantly to a distinct allocation as male or female [30]. As non-binary people usually do not follow a distinct and persistent gender allocation [1], it seems understandable that they also reject surgical procedures associated with such an assignment. Moreover, lower treatment satisfaction was associated with following an individual transgender care pathway. Lower satisfaction with previous transition-related interventions might have contributed to rejecting further interventions, even though a person had a wish for these interventions in the first place. However, the association between the continuation or discontinuation of transition-related interventions and variations in treatment satisfaction has not been investigated so far. Prior research mainly found structural circumstances (affordability, fear of discrimination from healthcare providers) as reasons for an interruption or discontinuation of transition-related interventions [29, 31,32,33,34]. Moreover, it must be noted that overall satisfaction with transition-related interventions was high in both groups (4.42 and 4.13).
A subgroup analysis of participants of the ICP group found several main individual transgender care pathways (Table 3). Around 20% of participants took hormones but did not undergo any surgery or have any plans to do so. Another 16.8% took hormones and underwent top surgery but did not plan to undergo gender-affirming genital surgery. Due to the distinctive physical effects that sex hormones can have on breast development [35] or voice pitch [36], both these groups could already have experienced a sufficient decrease of gender dysphoria and an increase in quality of life by these interventions. Limited genital dysphoria [13], fear of complications, and unsatisfactory aesthetic results must be considered as further reasons [37]. However, as our study did not provide sufficient data to support this interpretation, additional in-depth research is necessary in the future. Nearly a quarter of our participants – all assigned female at birth - followed an individual care pathway by accessing hormone therapy, top surgery, surgery of internal genital organs (hysterectomy, oophorectomy, salpingectomy), but no surgery of external genital organs (metoidioplasty, phalloplasty). This is in line with prior research reporting that TGD individuals assigned female at birth are less likely to undergo gender-affirming genital surgery than those assigned male at birth [13, 38]. The high number of complications and poor aesthetic results, especially with phalloplasty [37], need to be considered as reasons why participants in this group did not want to undergo gender-affirming surgery of the external genital organs. Moreover, the definite absence of menstruation after hysterectomy and oophorectomy might also have contributed to a significant lowering of gender dysphoria and an increase in quality of life, thus rendering further interventions unnecessary. Another group following an individual care pathway – all assigned male at birth- reported that they underwent hormone treatment, surgery of the internal (orchiectomy), and the external genital organs (vaginoplasty, penectomy; 38.5%). However, they did not undergo breast augmentation. From a clinical perspective, it must be noted that this subgroup might overlap with the group following a ‘traditional’ care pathway. Hormone therapy might have contributed to sufficient breast development [35], which is why these participants would not undergo any chest surgery, but they might have accessed the procedure if hormone therapy had not led to satisfactory breast development. In that case, they would have been classified as following a ‘traditional’ care pathway according to our grouping. However, when moving this subgroup into the TCP group and rerunning our analyses, we did not find significant changes in our results.
Finally, our study investigated a relatively small group of 27 TGD individuals who did not want to undergo any transition-related interventions. These participants might have primarily accessed care for psychological support or to evaluate their need for gender-affirming care. A high number of participants in this group reported a non-binary gender. This is in line with previous research investigating TGD individuals not seeking transition-related interventions [17]. As it has been reported repeatedly that non-binary individuals do undergo transition-related medical interventions less frequently [13, 15, 16], it is also likely that some of them do not want to undergo any treatment at all. In line with that, it has been found that some TGD individuals report that they do not experience distress associated with gender incongruence and, therefore, see no necessity for medical interventions [17]. Moreover, TGD individuals not seeking medical interventions might already experience a significant decrease in distress and an increase in quality of life by disclosing their feelings to loved ones or close friends and/or by using non-medical supplies (e.g., clothing, wigs, chest binder). However, it was noticeable that these participants reported significantly lower certainty about their gender than the other two groups (ICP, TCP). Regarding certainty about one’s gender, it could be assumed that some TGD individuals not seeking transition-related interventions are still in the phase of discovering their gender and, therefore, are unsure if they want to undergo transition-related medical interventions in the future. This struggle with questioning their gender and bodily appearance could have led to lower certainty about their gender.
Limitations
Our regression model only had a small effect (f2 = 0.11) and explained a small amount of variance (Table 2). Using a regression model, we only investigated one direction of the relationship between the variables (Predictor-Outcome). However, it can be argued that the variables used in our models might interact with each other in both directions. Therefore, our data needs to be interpreted carefully, and no absolute conclusions can be drawn from it for clinical practice. Moreover, our study does not provide a detailed look at the variance for a certain surgical procedure, e.g., people undergoing hysterectomy and salpingectomy, but not oophorectomy. Also, all the clinics were in metropolitan areas, so TGD individuals from rural areas could have been excluded [39]. Healthcare systems were, to some degree, comparable in all three countries [40]. With some exceptions (e.g., breast augmentation in the Netherlands), coverage for most gender-affirming healthcare services was available in all three countries, too [41]. The assessment period was fixed and not related to the time of an individual finalization of treatment. This means that TGD individuals were invited to participate in a follow-up at a fixed point in time, irrespective of their individual need to further continue treatment or not. Therefore, some of the treatment pathways may not have been “finalized”. The classification of transgender care pathways into distinct groups only insufficiently represents the actual diversity of treatment requests of TGD individuals. Also, it does not incorporate any information on social gender affirmation, which could have an important influence on which transition-related interventions a person wants to undergo. It is also important to notice that, even though non-binary TGD individuals were more likely to undergo an ICP, approximately half of the participants identifying with binary gender wanted to undergo an ICP, too. Therefore, choosing an individual pathway of care is not exclusively associated with identifying as non-binary. Finally, as participants were recruited at specialized clinics rather than as a community sample, individuals who are not interested in gender-affirming care can be expected to be underrepresented.
Conclusion
In conclusion, the present study highlights the various factors influencing transgender care pathways and highlights the complexity of individual gender-affirming care. With the goal of improving treatment satisfaction for TGD individuals, future research should focus on understanding how structural circumstances intersect with individual treatment preferences and influence transgender care pathways.
Data availability
We will consider sharing de-identified, individual participant-level data that underline the results reported in this article on receipt of a request detailing the study hypothesis and statistical analysis plan. All requests should be sent to the corresponding author. The corresponding author and lead investigators of this study will discuss all requests and make decisions about whether data sharing is appropriate based on the scientific rigor of the proposal. All applicants will be asked to sign a data access agreement.
References
Richards C, Bouman WP, Seal L, Barker MJ, Nieder TO, T’Sjoen G. Non-binary or genderqueer genders. Int Rev Psychiatry. 2016;28:95–102.
Lefevor GT, Boyd-Rogers CC, Sprague BM, Janis RA. Health disparities between genderqueer, transgender, and cisgender individuals: an extension of minority stress theory. J Counseling Psychol. 2019;66:385.
Safer JD, Tangpricha V. Care of transgender persons. N Engl J Med. 2019;381:2451–60.
Coleman E, Radix A, Bouman W, Brown G, De Vries A, Deutsch M, et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgender Health. 2022;23:S1–S259.
Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388:412–36.
Dhejne C, Van Vlerken R, Heylens G, Arcelus J. Mental health and gender dysphoria: a review of the literature. Int Rev Psychiatry. 2016;28:44–57.
van Leerdam TR, Zajac JD, Cheung AS. The effect of gender-affirming hormones on gender dysphoria, quality of life, and psychological functioning in transgender individuals: a systematic review. Transgend Health. 2023;8:6–21.
Swan J, Phillips TM, Sanders T, Mullens AB, Debattista J, Brömdal A. Mental health and quality of life outcomes of gender-affirming surgery: a systematic literature review. J Gay Lesbian Ment Health. 2023;27:2–45.
Chen D, Berona J, Chan Y-M, Ehrensaft D, Garofalo R, Hidalgo MA, et al. Psychosocial functioning in transgender youth after 2 years of hormones. N Engl J Med. 2023;388:240–50.
Grant R, Amos N, Lin A, Cook T, Hill AO, Pang K, et al. Mental health and wellbeing outcomes associated with social, medical, and legal gender affirmation among trans young people in Australia. Int J Transgend Health. 2024:1–13.
Cohen-Kettenis PT, Pfäfflin F. The DSM diagnostic criteria for gender identity disorder in adolescents and adults. Arch Sex Behav. 2010;39:499–513.
Richards C, Barker M, Lenihan P, Iantaffi A. Who watches the watchmen? A critical perspective on the theorization of trans people and clinicians. Feminism Psychol. 2014;24:248–58.
Beek TF, Kreukels BP, Cohen‐Kettenis PT, Steensma TD. Partial treatment requests and underlying motives of applicants for gender affirming interventions. J Sex Med. 2015;12:2201–5.
Nieder TO, Strauss B. Transgender health care in Germany: participatory approaches and the development of a guideline. Int Rev Psychiatry. 2015;27:416–26.
Koehler A, Eyssel J, Nieder TO. Genders and individual treatment progress in (non-) binary trans individuals. J Sex Med. 2018;15:102–13.
Scheim AI, Bauer GR. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. J Sex Res. 2015;52:1–14.
Nieder TO, Eyssel J, Köhler A. Being trans without medical transition: Exploring characteristics of trans individuals from Germany not seeking gender-affirmative medical interventions. Arch Sex Behav 2019;49:2661–72.
Canner JK, Harfouch O, Kodadek LM, Pelaez D, Coon D, Offodile AC, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;153:609–16.
Argren, Rigmor, et al. “The evolving recognition of gender in international and European law”. Gender-competent legal education. 2023;261.
Taylor J, Zalewska A, Gates JJ, Millon G. An exploration of the lived experiences of non-binary individuals who have presented at a gender identity clinic in the United Kingdom. Int J Transgend. 2019;20:195–204.
Otto-Moudry R, Kinney LM, Butcher RL, Blasdel G, Brown LK, Elwyn G, et al. Exploring decisional conflict experienced by individuals considering metoidioplasty and phalloplasty gender-affirming surgery. Plast Reconstr Surg–Glob Open. 2024;12:e5840.
Nolan IT, Poudrier G, Motosko CC, Cook TE, Saia W, Gothard MD, et al. Continued barriers to top surgery among transgender men. Plast Reconstr Surg. 2020;145:464e–5e.
Safer JD, Coleman E, Feldman J, Garofalo R, Hembree W, Radix A, et al. Barriers to health care for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23:168.
White Hughto JM, Rose AJ, Pachankis JE, Reisner SL. Barriers to gender transition-related healthcare: identifying underserved transgender adults in Massachusetts. Transgend Health. 2017;2:107–18.
Lerner JE, Robles G. Perceived barriers and facilitators to health care utilization in the United States for transgender people: a review of recent literature. J Health Care Poor Underserved. 2017;28:127–52.
James S, Herman J, Rankin S, Keisling M, Mottet L, Anafi M. The report of the 2015 US transgender survey 2016 [Available from: http://www.transequality.org/sites/default/files/docs/USTS-Full-Report-FINAL.PDF.
Kreukels B, Haraldsen I, De Cuypere G, Richter-Appelt H, Gijs L, Cohen-Kettenis P. A European network for the investigation of gender incongruence: the ENIGI initiative. Eur Psychiatry. 2012;27:445–50.
Bonferroni C. Teoria statistica delle classi e calcolo delle probabilita. Pubblicazioni del R Istituto Superiore di Scienze Economiche e Commericiali di Firenze. 1936;8:3–62.
Sun HH, Gillani B, Rhodes S, Hamilton D, Gupta S, Banik S, et al. Does every transgender person want gender affirming surgery? A survey of transgender individuals in the Midwestern United States. Int J Impot Res. 2024:1–6.
Wenzlaff F, Briken P, Dekker A. If there’sa penis, it’s most likely a man: Investigating the social construction of gender using eye tracking. PLoS ONE. 2018;13:e0193616.
Lehavot K, Katon JG, Simpson TL, Shipherd JC. Transgender veterans’ satisfaction with care and unmet health needs. Med Care. 2017;55:S90.
Nieto O, Brooks RA, Landrian A, Cabral A, Fehrenbacher AE. PrEP discontinuation among Latino/a and Black MSM and transgender women: a need for PrEP support services. PLoS ONE. 2020;15:e0241340.
Grant J, Mottet L, Tanis J, Herman JL, Harrison J, Keisling M. National transgender discrimination survey report on health and health care. 2010.
Kcomt L, Gorey KM, Barrett BJ, McCabe SE. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM-Population Health. 2020;11:100608.
de Blok CJM, Klaver M, Wiepjes CM, Nota NM, Heijboer AC, Fisher AD, et al. Breast development in transwomen after 1 year of cross-sex hormone therapy: results of a prospective multicenter study. J Clin Endocrinol Metab. 2018;103:532–8.
Bultynck C, Pas C, Defreyne J, Cosyns M, den Heijer M, T’Sjoen G. Self‐perception of voice in transgender persons during cross‐sex hormone therapy. Laryngoscope. 2017;127:2796–804.
Morrison SD, Chen ML, Crane CN. An overview of female-to-male gender-confirming surgery. Nat Rev Urol. 2017;14:486–500.
Eyssel J, Koehler A, Dekker A, Sehner S, Nieder TO. Needs and concerns of transgender individuals regarding interdisciplinary transgender healthcare: A non-clinical online survey. PLoS ONE. 2017;12:e0183014.
Burgwal A, Gvianishvili N, Hård V, Kata J, García Nieto I, Orre C, et al. Health disparities between binary and non binary trans people: a community-driven survey. Int J Transgenderism. 2019;20:218–29.
OECD, European Union. Health at a Glance: Europe 20222022.
Transgender Europe. Trans Health Map 2022: the state of trans healthcare in the EU 2022 [Available from: https://tgeu.org/trans-health-map-2022/.
Acknowledgements
The authors thank all the research participants for sharing their stories and experiences.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Koehler, Andreas (Conceptualization: Lead; Formal analysis: Lead; Visualization: Lead; Writing – original draft: Lead; Writing – review & editing: Lead), Becker-Hebly, Inga (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting, Methodology: Supporting; Project administration: Lead), Elaut, Els (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting, Methodology: Supporting; Project administration: Lead), Kreukels, Baudewijntje (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting, Methodology: Supporting; Project administration: Lead), Briken, Peer (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting), Heylens, Gunter (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting), Steensma, Thomas, D. (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting), Nieder, Timo (Conceptualization: Supporting; Writing – original draft: Supporting; Writing – review & editing: Supporting, Methodology: Supporting; Project administration: Lead).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The local ethics committees approved the initial and the follow-up studies (Amsterdam: METc 2008.108 (A2017.342); Ghent: 2013/153; Hamburg: 12/2017-PTK-HH). All participants gave informed consent to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koehler, A., Becker-Hebly, I., Elaut, E. et al. Traditional and individual care pathways in gender-affirming healthcare for transgender and gender-diverse individuals - results from the ENIGI follow-up study. Int J Impot Res 38, 37–43 (2026). https://doi.org/10.1038/s41443-025-01085-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41443-025-01085-8
This article is cited by
-
Comparing sexual outcomes and complications in Male-to-Female Gender-Affirming Surgery: penile inversion vs. robotic peritoneal vaginoplasty
International Journal of Impotence Research (2025)