Abstract
Platelets are key mediators of atherothrombosis, yet, limited tools exist to identify individuals with a hyperreactive platelet phenotype. In this study, we investigate the association of platelet hyperreactivity and cardiovascular events, and introduce a tool, the Platelet Reactivity ExpreSsion Score (PRESS), which integrates platelet aggregation responses and RNA sequencing. Among patients with peripheral artery disease (PAD), those with a hyperreactive platelet response (>60% aggregation) to 0.4 µM epinephrine had a higher incidence of the 30 day primary cardiovascular endpoint (37.2% vs. 15.3% in those without hyperreactivity, adjusted HR 2.76, 95% CI 1.5–5.1, p = 0.002). PRESS performs well in identifying a hyperreactive phenotype in patients with PAD (AUC [cross-validation] 0.81, 95% CI 0.68 –0.94, n = 84) and in an independent cohort of healthy participants (AUC [validation] 0.77, 95% CI 0.75 –0.79, n = 35). Following multivariable adjustment, PAD individuals with a PRESS score above the median are at higher risk for a future cardiovascular event (adjusted HR 1.90, CI 1.07–3.36; p = 0.027, n = 129, NCT02106429). This study derives and validates the ability of PRESS to discriminate platelet hyperreactivity and identify those at increased cardiovascular risk. Future studies in a larger independent cohort are warranted for further validation. The development of a platelet reactivity expression score opens the possibility for a personalized approach to antithrombotic therapy for cardiovascular risk reduction.
Similar content being viewed by others
Introduction
Platelets play a key role in atherogenesis and progression to thrombosis1,2,3. A landmark study more than three decades ago reported that increased platelet activity, measured by spontaneous platelet aggregation following a myocardial infarction (MI) off all antiplatelet therapy, was independently associated with long-term mortality and cardiovascular (CV) events3. Since then, many clinical studies have demonstrated the importance of platelet activity and CV risk4,5,6,7,8, with our group and others demonstrating the ability of platelet aggregation measures to identify populations with a hyperreactive platelet phenotype9,10.
Various technical barriers limit the routine clinical assessment of platelet aggregation responses to assess platelet hyperreactivity and CV risk11,12,13. Transcriptome analyses of platelets are increasingly used to discover novel aspects of platelet biology, as diagnostic and prognostic markers, and for therapeutic development efforts4,14. Several small platelet studies have characterized the transcriptome associated with platelet activity15,16,17. Most recently, platelet transcriptomic profiling has emerged as an innovative way to detect and track the prevalence and progression of certain malignancies14,18,19. Technological advancements have enhanced our understanding of the transcriptome and, coupled with bioinformatics, have fundamentally advanced transcriptomic-based tools to inform disease diagnosis and prognosis (e.g., cardiac allograft rejection20, detect respiratory viruses21, and diagnose cancer22). Developing a platelet hyperreactivity risk score is an innovative approach to identifying individuals with platelet hyperreactivity and, therefore, at significant CV risk.
Peripheral artery disease (PAD) affects ~8.5 million people over 40 years of age in the United States and 238 million globally23. Platelets mediate, in part, the pathogenesis of PAD, and platelet hyperreactivity is associated with PAD prevalence, severity, progression, and CV risk4,24,25. Despite medical and surgical therapy advances, PAD remains associated with significant morbidity and mortality26. The Platelet Activity and Cardiovascular Events in PAD (PACE-PAD) clinical study was designed to (1) prospectively investigate whether in symptomatic PAD patients requiring lower extremity revascularization (LER), platelet activity is associated with incident MACLE and (2) evaluate whether the platelet transcriptome identifies a platelet hyperreactivity signature predictive of incident CV events. Leveraging platelet activity and platelet transcriptomic measures from this well-phenotyped clinical cohort facilitated the development of a Platelet Reactivity ExpreSsion Score (PRESS), which discriminates individuals with a hyperreactive platelet phenotype. PRESS was associated with acute myocardial infarction and a higher risk for developing a future CV event. This study provides a informatics tool that discriminates platelet hyperreactivity, which can serve as a diagnostic tool to discriminate CV risk and potentially facilitate a personalized approach for CV risk reduction.
Results
A total of 300 patients scheduled for a LER procedure between March 2014 and November 2017 were enrolled. Of these, 13 individuals were subsequently excluded because a procedure was not performed (n = 7), another exclusion was noted (n = 4), or they died during index hospitalization from hemorrhagic complications (n = 2, Supplementary Fig. 1). Among the remaining 287 patients, open (n = 118, 41.1%), endovascular (n = 121, 42.2%), and hybrid (n = 28, 9.8%) procedures were performed. In a small subset of patients, a peripheral angiogram was performed without revascularization (n = 20, 6.9%). The mean age was 70 ± 11 years, 33% were female, and 61% were white. More than half of all patients (54%) had known coronary artery disease, 53% had diabetes mellitus, and 78% presented with CLI (Supplementary Table 1). Before surgery, the median (IQR) ankle-brachial index (ABI) was 0.54 (0.41, 0.72).
Thirty days post LER, 54 (18.8%) patients experienced a MACLE. Patients with a postoperative MACLE were more likely to present with CLI (90.7% vs. 75.5%, p = 0.024, Supplementary Table 1). Antiplatelet therapy, beta-blockers, statins, and ACE inhibitors/angiotensin receptor blockers were not significantly different between patients and those without post-procedural MACLE.
Platelet Hyperreactivity is associated with 30 day MACLE
Directly before LER, platelet aggregation was measured in 254 (88.5%) patients (Fig. 1A). The baseline characteristics of patients with and without assessment of platelet aggregation are described in Supplementary Table 2. Median platelet aggregation in response to 0.4 µM epinephrine was 32% (20, 49) and was significantly higher in patients with versus without MACLE (Fig. 1B). Platelet aggregation in response to epinephrine at multiple doses and time points was consistently higher in patients with MACLE (Supplementary Table 3). In addition, patients with MACLE had significantly higher platelet aggregation in response to other agonizts at submaximal doses (e.g., arachidonic acid, ADP, collagen, serotonin) than patients who did not go on to develop a major cardiac or limb event (Supplementary Table 3). These data demonstrate that platelet reactivity before LER is strongly associated with MACLE 30 days postoperatively.
A PACE-PAD Trial Design: Patients with peripheral artery disease (PAD) undergoing lower extremity revascularization (LER) were recruited into the PACE-PAD study (NCT02106429). Peripheral blood samples were collected immediately before the LER procedure, platelet aggregation was assessed via light transmission aggregometry (n = 254), and platelets were isolated for subsequent RNA-sequencing (n = 129). Patients were followed for 30 days following LER to assess post-operative CV events, with the primary endpoint a composite of major adverse cardiac or limb event (MACLE, defined by death, myocardial infarction (MI), stroke, major amputation, major or minor reintervention of the index limb). B Patients (n = 246) who experienced a MACLE within 30 days of LER had higher platelet aggregation responses to 0.4 µM epinephrine before the LER procedure. Bar represents median aggregation % ± IQR. % Aggregation was compared using a two-sided Mann-Whitney test. C Schematic of subject stratification by platelet reactivity status. D Bimodal distribution of platelet aggregation responses to 0.4 µM epinephrine of PACE-PAD patients. Hyperreactivity defined as >60% aggregation. E PACE-PAD patients whose platelet reactivity at baseline was >60% were significantly more likely to experience MACLE (n = 246). MACLE frequency were compared using chi-square tests. F Influence of platelet aggregation to MACLE incidence. Kaplan-Meier analysis of 30 day MACLE. Platelet aggregation responses above the median were associated with a 2.76-fold increase in MACLE (HR = 2.76, p = 0.001). Survival curves were compared using log-rank tests. Source data are provided as a Source Data file. Panel A and C created with BioRender.com released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license.
Platelet hyperreactivity and clinical presentation
In response to submaximal epinephrine, platelet aggregation induced a bimodal response where a small yet significant proportion of individuals demonstrated a hyperreactive platelet phenotype with >60% aggregation (Fig. 1C, D). Among patients with aggregation measured in response to 0.4 µM epinephrine, 17.5% displayed platelet hyperreactivity. Patients with a hyperreactive platelet phenotype did not differ by age, sex, or race/ethnicity but were more likely to have diabetes mellitus, present with gangrene, and less likely to receive antiplatelet therapy (Supplementary Table 4). Following multivariable adjustment, gangrene (aOR 2.50, 95% CI 1.12 – 5.54) was associated with higher odds of platelet hyperreactivity and antiplatelet therapy (aOR 0.15, 95% CI 0.06 – 0.39) with lower odds of platelet hyperreactivity. After excluding 31 (10.7%) patients not on antiplatelet therapy, gangrene was the only covariate associated with higher odds (aOR 2.98, 95% CI 1.40 – 6.34) of platelet hyperreactivity.
Platelet hyperreactivity and clinical events
Individuals with a hyperreactive platelet phenotype in response to 0.4 µM epinephrine had a higher incidence of 30 day MACLE (37.2% vs. 15.3% in those with aggregation ≤60%, p = 0.002; Fig. 1E, F). The frequency of events, including individual components of the composite MACLE endpoint, is shown in Table 1, stratified by those with and without a hyperreactive platelet phenotype in response to submaximal epinephrine. After multivariable adjustment for age, sex, race/ethnicity, body mass index, diabetes, carotid artery disease, prior stroke, and CLI, platelet hyperreactivity was associated with a nearly 3-fold increased risk of MACLE (adjusted HR [aHR] 2.76, 95% CI 1.5 – 5.1, p = 0.002, Fig. 2A, Table 1). After excluding 31 (10.7%) patients who were not on antiplatelet therapy at the time of blood collection, a hyperreactive platelet phenotype remained independently associated with MACLE (41.4% vs. 16.7%; HR 3.06, 95% CI 1.57 to 5.98, p = 0.001; Supplementary Fig. 2). Platelet hyperreactivity in response to a range of epinephrine concentrations was consistently associated with MACLE after multivariable adjustment (Supplementary Fig. 3; Supplementary Table 5).
A The adjusted hazard ratio for major adverse cardiac or limb events (MACLE, defined by death, myocardial infarction (MI), stroke, major amputation, major or minor reintervention of the index limb) at 30 days based on preprocedural platelet aggregation responses to 0.4 µM epinephrine. Multivariable adjustment for age, sex, race/ethnicity, body mass index, diabetes, carotid artery disease, prior stroke, and critical limb ischemia. n = 246. Hazard ratios and 95% CIs were computed by cox proportional hazard models. B Sub-group Analysis: Platelet hyperreactivity to 0.4 µM epinephrine and incidence of MACLE within 30 days post lower extremity revascularization. The adjusted hazard ratio for MACLE at 30 days based on preprocedural platelet aggregation responses to 0.4 µM epinephrine (n = 43 hyperreactive, n = 203 not hyperreactive). Error bars represent the 95% confidence intervals. BMI body mass index, CLI critical limb ischemia, CAD coronary artery disease, RCRI Revised Cardiac Risk Index. Source data are provided as a Source Data file.
Multivariable adjusted hazard ratios for 30 day MACLE associated with platelet hyperreactivity are shown in Fig. 2B, stratified by other baseline characteristics. The association between platelet hyperreactivity and MACLE was directionally consistent across age, sex, CV risk, and antiplatelet therapies.
A hyperreactive platelet phenotype discriminates patients at risk of 30 day MACLE beyond commonly used perioperative cardiac risk models (e.g., RCRI)27. The addition of platelet hyperreactivity to the RCRI model improved discrimination to predict the 30 day composite of MACLE (C-statistic for RCRI – 0.59, 95% CI 0.51 to 0.68; C-statistic for RCRI plus platelet hyperreactivity—0.64, 95% CI 0.55 to 0.72; p = 0.009). The addition of platelet hyperreactivity significantly improved both reclassification (NRI; 0.42, 95% CI 0.13 to 0.71; p = 0.005) and the discrimination as calculated by the IDI (p = 0.011).
Development of Platelet Reactivity ExpresSion Score (PRESS)
The platelet transcriptome is used to gain insight into platelet mechanisms14,28,29, disease onset and progression4,15,17,30, and is reproducible over time31. Within the PACE cohort, 129 patients had platelet RNA sequencing from samples collected before LER (Supplementary Fig. 1; Fig. 3A). Amongst these, 19 (22.6%) patients had a hyperreactive platelet response to epinephrine (0.4 µM, demographics Fig. 3B, Supplementary Table 6). Following adjustment for age, sex, and race/ethnicity, differential expression analyses utilizing two statistical thresholds (DESeq2 and Wilcoxon signed-rank test) found that 796 transcripts were differentially expressed (p < 0.05) in patients with a hyperreactive platelet phenotype. Gene set enrichment analysis (GSEA) revealed biological pathways linked to platelet activation enriched in subjects with hyperreactive platelets. In the basal state, pathways related to anchoring junctions, secretory granules, the cytoskeleton, ribosomes, and vesicle-mediated transport were enriched in platelets from hyperreactive subjects (Supplementary Fig. 4). Among these 796 differentially expressed transcripts, 451 were significantly correlated (p < 0.05) with percent aggregation to epinephrine (0.4 µM), with 174 transcripts positively and 277 transcripts negatively associated with platelet hyperreactivity (Fig. 3C, D, Supplementary Table 7). Using a combination of weighted expression values from these 451 genes, we generated a Platelet Reactivity ExpresSion Score (PRESS) for each participant. Following 10-fold cross-validation, PRESS discriminated patients from those without platelet hyperreactivity (AUC [cross-validation] 0.81, 95% CI 0.68 to 0.94).
A, B To generate a platelet hyperreactivity gene signature, platelets were collected from PACE-PAD patients before lower extremity revascularization (LER, n = 129). Platelet RNA-seq and stratification of patients by hyperreactive platelet responses (aggregation responses > 60% versus = 40% to 0.4 µM epinephrine, n = 84). Violin plots showing platelet aggregation distribution, median represented by the bold dashed line and IQR by dashed lines. P < 0.001 as determined by a 2-sided Mann-Whitney U-test. C, D Overlap of transcripts differentially expressed (using both DESeq2 Wald test and the Wilcoxon rank-sum test after adjustment for age, sex, and race/ethnicity) between patients with hyperreactive or not hyperreactive platelets (n = 796), and transcripts significantly correlated with platelet aggregation responses to 0.4 µM epinephrine (n = 2035). Overlapping genes, n = 451 (PRESS gene set), 174 transcripts positively and 277 transcripts negatively associated with platelet hyperreactivity. E Boxplot showing the platelet hyperreactivity signature score in 10-fold cross-validation training comparing hyperreactive platelet and not hyperreactive platelet patient groups. The line across the box indicates the median, with the whiskers extending to ±1.5 × IQR following z-score normalization. Each outlier outside the whiskers are represented by individual marks. n = 84. F Receiver operating characteristic (ROC) curve of the mean 10-fold cross-validation training of the hyperreactive platelet signature, the shaded areas represent 95% CIs plotted for sensitivity at given in-sample specificities. Source data are provided as a Source Data file. Panel A created with BioRender.com released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license.
PRESS validation
To further evaluate the ability of PRESS to discriminate individuals with hyperreactive platelets, performance was assessed in an independent validation cohort, “Duke Cohort” (n = 35, free of CVD and off antiplatelet therapy, of which 14 (40%) had a hyperreactive [>60% aggregation] platelet phenotype (Fig. 4A, B; Supplementary Fig. 1)32. Within the Duke cohort, PRESS was significantly higher in those with versus without platelet hyperreactivity (p = 0.0095, Fig. 4C). The diagnostic performance of PRESS in the Duke Cohort performed well with an AUC of 0.77 (95% CI 0.75 to 0.79, Fig. 4D). The accuracy was 80%, sensitivity 71%, and specificity 86% when discriminating between those with and without platelet hyperreactivity (Fig. 4E). Furthermore, GSEA pathway analysis, incorporating PRESS in the Duke cohort, revealed significant enrichment of both upregulated (p = 0.006) and downregulated (p < 1.0 × 10−10) PRESS genes in subjects with hyperreactive platelets (Fig. 4F). Collectively, these data demonstrate the utility of PRESS in discriminating platelet hyperreactivity across populations.
A, B The PRESS signature was validated in an independent cohort (Duke cohort) of healthy participants with platelet aggregation measured at two separate time points and platelet RNAseq performed (n = s35). In this cohort, 14 participants had a hyperreactive platelet phenotype (aggregation >60% in response to epinephrine 0.5 µM). Violin plots showing platelet aggregation distribution, median represented by the bold dashed line and IQR by dashed lines. P < 0.001 as determined by a 2-sided Mann-Whitney U-test C Boxplot showing the performance of the extra-trees classifier ensemble model was trained on the PRESS gene set within the PACE cohort and externally validated on the Duke cohort. The line across the box indicates the median, with the whiskers extending to ± 1.5 × IQR following z-score normalization. Each outlier outside the whiskers are represented by individual marks. P = 0.0095 as determined by a 2-sided Student’s t-test. n = 35 (D) Receiver operating characteristic (ROC) curve of the extra-trees classifier ensemble model validated in the “Duke cohort” of healthy participants. The shaded areas represent 95% of CIs plotted for sensitivity at given in-sample specificities. E Performance of PRESS gene set in the Duke validation cohort (n = 35). F GSEA pathway analysis, incorporating the PRESS gene set of the Duke cohort, revealed significant enrichment of upregulated and downregulated PRESS in subjects with hyperreactive platelets. Source data are provided as a Source Data file. Panel A created with BioRender.com released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license.
PRESS gene set is enriched in cohorts with platelet hyperreactivity
Next, we reasoned that PRESS could discriminate populations with well-described hyperreactive platelets and a prothrombotic phenotype that underlies CV risk14. To test this, we investigated PRESS in multiple platelet RNA-seq cohorts from patients with previously described platelet hyperreactivity (Supplementary Fig. 1)32,33,34. First, we compared the platelet transcriptome of patients with established lower extremity atherosclerosis to a high-risk primary prevention cohort4,35. Incorporating PRESS into the analytical pipeline, PRESS was enriched in the platelet transcriptome of patients with versus without atherosclerosis (PRESS Up and Down, p = 0.0007, and p < 1 × 10−10, respectively, Fig. 5A, Supplementary Table 8). Furthermore, PRESS was significantly enriched in the platelet transcriptome of subjects with both COVID-19 and SLE (Fig. 5, Supplementary Table 8). Finally, PRESS was enriched in the transcriptome of reticulated (immature) platelets, a hyperreactive and prothrombotic platelet subtype, relative to non-reticulated (mature) platelets (Fig. 5A, Supplementary Table 8)36. Collectively, our data demonstrate that PRESS, in lieu of platelet function testing, can discriminate platelet hyperreactivity across disease states.
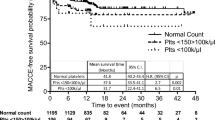
A GSEA pathway analysis, incorporating PRESS into multiple clinical cohorts or platelet subtypes; atherosclerosis, systemic lupus erythematosus, COVID-19, and reticulated platelets with platelet RNA-seq revealed significant enrichment of both upregulated and downregulated PRESS. Refer to Supplemental Fig. 1 for population descriptions. B Platelet aggregation to 0.4 μM epinephrine stratification based on each individuals PRESS (n = 129) in the PACE-PAD cohort. Violin plots showing platelet aggregation distribution, median represented by the bold dashed line and IQR by dashed lines. C Subjects with a PRESS greater than the median have increased platelet aggregation responses to epinephrine at multiple doses (0.1 μM, 0.4 μM, and 2 μM) and time points. D PRESS was calculated in a cohort of patients referred for coronary angiography with myocardial infarction (MI) (n = 19) relative to patients referred for cardiac catheterization with coronary artery disease without MI (n = 9). The line across the box indicates the median, with the whiskers extending to ± 1.5 × IQR following z-score normalization. Minimum and maximum data values are used as end points for the whiskers.p = 0.0084, as assessed by 2-sided Student’s t-test. E Kaplan-Meier cumulative incidence plot of major adverse cardiac events (death, myocardial infarction, stroke or major amputation) in a cohort of patients with peripheral artery disease followed for a median of 18 months. After adjustment for age, sex, race/ethnicity, BMI, diabetes, carotid artery disease, prior stroke, and CLI, a PRESS above the median was associated with a 90% increase in a major cardiovascular event (50.7% vs. 31.9% below the median, adjusted HR 1.90, CI 1.07 –3.36, p = 0.027). Source data are provided as a Source Data file.
PRESS is associated with cardiovascular risk
PRESS successfully stratified individuals based on their platelet aggregation response to submaximal agonist stimulation with epinephrine (Fig. 5B), across epinephrine concentrations (Fig. 5C), and across multiple agonizts (Supplementary Table 9). To determine the prognostic value of PRESS, we explored the association between PRESS and CV risk in two populations of CV disease. In the Heart Attack Research Program (HARP), PRESS was calculated in women undergoing coronary angiography. PRESS was significantly increased in women with acute MI compared to women referred for coronary angiography with obstructive coronary artery disease without MI (p = 0.0084, Fig. 5D, Supplementary Table 10). After multivariable adjustment for age, race/ethnicity, diabetes, and hypertension, PRESS was significantly associated with acute MI (β = 1.8, 95% CI 0.2 – 3.3, p = 0.02). In the second cohort of patients with lower extremity PAD undergoing LER, PRESS was calculated from 129 platelet RNA samples collected prior to LER (Supplementary Table 11). After a median follow-up of 18 months, the cumulative incidence of major adverse CV events differed by PRESS. After adjusting for age, sex, race/ethnicity, BMI, diabetes, carotid artery disease, prior stroke, and CLI, a PRESS above the median value was associated with a 90% increase in a major CV event (50.7% vs. 31.9% below the median, adjusted HR 1.90, CI 1.07 – 3.36), p = 0.027, Fig. 5E). When PRESS was stratified into tertiles, those with a score in the highest tertile were at the highest risk of a major CV event (54.3% vs 28.3% in the lowest tertile, adjusted HR 2.39, CI 1.15 – 4.98, p = 0.02, Supplemental Fig. 5). Altogether, these data demonstrate that PRESS can discriminate those at increased CV risk.
Discussion
Patients with symptomatic PAD undergoing LER are at high risk for cardiac and limb events, many of which are platelet-mediated. Our data demonstrate that the platelet phenotype prior to LER is associated with incident cardiac and limb events within the first 30 days post-revascularization. The association between platelet hyperreactivity and 30-day events was independent of demographics, clinical characteristics, perioperative risk, and antiplatelet therapy. Notably, incorporating platelet aggregation into traditional perioperative CV risk models improved both reclassification and risk discrimination.
Clinically, platelet aggregometry is used to assess those with suspected platelet function disorders; however, this technique is labor and time-intensive and requires careful quality control and technical expertize in its performance and interpretation. Thus, in conjunction with platelet aggregation measures, we developed and validated a platelet transcriptomic signature that can identify patients with a hyperreactive platelet phenotype. This transcriptional signature could discriminate hyperreactive platelet profiles and identify individuals at elevated CV risk. Collectively our study highlights the clinical relevance of platelet hyperreactivity, both at the functional and transcriptomic level.
Platelets are major players in the pathogenesis of atherogenesis and thrombosis1. In addition to their well-described effects on CV disease, platelets are increasingly recognized for their role in inflammation and immunity37,38. Increased platelet activity has been observed across multiple disease states (e.g., CV, rheumatological and infectious)1,3,5,39,40. Platelet aggregation has previously been proposed as a valuable biomarker of CV risk41. Spontaneous platelet aggregation measured 3 months following an MI off antiplatelet therapy was associated with CV morbidity and all-cause mortality3. Subsequent studies noted conflicting and inconsistent results41. Data from the Framingham study found that in those free of CV disease and without antiplatelet therapy, hyperreactivity to ADP, although not epinephrine, was modestly associated with the risk of MI or stroke during a 20 year follow-up8. In the current study, we extend prior observations to the perioperative period and demonstrate that platelet hyperreactivity measured before LER is associated with 30 day MACLE. Our findings are directionally consistent in multiple subgroups, including by age, sex, race/ethnicity, antiplatelet therapy, and CV risk. In fact, platelet hyperreactivity provided additional predictive value beyond traditional assessments of perioperative risk.
Although our data suggest a significant association between platelet hyperreactivity and subsequent CV events, routine clinical measurement of platelet aggregation is widely considered infeasible. Variability, poor site standardization, cost, time of processing, and pre- and post-analytical measures (e.g., needle gauge, blood sampling and handling, specimen transport and processing) limit enthusiasm for routinely measuring platelet aggregation42. Investigation of the platelet transcriptome however increases accessibility and allows unbiased insight into mechanisms and pathways associated with platelet hyperreactivity. Transcriptome analyses of platelets are increasingly used for discoveries related to platelet biology, as diagnostic and prognostic markers, and for potential therapeutic development14,18,19.
Our platelet transcriptomic signature is able to differentiate individuals with platelet hyperreactivity. While PRESS was developed in patients with symptomatic PAD on antiplatelet therapy, discriminating platelet hyperreactivity in patients on and off antiplatelet therapy is clinically appealing and removes a major barrier to platelet function testing. Thus, our validation of the signature in an external cohort of healthy subjects who were not taking any antiplatelet therapy points to the robustness and utility of our signature. In fact, the PRESS gene set contains several transcripts linked to platelet activation responses (e.g. P2RX143, RHOA44, WDR115, CD69)45, and is characterized by pathways associated with platelet activation (anchoring junctions, organelle organization, cytoskeleton reorganization, and vesicle-mediated transport). Altogether, these data demonstrate that individuals with hyperreactive platelets have a unique transcriptome reflective of a primed activation state.
Since PRESS successfully discriminated platelet hyperreactivity on and off antiplatelet therapy, we investigated if this signature was enriched in platelets of patients with diseases known to have a hyperreactive platelet phenotype. Consistently, PRESS was among the top candidate pathways enriched in patients with well-documented platelet hyperreactivity, including lower extremity atherosclerosis, COVID-19, and SLE. Additionally, as further validation, we incorporated PRESS into GSEA analyses of platelet RNA-seq of reticulated versus non-reticulated platelets. Since reticulated platelets are larger, younger, and immature platelets with increased activity and greater prothrombotic potential, PRESS was found to be amongst the most enriched pathways in this platelet population.
Our study has identified various areas for future research. While PRESS was developed in patients with symptomatic PAD and validated in a healthy control cohort, future validation of this signature in a significantly larger primary prevention population (e.g., those at risk for a first cardiovascular event) is important to assess the robustness and applicability of the signature. Identifying individuals with a hyperreactive platelet phenotype at risk for a CV event may benefit from primary prevention with antiplatelet therapy and should be investigated. Once individuals with a hyperreactive platelet phenotype are identified, future studies randomizing these high-risk cohorts based on their platelet phenotype could identify a group that benefits from antiplatelet therapy29,46. Investigation of platelet hyperreactivity could also identify individuals at differential risk for bleeding and thus support the modification of antithrombotic therapies to attenuate bleeding. Additional studies are needed to explore the impact of platelet-directed pharmacotherapies on these genes. Our future work will address these research questions and adapt our gene signature for translation to diagnoses, prognostication, and precision-guided care with antiplatelet therapies.
Several limitations should be considered when interpreting the results of this study. First, the population that derived the platelet hyperreactivity signature had symptomatic PAD on antiplatelet therapy. Thus, applicability to other cohorts with CVD to assess its clinical utility is needed. Nonetheless, we validated the PRESS gene signature in subjects without clinical CV disease, highlighting our signature’s ability to discriminate platelet hyperreactivity in subjects with and without CV disease and on- and off-platelet therapy. Additionally, future validation in larger cohorts is necessary to assess the robustness and clinical applicability of the signature. In the subgroup of patients used for the PRESS derivation cohort (n = 84), participants with platelet hyperreactivity trended towards more frequent cardiovascular events. However, in this smaller cohort statistical significance was not reached (Supplementary Table 12 and 13). Second, while submaximal epinephrine was used to define platelet hyperreactivity, our data are consistent across various agonizts and concentrations (Supplementary Table 9). Additionally, submaximal epinephrine was chosen as we and others have shown a distinct bimodal platelet aggregation response reproducible over time and generalizable to other forms of platelet activation9,10,47. Third, platelet activity was measured at the time of LER in our patient population, a procedure that is performed throughout the day. Thus platelet activity measures may be affected by circadian variation. Finally, while platelet hyperreactivity was associated with 30 day CV and limb events, future work is needed to extend these findings to longer follow-ups.
In individuals with symptomatic PAD undergoing LER, platelet aggregation in response to submaximal epinephrine is associated with 30 day MACLE. A platelet transcriptional signature, PRESS, can discriminate individuals with a hyperreactive platelet phenotype and identify those at increased risk for CV events. Future studies can leverage this platelet hyperreactivity score to investigate platelet-mediated diseases and personalized diagnostics to improve CV risk reduction.
Methods
Study cohort
This study was authorized by the New York University Langone Health and VA New York Harbor Healthcare System Institutional Review Boards and the Office of Research Administration at Bellevue Hospital. All participants provided written informed consent. Male and female patients (n = 300) > 21 years of age with PAD undergoing non-emergent LER were recruited into the PACE-PAD study (NCT02106429) from New York University Langone Health: Manhattan Campus, Bellevue Hospital, or the Veterans Affairs New York Harbor Healthcare System. Individuals were excluded if they used NSAIDs in the past 72 h, had a platelet count <100 × 109/L or >500 × 109/L, hemoglobin <8 mg/dl, or any known hemorrhagic diathesis.
Monitoring of post-procedure cardiovascular events
Patients were followed for 30 days following LER to assess post-operative CV events4,35. Surveillance electrocardiograms (ECG) and cardiac troponin I concentrations were measured on post-procedural day 2. Blood collections and ECGs performed as part of routine care were used to ascertain event occurrence after postoperative day 2. After hospital discharge, patients were contacted by telephone (or during their routine clinical follow-up) to identify additional events, quality of life, and medication use. The primary endpoint was a composite of major adverse cardiac or limb events (MACLE), defined by major adverse cardiovascular events (MACE; death, myocardial infarction (MI), stroke) and major adverse limb events (MALE; major amputation, or major [new bypass graft, jump/interposition graft revisions or thrombectomy/thrombolysis] or minor [balloon angioplasty, atherectomy, laser treatment and/or stenting or stent/grafting] reintervention of the index limb) at 30 days.
Two cardiologists and one vascular surgeon blinded to the platelet aggregation results adjudicated all events by review of medical records. Additional details regarding endpoints are provided in the Supplemental Methods.
Blood collection
Before LER, peripheral blood samples were collected from fasting patients at the onset of the procedure. After an initial 2 cc discard, whole blood was collected into tubes containing 3.2% sodium citrate (BD Vacutainer, cat # 369714) for platelet activity measures and collection of platelets for subsequent RNA isolation. Blood specimens were immediately processed, and citrate-anticoagulated blood was centrifuged (within 30 minutes of collection) at 200 g for 10 min to obtain platelet-rich plasma48.
Platelet aggregation
Light Transmission Aggregometry (LTA) measures the kinetics of platelet aggregation in a glycoprotein IIb/IIIa-dependent manner and is the most widely used measurement of platelet function49,50. Platelet aggregometry was conducted on a Helena (Beaumont, TX) AggRAM light transmission aggregometer based on the method of Born51. Platelet aggregation was measured in response to submaximal agonist stimulation. Agonizts included epinephrine (2, 0.4, 0.1 µM, Helena Laboratories, cat # 5367), adenosine diphosphate (ADP; 2, 1, 0.4 µM, Helena Laboratories, cat # 5366), collagen (1, 0.2 µg/ml, Helena Laboratories, cat # 5368), serotonin (10 µM, Sigma Aldrich, cat # H9523), epinephrine and serotonin (1 and 10 µM respectively) and arachidonic acid (AA; 1.6 mM, Helena Laboratories, cat # 5364) incubated with and without aspirin in vitro (3 mM, Santa Cruz Biotechnology, cat # sc-202471). Platelet hyperreactivity was defined by platelet aggregation >60% in response to submaximal epinephrine 0.4 µM10.
Platelet transcriptome
Blood was collected for platelet RNA sequencing at the same time as measures of platelet aggregation. Briefly, platelets were isolated and purified by incubation with microbeads to deplete leukocytes and red blood cells (EasySep™ Human CD45 Depletion Kit, StemCell Technologies, cat # 17898 and EasySep™ RBC Depletion Reagent, StemCell Technologies, cat # 18170). Isolated platelets lysed in 500 uL of QIAzol Lysis Reagent (Qiagen, cat # 79306) and stored at −80 oC. RNA was isolated with Direct-zol RNA microspin columns (Zymo Research, cat # R2062), and quality and quantity were determined with a Bioanalyzer 2100 (Agilent Technologies). RNA quality and quantity were determined with a Bioanalyzer 2100 (Agilent Technologies). Sequencing libraries were barcoded and prepared using the Clontech SMART-Seq HT with Nxt HT kit (Takara Bio USA, cat # 634437), and libraries were sequenced single end on an Illumina NovaSeq 600015,32,39,52. Samples were analyzed using the Seq-N-Slide pipeline53. Reads were aligned to the hg38 genome using STAR54 v2.6.1 and quantified using featureCounts55 v1.6.3. Read quality was assessed using FASTQC56 v0.11.7.
Development and application of the Platelet Reactivity Expression Score (PRESS)
The platelet transcriptome was compared between patients with a hyperreactive phenotype (>60% aggregation in response to submaximal epinephrine, 0.4 µM) relative to those with a platelet aggregation response <40% in response to submaximal epinephrine (0.4 µM)10. To develop PRESS, we identified genes differentially expressed between groups using the DESeq2 Wald test57 and the more conservative Wilcoxon rank-sum test after adjustment for age, sex, and race/ethnicity. Only transcripts significantly different (p < 0.05) in both tests were retained for downstream analysis. A nominal p-value cutoff of 0.05 was used as very few genes reached significance after the correction of Benjamini-Hochberg multiple testing. To increase confidence in our final gene set, we identified transcripts significantly correlated with the percent of platelet aggregation in response to submaximal agonist stimulation with epinephrine 0.4 µM as a continuous variable. The intersect of genes identified as significantly differential using both the DESeq2 Wald test, and the Wilcoxon rank-sum and significantly correlated with platelet aggregation were then used to generate the Platelet Reactivity Expression Score (PRESS).
To assign PRESS at a sample level, we built a soft voting ensemble model of random forests, extra-trees forests, adaboost forests, and gradient boosted forests (n = 28 each). Internal classifiers of the soft voting ensemble model were tuned to optimize area under the receiver operating curve (AUC) using GridSearchCV. Each model was trained on the scaled and normalized transcript expression of PRESS genes. To assess model training performance, the mean and 95% confidence interval (CI) of the AUC was calculated with 10-fold cross-validation. After cross-validation, the model was refit on all samples for downstream testing and validation in external datasets. The model was used to generate a PRESS score for each individual, presented as a z-scored predictive probability, which was used to represent sample-specific platelet reactivity.
Platelet aggregation validation cohort
Our PRESS model was validated in an external cohort of healthy participants from Duke University who enrolled in a clinical study examining the effect of antiplatelet therapy on platelet activity and the platelet transcriptome58. We used data from patients without antiplatelet therapy for >4 weeks before blood collection. Platelet LTA was measured in response to submaximal epinephrine 0.5 µM, and platelet RNA was isolated and sequenced58. Consistent with our derivation cohort in patients with PAD, PRESS was compared between patients with a hyperreactive platelet phenotype (>60% aggregation) and those with aggregation <40% in response to submaximal epinephrine stimulation. Performance of the PRESS model was validated within the Duke Cohort with 1000-fold bootstrapping to determine AUC and 95% confidence intervals for external model performance.
Platelet hyperreactivity PRESS gene set
The PRESS gene set was divided into upregulated (PRESS-up) and downregulated (PRESS-down) genes. To reduce potential bias in our validation of PRESS by GSEA, we reduced the gene set only to include genes that are part of the GO term universe of genes (164/174 for PRESS-up; 257/277 for PRESS-down). Pre-ranked gene set enrichment analysis (GSEA) was performed using the log2 fold change (log2fc) values as a ranking method59,60. All GSEA were performed using ClusterProfiler61.
Clinical validation cohorts (Supplemental Fig. 1): Platelet RNA collected and sequenced were used for validation of the PRESS in multiple cohorts: (1) Patients with lower extremity atherosclerosis (n = 129) versus a high-risk primary prevention cohort (n = 28, multiple CV risk factors without clinical atherosclerosis)35,39; (2) systemic lupus erythematosus (SLE, n = 51) versus controls (n = 18), (3) COVID-19 (n = 8) versus controls (n = 10)34; (4) previously published transcriptome analysis of reticulated (immature) versus non-reticulated (mature) platelets36; and (5) subjects recruited into the Women’s Heart Attack Research Program (HARP, NCT03022552) who presented with acute MI (n = 19) and obstructive coronary artery disease (n = 9) confirmed by coronary angiography. Following adjustment for age, sex, and race/ethnicity, PRESS was compared between groups. For all studies, with the exception of HARP, both men and women were included. HARP only contains women. Sex was determined by self-report during study admission and consent.
Statistical analysis
When comparing participant demographics and clinical variables between groups, we used 2-sample t-tests or Wilcoxon tests for continuous variables and χ2 tests or Fisher’s exact tests for categorical variables. Categorical variables are presented as numbers (percentage) and continuous variables as mean ± SD or median (interquartile range) as appropriate.
To investigate the association between platelet hyperreactivity and MACLE up to 30 days post-procedure, patients were divided into two groups based on aggregation responses to submaximal epinephrine (0.4 µM): hyperreactive (>60% aggregation) and not hyperreactive (≤60% aggregation)9,10,47. Cox proportional hazard regressions were used to assess the relationship between platelet hyperreactivity and 30 day MACLE. Models were adjusted for age, sex, race/ethnicity, and population-relevant clinical risk factors, including BMI, diabetes, carotid artery disease, prior stroke, and critical limb ischemia (CLI). In the HARP cohort, which includes only females, sex was not included in multivariable models. In PACE, CLI (the most severe form of PAD) and carotid artery disease were included in the multivariable model. These two variables were not available in the non-PAD cohorts
Survival curves were plotted using the Kaplan-Meier method, and differences between groups were determined using log-rank tests. Analyses were repeated after excluding patients who did not receive antiplatelet therapy at baseline blood collection. Subgroup analyses were performed stratified by age, sex, race/ethnicity, body mass index, diabetes mellitus, coronary artery disease, medical therapy, and clinical presentation.
A Cox proportional hazard regression model was generated with the Revised Cardiac Risk Index (RCRI) as a covariate to predict MACLE at 30 days to assess whether platelet aggregation measures improve perioperative CV risk prediction27. Platelet hyperreactivity was subsequently added to the model. Harrell’s C-statistics and 95% CI were computed for model discrimination; a z-score test was constructed to compare the two C statistics62. We also assessed the net reclassification improvement (NRI; the probability that patients are reclassified to higher or lower risk) and integrated discrimination improvement (IDI; to quantify mean predicted probabilities of events and nonevents based on the addition of the new biomarkers to the model)63.
In the cohort of PACE-PAD with RNA sequencing data available, each participant was assigned a hyperreactivity score (PRESS) using the predicted probability of the ensemble model. During a median follow-up of 18 months, we investigated whether PRESS was associated with a composite of death, MI, stroke, and major amputation. Cumulative event rates were estimated using Kaplan-Meier curves stratified by groups and were compared using the log-rank test. Cox proportional hazards regression analyses were performed to investigate the association of PRESS with outcomes in both univariable and multivariable analyses adjusting for demographics and CV risk factors, including age, sex, race/ethnicity, BMI, diabetes, carotid artery disease, prior stroke, and critical limb ischemia.
Statistical analysis was performed with Rstudio, version 4.0.3. A 2-sided value of P < 0.05 was considered statistically significant. Machine learning training and validation were performed in Python, version 3.10.6.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available in the article, its Supplementary information, the Source data and from the corresponding author upon request. The platelet RNA-seq data generated in this study have been deposited in the GEO database under accession code GSE232027. Additional publicly available data is on the GEO database under the accession codes GSE226147, GSE126448 and GSE176480. Source data are provided with this paper.
Code availability
Code is available on https://github.com/ruggleslab/press (https://doi.org/10.5281/zenodo.12537341).
References
Davi, G. & Patrono, C. Platelet activation and atherothrombosis. N. Engl. J. Med. 357, 2482–2494 (2007).
Falk, E. Coronary thrombosis: pathogenesis and clinical manifestations. Am. J. Cardiol. 68, 28B–35B (1991).
Trip, M. D., Cats, V. M., van Capelle, F. J. & Vreeken, J. Platelet hyperreactivity and prognosis in survivors of myocardial infarction. N. Engl. J. Med. 322, 1549–1554 (1990).
Dann, R. et al. Platelet-derived MRP-14 induces monocyte activation in patients with symptomatic peripheral artery disease. J. Am. Coll. Cardiol. 71, 53–65 (2018).
Rajagopalan, S. et al. Platelet activation increases with the severity of peripheral arterial disease: implications for clinical management. J. Vasc. Surg. 46, 485–490 (2007).
Gurbel, P. A., Becker, R. C., Mann, K. G., Steinhubl, S. R. & Michelson, A. D. Platelet function monitoring in patients with coronary artery disease. J. Am. Coll. Cardiol. 50, 1822–1834 (2007).
Michelson, A. D. Methods for the measurement of platelet function. Am. J. Cardiol. 103, 20A–26A (2009).
Puurunen, M. K. et al. ADP platelet hyperreactivity predicts cardiovascular disease in the FHS (Framingham Heart Study). J. Am. Heart Assoc. 7, e008522 (2018).
Berger, J. S. et al. Hyperreactive platelet phenotypes: relationship to altered serotonin transporter number, transport kinetics and itrinsic response to adrenergic co-stimulation. Thromb. Haemost. 109, 85–92 (2012).
Yee, D. L., Sun, C. W., Bergeron, A. L., Dong, J. F. & Bray, P. F. Aggregometry detects platelet hyperreactivity in healthy individuals. Blood 106, 2723–2729 (2005).
Breddin, H. K. et al. Spontaneous platelet aggregation as a predictive risk factor for vascular occlusions in healthy volunteers? results of the HAPARG study. Haemostatic parameters as risk factors in healthy volunteers. Atherosclerosis 144, 211–219 (1999).
Elwood, P. C., Renaud, S., Beswick, A. D., O’Brien, J. R. & Sweetnam, P. M. Platelet aggregation and incident ischaemic heart disease in the Caerphilly cohort. Heart 80, 578–582 (1998).
Cattaneo, M. et al. Results of a worldwide survey on the assessment of platelet function by light transmission aggregometry: a report from the platelet physiology subcommittee of the SSC of the ISTH. J. Thromb. Haemost. 7, 1029 (2009).
Davizon-Castillo, P., Rowley, J. W. & Rondina, M. T. Megakaryocyte and platelet transcriptomics for discoveries in human health and disease. Arterioscler Thromb. Vasc. Biol. 40, 1432–1440 (2020).
Montenont, E. et al. Platelet WDR1 suppresses platelet activity and is associated with cardiovascular disease. Blood 128, 2033–2042 (2016).
Edelstein, L. C. et al. Racial differences in human platelet PAR4 reactivity reflect expression of PCTP and miR-376c. Nat. Med. 19, 1609–1616 (2013).
Eicher, J. D. et al. Characterization of the platelet transcriptome by RNA sequencing in patients with acute myocardial infarction. Platelets 27, 230–239 (2016).
In ‘t Veld, S. et al. Detection and localization of early- and late-stage cancers using platelet RNA. Cancer Cell 40, 999–1009.e1006 (2022).
Best, M. G., In ‘t Veld, S., Sol, N. & Wurdinger, T. RNA sequencing and swarm intelligence-enhanced classification algorithm development for blood-based disease diagnostics using spliced blood platelet RNA. Nat. Protoc. 14, 1206–1234 (2019).
Fujita, B. et al. Predictive value of gene expression profiling for long-term survival after heart transplantation. Transpl. Immunol. 41, 27–31 (2017).
Creager, H. M. et al. Clinical evaluation of the BioFire(R) respiratory panel 2.1 and detection of SARS-CoV-2. J. Clin. Virol. 129, 104538 (2020).
Yu, W. et al. Exosome-based liquid biopsies in cancer: opportunities and challenges. Ann. Oncol. 32, 466–477 (2021).
Criqui, M. H. et al. Lower extremity peripheral artery disease: contemporary epidemiology, management gaps, and future directions: a scientific satement from the American heart association. Circulation 144, e171–e191 (2021).
Cassar, K., Bachoo, P., Ford, I., Greaves, M. & Brittenden, J. Platelet activation is increased in peripheral arterial disease. J. Vasc. Surg. 38, 99–103 (2003).
Allen, N. et al. Circulating monocyte-platelet aggregates are a robust marker of platelet activity in cardiovascular disease. Atherosclerosis 282, 11–18 (2019).
Golomb, B. A., Dang, T. T. & Criqui, M. H. Peripheral arterial disease: morbidity and mortality implications. Circulation 114, 688–699 (2006).
Lee, T. H. et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100, 1043–1049 (1999).
Schubert, S., Weyrich, A. S. & Rowley, J. W. A tour through the transcriptional landscape of platelets. Blood 124, 493–502 (2014).
Cofer, L. B., Barrett, T. J. & Berger, J. S. Aspirin for the primary prevention of cardiovascular disease: time for a platelet-guided approach. Arterioscler Thromb. Vasc. Biol. 42, 1207–1216 (2022).
Healy, A. M. et al. Platelet expression profiling and clinical validation of myeloid-related protein-14 as a novel determinant of cardiovascular events. Circulation 113, 2278–2284 (2006).
Rondina, M. T. et al. Longitudinal RNA-Seq analysis of the repeatability of gene expression and splicing in human platelets identifies a platelet SELP splice QTL. Circ. Res. 126, 501–516 (2020).
Barrett, T. J. et al. Platelets amplify endotheliopathy in COVID-19. Sci. Adv. 7, eabh2434 (2021).
Manne, B. K. et al. Platelet gene expression and function in patients with COVID-19. Blood 136, 1317–1329 (2020).
El Bannoudi, H. et al. Platelet LGALS3BP induces myeloid inflammation in systemic lupus erythematosus. Arthritis Rheumatol. 75, 711–722 (2022).
Newman, J. D. et al. Gene expression signature in patients with symptomatic peripheral artery disease. Arterioscler Thromb. Vasc. Biol. 41, 1521–1533 (2021).
Bongiovanni, D. et al. Transcriptome analysis of reticulated platelets reveals a prothrombotic profile. Thromb. Haemost. 119, 1795–1806 (2019).
Gawaz, M., Langer, H. & May, A. E. Platelets in inflammation and atherogenesis. J. Clin. Invest.h 115, 3378–3384 (2005).
Koupenova, M., Clancy, L., Corkrey, H. A. & Freedman, J. E. Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ. Res. 122, 337–351 (2018).
Barrett, T. J. et al. Platelets contribute to disease severity in COVID-19. J. Thromb. Haemost. 19, 3139–3153 (2021).
Steinhubl, S. R. & Moliterno, D. J. The role of the platelet in the pathogenesis of atherothrombosis. Am. J. Cardiovasc. Drugs 5, 399–408 (2005).
Sharma, G. & Berger, J. S. Platelet activity and cardiovascular risk in apparently healthy individuals: a review of the data. J. Thromb. Thrombolysis 32, 201–208 (2011).
Gorog, D. A. & Fuster, V. Platelet function tests in clinical cardiology: unfulfilled expectations. J. Am. Coll. Cardiol. 61, 2115–2129 (2013).
Mahaut-Smith, M. P., Tolhurst, G. & Evans, R. J. Emerging roles for P2X1 receptors in platelet activation. Platelets 15, 131–144 (2004).
Aslan, J. E. & McCarty, O. J. Rho GTPases in platelet function. J. Thromb. Haemost. 11, 35–46 (2013).
Testi, R., Pulcinelli, F., Frati, L., Gazzaniga, P. P. & Santoni, A. CD69 is expressed on platelets and mediates platelet activation and aggregation. J. Exp. Med. 172, 701–707 (1990).
Berger, J. S. Aspirin for primary prevention-time to rethink our approach. JAMA Netw. Open 5, e2210144 (2022).
Yee, D. L., Bergeron, A. L., Sun, C. W., Dong, J. F. & Bray, P. F. Platelet hyperreactivity generalizes to multiple forms of stimulation. J. Thromb. Haemost. 4, 2043–2050 (2006).
Merolla, M., Nardi, M. A. & Berger, J. S. Centrifugation speed affects light transmission aggregometry. Int J. Lab Hematol. 34, 81–85 (2012).
Refaai, M. & Laposta, M. Platelet aggregaton. In: Michelson AD (ed. Platelets, S. D.) 291–296 (CA: Academic Press, 2002).
Breddin, H. K. Can platelet aggregometry be standardized? Platelets 16, 151–158 (2005).
Born, G. V. Aggregation of blood platelets by adenosine diphosphate and its reversal. Nature 194, 927–929 (1962).
Marcantoni, E. et al. Platelet transcriptome profiling in HIV and ATP-binding cassette subfamily C member 4 (ABCC4) as a mediator of platelet activity. JACC Basic Transl. Sci. 3, 9–22 (2018).
igordot/sns (2020).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Liao, Y., Smyth, G. K. & Shi, W. featureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014).
Andrews, S. Babraham Bioinformatics - FastQC A Quality Control tool for High Throughput Sequence Data. https://www.bioinformatics.babraham.ac.uk/projects/fastqc/ (2023).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Myers, R. A. et al. Aspirin effects on platelet gene expression are associated with a paradoxical, increase in platelet function. Br. J. Clin. Pharm. 88, 2074–2083 (2022).
Liberzon, A. et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics 27, 1739–1740 (2011).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Yu, G., Wang, L. G., Han, Y. & He, Q. Y. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS 16, 284–287 (2012).
Kang, L., Chen, W., Petrick, N. A. & Gallas, B. D. Comparing two correlated C indices with right-censored survival outcome: a one-shot nonparametric approach. Stat. Med. 34, 685–703 (2015).
Pencina, M. J., D’Agostino, R. B. Sr, D’Agostino, R. B. Jr & Vasan, R. S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat. Med. 27, 157–172 (2008).
Acknowledgements
Support for this study was provided by the National Institutes of Health (R01HL114978 and R35HL144993 to J.S.B., R01HL167917 to T.J.B., 5R01HL118049 to D.V., K23HL150315 to N.S.). The NYU CTSA grant UL1TR001445 from the National Center for Advancing Translational Sciences (NCATS) partly supported the study. NYU Langone Health DART Genomic Technology Core is partially funded by NYU Cancer Center Support Grant NIH/NCI P30CA016087.
Author information
Authors and Affiliations
Contributions
J.S.B. had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: J.S.B., T.J.B. Acquisition, analysis, or interpretation of data: J.S.B., T.J.B., M.C., D.V., Y.X., M.M., F.S. Drafting of the manuscript: J.S.B, T.J.B. Critical revision of the manuscript for important intellectual content: K.R., J.N., J.H., C.R., N.S., Y.X., D.V. Statistical analysis: M.C., Y.X., M.M. Obtained funding: J.S.B.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Udaya Tantry, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Berger, J.S., Cornwell, M.G., Xia, Y. et al. A Platelet Reactivity ExpreSsion Score derived from patients with peripheral artery disease predicts cardiovascular risk. Nat Commun 15, 6902 (2024). https://doi.org/10.1038/s41467-024-50994-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-024-50994-7