Abstract
Skull-base chordoma is a rare, aggressive bone cancer with a high recurrence rate. Despite advances in genomic studies, its molecular characteristics and effective therapies remain unknown. Here, we conduct integrative genomics, transcriptomics, proteomics, and phosphoproteomics analyses of 187 skull-base chordoma tumors. In our study, chromosome instability is identified as a prognostic predictor and potential therapeutic target. Multi-omics data reveals downstream effects of chromosome instability, with RPRD1B as a putative target for radiotherapy-resistant patients. Chromosome 1q gain, associated with chromosome instability and upregulated mitochondrial functions, lead to poorer clinical outcomes. Immune subtyping identify an immune cold subtype linked to chromosome 9p/10q loss and immune evasion. Proteomics-based classification reveals subtypes (P-II and P-III) with high chromosome instability and immune cold features, with P-II tumors showing increased invasiveness. These findings, confirmed in 17 paired samples, provide insights into the biology and treatment of skull-base chordoma.
Similar content being viewed by others
Introduction
Chordomas are rare, slow-growing, locally aggressive malignant bone tumors that are thought to arise from embryonic notochordal remnants and mainly reside throughout the axial skeleton, such as the skull-base, mobile spine and sacrum1. Chordomas account for 1% to 4% of all bone malignancies. The incidence of chordoma is 0.08 per 100,000 people each year, with skull-base location accounting for one case per two million people each year2. The pathogenesis of chordomas remains unclear.
Although chordomas are considered slow-growing, low-grade neoplasms, they are highly recurrent with a 5 year local recurrence rate of 53% and a 10 year local recurrence rate as high as 88%3. The standard treatments for chordoma are surgery and radiotherapy, and there are currently no drugs approved for the treatment of chordoma. Chordomas are generally resistant to cytotoxic chemotherapy4. Most chordoma patients experience local recurrence, especially those with skull-base chordoma (SBC)5. Historically, SBC has been considered resistant to conventional chemotherapy and radiotherapy, with incomplete tumor resection and advanced radiation therapy techniques as the primary treatments for localized tumors due to the special location of the skull-base and the emphasis on preserving nerve function (Walcott et al., 2012). Radiation therapy techniques include gamma knife stereotactic radiation (GKSR) therapy and proton beam (PB) therapy6. Studies have shown that with a radiation dose of less than 60 Gray (Gy), such as GKSR therapy, the 5 year recurrence rate is 28%6. Therefore, high-dose radiotherapy (>60 Gy), such as PB therapy, is used to irradiate the tumor bed. However, 26% of patients who received high-dose radiotherapy after surgery still experienced recurrence3. The identification of predictive biomarkers of radiotherapy resistance in chordoma is urgently needed.
Over the last decade, genomic studies of chordoma have revealed several potential oncogenes in chordoma, including somatic variants in LYST, PI3K signaling genes and chromatin modeling genes7. A previous study showed that somatic duplications of the TBXT gene confer major susceptibility to familial chordoma8. In addition, copy number alterations (CNAs), such as deletions of CDKN2A, and loss of 9p21, 1p36 and 22q, are frequently observed in chordoma tumors6. However, the effects of these genomic changes on downstream gene functions remain remains unclear. Most of these genomic studies of chordoma have demonstrated frequently occurred copy number alterations, suggesting possible chromosome instability (CIN). Although widespread in most other tumors9,10,11, CIN has not been comprehensively characterized in chordoma.
Clinical studies targeting oncogenic genes such as CDK4/6 (ClinicalTrials.gov Identifier NCT03110744), EGFR (ClinicalTrials.gov Identifier NCT03083678, NCT05041127), PDGFR (ClinicalTrials.gov Identifier NCT01407198), and TBXT (ClinicalTrials.gov Identifier NCT02383498), and immune checkpoints, have been conducted on chordoma patients. However, only a small proportion of patients responded to those therapies. Despite the progress mentioned above, there is still a large percentage of SBC patients without available targeted therapeutic options. Additionally, due to the heterogeneity of the immune microenvironment of tumors12, it is critical to profile the immune microenvironment landscape of SBC, which could become the cornerstone for the development of targeted drugs.
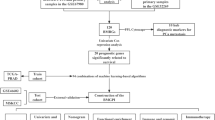
To explore the mechanism of SBC recurrence and discover actionable therapeutic targets, here we perform genomic, transcriptomic, proteomic, and phosphoproteomic analysis of 187 tumor samples. Our study reveals the relationships between genetic alterations and transcriptional or translational regulation. Furthermore, we establish an unbiased molecular classification based on proteomics data to uncover the mechanisms of SBC and explore targetable markers. The underlying data serves as an essential resource for further biological features, diagnostic markers, and drug discovery.
Results
Proteogenomic landscape of SBC
To establish a proteogenomic landscape for SBC to improve treatment responses, we collected 187 tumor samples from 162 SBC patients admitted to Huashan Hospital (Shanghai, China) via surgical resection. The 187 samples included 121 primary tumors and 66 recurrent tumors (Fig. 1A; Methods). The histopathology of each SBC sample was confirmed by at least two expert pathologists. The clinical data, including age, radiotherapy dose, radiotherapy outcome, overall survival (OS), progression-free survival (PFS), tumor anatomy, surgical outcome, etc., are summarized in Supplementary Data 1. To analyze the impact of tumor location on outcomes, we divided all tumors into three groups based on tumor anatomy: the seller group (n = 54), craniocervical junction group (n = 11), and clivus group (n = 122). Survival Kaplan-Meier (K-M) curves were generated to compare OS and PFS among the three groups. The results showed no significant difference of OS and PFS among three groups based on anatomy (Supplementary Fig. 1A and 1B). According to previous studies, although the location of SBC was related to the difficulty of gross total resection13, it did not appear to significantly impact prognosis14. Moreover, we classified the tumors into two groups based on surgical outcomes: the gross total resection (GTR) group and the incomplete resection (IR) group. Survival K-M curves revealed no significant differences in OS or PFS between the GTR group and the IR group in our cohort (Supplementary Fig. 1C and 1D). This finding was consistent with previous studies14,15. Several previous studies have reported the surgical outcome (GTR vs IR) to be the predictors of outcomes, thus we performed further analysis to explore the reason for the lack of a significant difference in prognosis between the GTR group and the IR group in our study. In terms of PFS, it was hypothesized that the administration of radiotherapy following IR might have impacted PFS in these patients. We observed that within the IR group, 34 patients received radiotherapy after surgery, which might have led to their longer PFS. To this end, we further divided all tumors into three groups based on both surgical outcomes and records of radiotherapy: the GTR group (n = 60), the IR without post-operative radiotherapy group (n = 90) and the IR with post-operative radiotherapy group (n = 34). Furthermore, we compared PFS among these three groups. K-M curves revealed a significant difference in PFS between the GTR group (n = 60) and the IR without post-operative radiotherapy group (n = 90), while there was no significant difference in PFS between the GTR group (n = 60) and IR with post-operative radiotherapy group (n = 34) (Supplementary Fig. 1E, F). In terms of OS, we recorded the time from disease onset to death or loss to follow-up. During this period, the majority of our patients received radiotherapy, which might affect the differences observed between patients who underwent complete resection and those who underwent incomplete resection. These findings could preliminarily explain the lack of significant differences in OS and PFS between the two surgical outcome groups in our cohort.
A Schematic overview of the number of tumors profiled and various data types data acquired for this cohort. B Genetic profile of genes that were mutated in at least 4% of the cases (upper) or known chordoma-related genes. C Comparisons of tumor mutational burden (TMB) between SBC cohort and other cancer cohorts included in The Cancer Genome Atlas (TCGA). D Significant GISTIC arm-level copy number alterations (CNAs) in primary SBC tumors (q < 0.1). E The percentage of arm-level CNA gain and loss events in primary SBC tumors. F Distribution of chromosome instability (CIN) status and GISTIC CNAs in SBC tumors. Samples are ordered by CIN score. G Survival Kaplan–Meier curves of primary SBC patients with CIN-high (CIN + , n = 43) or CIN-low (CIN-, n = 61) status (p-value from log rank test). Left panel, overall survival (OS); right panel, progression-free survival (PFS). H CIN score among primary tumors, recurrent tumors without radiotherapy and recurrent tumors after radiotherapy in SBC (Wilcoxon rank-sum test, p = 0.0024, p = 0.0004). Primary tumor, n = 107; recurrent tumor without radiotherapy, n = 36; recurrent tumor after radiotherapy, n = 23. The middle bar represents the median, and the box represents the interquartile range; bars extend to 1.5 × the interquartile range. Source data are provided with this paper.
The cohort consisted of 52% male patients and 48% female patients, with a median age of 45.5 years (range, 11–80 years). A comparison of the current cohort with previously published chordoma cohorts5,7,16 indicated that basic patient features (i.e., age, sex and history of treatment) were similar, although some distinctive features were observed in our cohort (Supplementary Data 1). Our cohort consisted of 66 (35%) recurrent tumor samples. Initially, 121 primary tumors were obtained from treatment-naïve SBC patients. However, while retrospectively screening electronic medical records, we found several patients with available clinical and prognostic records who had progressive disease. Importantly, these patients also underwent tumor resection surgery at Huashan Hospital after recurrence, enabling our expansion of the cohort to include 66 recurrent tumor samples, including 38 recurrent tumors without radiotherapy and 28 recurrent tumors after radiotherapy (Supplementary Fig. 1G, H, and S1I; Methods). In our study, 19 patients had one primary tumor and one matched recurrent sample, and 2 patients had one primary tumor and matched samples of two recurrences. In addition to these 21 patients, two patients (P122 and P123) had one recurrent sample before radiotherapy and one matched recurrent sample after radiotherapy. Overall, 23 patients had paired tumor samples from before and after recurrence (Supplementary Fig. 1J; Methods).
Homogenized tumor samples were aliquoted for molecular profiling via whole-exome sequencing (WES), RNA sequencing (RNA-seq), proteomics, and phosphoproteomics. WES was conducted on 163 tumor samples with a mean depth of 200X; 24 tumor samples were excluded due to low DNA quality. In total, WES data from 95 paired tumor-blood SBC samples, which consisted of 68 paired primary samples and 27 paired recurrent samples, were included in subsequent somatic mutation analysis. After processing and filtering for quality, a total of 1903 mutations were detected including 1748 single-nucleotide variants (SNVs) and 155 small insertion-deletions (indels) (Supplementary Data 2). We found that PCDHA3 (9%) and LYST (6%) were the most frequently mutated genes in primary SBCs (Fig. 1B), and both the mRNA and protein expression of these mutant genes were not significantly different from those in SBCs lacking mutations in these genes. Furthermore, no significant differences in the number of mutated genes or frequency of mutations were found between primary and recurrent SBCs (Supplementary Fig. 1D). In addition, we noted that the majority (98%) of mutated genes occurred in only one or two samples (Supplementary Fig. 1D; Supplementary Data 2), which indicated high intertumoral heterogeneity in the somatic mutation landscape among SBC patients. Meanwhile, as shown in Supplementary Fig. 2A, the recurrent samples in general had fewer mutations in the displayed genes, indicating the diverse top mutations between the primary cohort and the recurrent cohort. Specifically, the most common mutations found in recurrent tumors, such as C8B, CDH23, COL3A1, and CREBBP, were more frequently mutated in recurrent tumors than in primary tumors (Supplementary Fig. 2B), suggesting that recurrent tumors had a mutation panel distinct from that of primary tumors. Additionally, there was no significant difference of TMB between primary and recurrent tumors (Supplementary Fig. 2C), indicating that recurrent samples had comparable TMB level with primary samples. Overall, we found that the primary top mutated genes were distinct from the recurrent top mutated genes, suggesting that recurrent tumors might have different mutation patterns compared with primary tumors.
Consistent with the previous studies16, the tumor mutational burden (TMB, median = 0.26 mutations/Mb per sample, range = 0.02–5.64 mutations/Mb per sample, Supplementary Data 1) of most SBC samples was relatively low, and generally lower than that of most cancer types sequenced in The Cancer Genome Atlas (TCGA) (Fig. 1C). Although previous genetic studies have shown that mutations may impact some cancer-associated processes in chordoma5,7,16, the relatively low TMB and extensive heterogeneity in this cohort suggested that the mutations detected likely had limited impacts on the downstream regulation of the oncogenic process in SBC.
We then conducted RNA-seq analysis on 180 tumor samples that passed quality control measures (excluding seven samples due to poor RNA quality), resulting in a set of transcriptional profiles for 18,788 genes that had fragments per kilobase of transcript per million fragments mapped (FPKM) above one (Supplementary Fig. 2D; Methods). For subsequent proteomic and phosphoproteomic analysis, we performed consistent and rigorous quality control methods (Supplementary Fig. 2D, 2E, and 2F; Methods). Pearson’s correlation coefficient was calculated for all quality control (QC) runs using standard samples (Supplementary Fig. 2E; Methods). The average correlation coefficient of the QC samples was 0.97 (range, 0.96–0.99), thus validating the consistency and stability of our mass spectrometry (MS) platform (Supplementary Fig. 2E). Both the tumor proteome and phosphoproteome exhibited unimodal distributions and passed the proteomics quality control procedure (Supplementary Fig. 2D; Methods). In our cohort, 187 SBCs and 174 SBCs that passed quality control and were used for further proteomic and phosphoproteomic analysis, respectively. The density plot of the normalized intensities of the proteins identified in each sample demonstrated that all these samples passed the quality control with an expected unimodal distribution (Supplementary Fig. 2D). Furthermore, we performed PCA analysis on both proteomic and phosphoproteomic profiles. The PCA plots showed no significant batch effects in either proteomic or phosphoproteomic profiles (Supplementary Fig. 2F). In summary, our quality evaluation confirmed the high quality and integrity of the proteomic and phosphoproteomic profiles used for further analysis. Label-free quantification of the 187 tumor samples yielded a total of 11,639 proteins (at a 1% false discovery rate (FDR) at the protein and peptide levels), with an average of 7624 proteins per sample. Through this analysis, a total of 27,121 phosphosites (belonging to 8,151 phosphoproteins) were quantified and identified in our cohort. The Feature counts for each multi-omics dataset are shown in Fig. 1A.
This study thus established a comprehensive landscape of SBC tumors at the genomic, transcriptomic, proteomic, and phosphoproteomic levels, which also enabled exploration of tumor recurrence-associated proteins and screening for potential targets to enhance radiotherapy sensitivity in SBC patients.
The genomic characterization and CIN of SBC
Previous studies have shown that chordoma is characterized by frequent CNAs7,16,17. Analysis of CNAs using WES data (Methods) revealed that the most significantly altered (q < 0.1) arm-level amplifications in primary tumors were located on chromosomes 1q, 2p and q, 5p and q, 6p and q, 7p and q, and 21p, while deletions were detected on chromosomes 3p and q, 4p and q, 9p and q, 10p and q, 13q, 14q, 17p, 18p and q, 19p and q, 21p and 22q (Fig. 1D; Supplementary Data 2), which was consistent with previous studies16,17. More specifically, amplifications of chromosomes 1q, 7p and 7q and deletions of chromosomes 1p, 3, 4, 9, 10, 13q, 14q, 18, and 22q identified in our cohort were also detected by Bai et al16. Previously reported focal level CNAs were also identified in our cohort16, including amplifications of 1p21.1 and 1q21.2, and deletions of 3p21, 9p21.3, and 22q11.21 (Supplementary Fig. 2G; Supplementary Data 2). The majority (86%) of primary SBC tumors displayed arm-level amplifications and deletions, which was similar to the findings that 77.5% of the primary chordoma samples had arm-level SCNAs in a previous study16. Based on the arm-level CNA results (Fig. 1E), the top 10 amplified arm frequencies were as follows: 7p (61%), 7q (60%), 21p (47%), 1q (40%), 6q (39%), 5p (37%), 5q (36%), 2p (34%), 2q (34%), 6p (33%). The top 10 frequently deleted arms were: 22q (60%), 3p (49%), 13q (48%), 14q (46%), 10q (45%), 3q (44%), 10p (41%), 9q (38%), 9p (37%) and 18p (36%). These findings were highly consistent with the findings regarding arm-level events in previous studies on the genomic characteristics of chordoma16,17,18,19. Additionally, we found that the majority of the arm-level CNA events significantly co-occurred in a subgroup of SBCs (Fisher’s exact test, p < 0.05), whereas the other subgroup of SBCs had very few arm-level CNA events (Supplementary Fig. 2H), suggesting high diversity in the level of CIN among SBCs.
CIN is a hallmark of human cancers that leads to the introduction of CNAs during cell division. Moreover, high CIN is associated with poor prognosis, metastasis, and anti-neoplastic therapeutic resistance9,20. As CIN can be inferred by CNA data generated from WES data in previous studies21,22,23, we calculated CIN scores for each tumor sample to estimate their CIN status (Supplementary Data 1; Methods). We then categorized the SBC tumors into CIN-high (CIN + ) or CIN-low (CIN-) subgroups based on the distribution of CIN scores (Fig. 1F; Methods). We also investigated the influence of tumor purity on CIN. There was no significant difference in tumor purity between CIN+ SBCs and CIN- SBCs (Supplementary Fig. 2I). Further analysis of data from primary tumors showed that CIN+ status was significantly correlated with poor OS and PFS, suggesting that CIN could be prognostically informative (Fig. 1G). Among all tumors, the CIN+ tumors also showed a significant association with worse OS and PFS (Supplementary Fig. 3A). The comparison of primary and recurrent tumor CIN score showed that recurrent tumors had significantly higher CIN scores, suggesting that CIN status was also related to SBC recurrence (Fig. 1H; Wilcoxon rank-sum test, p = 0.0024, p = 0.0004). Moreover, we incorporated a investigation on the difference in patient prognosis based on both CIN and the surgical outcomes. Here, we divided the cohort into six groups: (1) GTR CIN + , (2) GTR CIN-, (3) IR CIN+ without post-operative radiotherapy (referred to CIN- patients who underwent incomplete resection and did not receive post-operative radiotherapy), (4) IR CIN- without post-operative radiotherapy (referred to CIN- patients who underwent incomplete resection and did not receive post-operative radiotherapy), (5) IR CIN+ with post-operative (referred to CIN+ patients who underwent incomplete resection and received post-operative radiotherapy), and (6) IR CIN- with post-operative (referred to CIN- patients who underwent incomplete resection and received post-operative radiotherapy). The K-M analysis revealed significant differences in OS and PFS among these six groups (Supplementary Fig. 3B), indicating that the incorporation of CIN status with surgical outcomes can further differentiate the prognosis of SBC patients. The “IR CIN+ ” group displayed significantly worse OS and PFS compared with other groups (Supplementary Fig. 3C), suggesting that CIN could serve as an additional prognostic factor for patients with residual tumors after surgery. These collective results indicated that variation in CIN status reflected the genetic heterogeneity among SBC patients, and could therefore potentially serve as a prognostic indicator and/or therapeutic target in treatments of SBC.
In addition, we utilized the T2T reference genome to validate our CIN findings. The T2T reference genome provided a more comprehensive and updated reference of the human genome24,25, which is a valuable resource for various genomic studies and analyses. We compared the outcomes obtained using the Hg19 reference genome with those obtained using T2T. The results revealed a strong positive correlation between the Hg19 CIN score and the T2T CIN score (Supplementary Fig. 4A, Pearson’s correlation, r = 0.98, p < 2.2e-16), indicating high concordance between the CNA results of T2T and Hg19. The T2T CIN score was then used to classify SBC samples into CIN+ and CIN- groups. We assessed the consistency between samples classified as CIN+ or CIN- based on the T2T and Hg19 reference genomes. We found that 97.67% of the CIN+ samples demonstrated consistency between the T2T and Hg19 classifications, while 92.21% of the CIN- samples exhibited concordance (Supplementary Fig. 4B). Classifying CIN status in SBC tumors using the T2T reference genome showed remarkably high similarity to CIN status results obtained from the previous analysis utilizing the Hg19 reference genome. The distribution and diversity of T2T CNAs were similar to those of Hg19 CNAs (Supplementary Fig. 4C). The significant concordance between the updated results obtained using the T2T reference genome and the previous results obtained using the Hg19 reference genome supported the stability and reliability of our findings on CIN in SBC. To explore survival and recurrence prognosis differences, we performed OS and PFS analyses by dividing the samples into T2T CIN+ and T2T CIN- groups. T2T CIN + SBC patients exhibited significantly worse prognosis compared with T2T CIN- patients, consistent with the previous outcomes of Hg19 CIN+ group (Supplementary Fig. 4D), validating our previous finding that CIN could be a potential prognostic marker in SBC. Moreover, we identified significant chromosome arm gain or loss events form the CNA data using the T2T reference genome. The results showed that 1q gain. 9p loss and 10q loss were significant in the primary SBC cohort, consistent with our previous observations using the Hg19 reference genome (Supplementary Fig. 4E). Collectively, these results obtained from WES data using the T2T reference genome were consistent with above analyses using the Hg19 reference genome, suggesting the robustness and validity of our findings.
To further validate these findings and expand our understanding, we conducted fluorescence in situ hybridization (FISH) analysis on the identified CIN+ samples. Specifically, FISH was performed on the samples that were identified as having 1q gain, 9p loss or 10q loss, respectively. FISH for chromosome 1q gain was performed using the GSP 1q21/1p36 probe following previous studies26. The GSP 9p21/CSP 9 probe27 and the GSP 10q23/CSP 10 probe28,29 were used in FISH for chromosome 9p loss and 10q loss, respectively (Methods). Based on the CNA results obtained from the WES data, we selected samples with specific arm-level CNAs, including 1q gain, 9p loss and 10q loss, for FISH analysis. The FISH results revealed specific arm-level CNAs in the tested samples. Sample N11S1666 (from Patient #P012) showed 1q gain, sample N13S1303 (from Patient # P068) showed 9p loss, and sample N14S2329 (from Patient #P161) showed 10q loss (Supplementary Fig. 4F). The FISH results of these samples confirmed that our previous analysis of arm-level events using WES was reliable.
In addition to the CIN observed in our WES-based analysis of copy number alterations (CNAs), there were various other types of CIN. Due to the limitations of our WES data analysis in delineating all types of CIN, we employed FISH to explore other forms of CIN. Specifically, we detected micronuclei and anaphase bridges in the CIN+ samples. In consistent with our result, previous studies have suggested that various types of CIN coexist9, such as micronuclei and anaphase bridges. Micronuclei are small membrane-bounded compartments with a DNA content encapsulated by a nuclear envelope that spatially separated from the primary nucleus during mitosis when whole or fragmented chromosomes fail to segregate properly30. Anaphase bridges, on the other hand, arose from structural abnormalities or defective disjunction of the sister chromatids during anaphase, leading to DNA threads being stretched between separating chromosomes31. We performed immunofluorescence staining on CIN+ samples, in which DNA was stained with DAPI (blue), following established protocols described in previous research studies32,33. We found small DNA-containing nuclear structures that were spatially isolated from the main nucleus, which could be identified as micronuclei (Supplementary Fig. 4G). For anaphase bridges, we performed FISH and immunofluorescence (IF) staining in CIN+ samples (Methods). These results preliminarily demonstrated disrupted bridge-like structures in the CIN+ samples, which represented anaphase bridges (Supplementary Fig. 4H). The observation of micronuclei and anaphase bridges in our CIN + SBC samples expanded the understanding of CIN phenomena in SBC and highlighted the complexity and heterogeneity of CIN in SBC. These findings provided compelling evidence that multiple forms of CIN could coexist within the same sample, reinforcing the notion that different mechanisms contribute to CIN. These additional results not only strengthened the validity of our initial findings based on WES data but also emphasized the significance of comprehensive consideration of various CIN phenomena in evaluating genomic instability in SBC for future studies.
Proteogenomic analysis of CIN + SBC
To better understand the effects of CIN on SBC, we examined differences between CIN+ and CIN- tumors using both RNA-seq data and the proteome data. We calculated the ssGSEA scores of hallmark pathways in each sample using transcriptomic data and proteomic data. As a result, at both transcriptomic and proteomic level, the pathways including MYC targets, mTORC1 signaling, unfolded protein response, and E2F targets pathways were upregulated in the CIN+ group (FDR < 0.05), while the coagulation, allograft rejection and apoptosis pathways were upregulated in the CIN- group (FDR < 0.05) (Supplementary Fig. 5A). Along with this finding, gene set enrichment analysis (GSEA) of differentially expressed proteins (DEPs) based on the proteomic data also revealed that oncogenic pathways including MYC targets, E2F targets, mTORC1 signaling and DNA repair pathways were significantly upregulated in CIN+ SBCs (FDR < 0.05), while pathways associated with the tumor microenvironment, including coagulation, allograft rejection, and epithelial mesenchymal transition pathways, as well as the apoptosis pathway were significantly downregulated (Fig. 2A; Supplementary Data 3). These results suggested that the differential pathways identified using proteomic data were consistent with the findings obtained using transcriptomic data. These upregulated pathways suggested greater proliferative potential in SBCs with higher CIN. We therefore calculated the multi-gene proliferation score (MGPS), an indicator of tumor cell cycle progression potential34,35, for each sample, which revealed a significant correlation between MGPS score and CIN score (Fig. 2B; Spearman’s correlation, r = 0.29, p = 2.2e-04). Furthermore, we analyzed the correlations of the CIN score and other alternative gene sets that can indicate tumor proliferation, such as the G2M checkpoint, cell cycle checkpoint, cell cycle, and cell cycle DNA replication pathways, to further validate the correlation between CIN and proliferation. These gene sets were reported to be strongly associated with tumor proliferation in previous studies36. For instance, Yuan et al.37 and Petralia et al.38 used the expression of the cell cycle gene set to assess active proliferation in their studies. Wang et al39. used cell cycle checkpoints and DNA replication pathways to indicate the proliferation ability of medulloblastoma. Our results showed that the G2M checkpoint, cell cycle checkpoint, cell cycle, and cell cycle DNA replication pathways were all positively correlated with the CIN score and were upregulated in the CIN+ group compared with the CIN- group (Supplementary Fig. 5B) We also observed that several proliferation-related proteins, including CDC7, MCM6, MSH2, PCNA, RHEB, and G3BP1, were significantly upregulated in the CIN + SBC tumors compared with the CIN- tumors (Supplementary Fig. 5C). These results suggested that a higher level of CIN might promote tumor proliferation in SBC. We further investigated the association between CIN and proliferation in previously published studies40,41,42. An increased degree of CIN was reported to be positively correlated with increased proliferation signatures in several studies in other tumor types40,41,42. Moreover, the results of immunohistochemistry (IHC) analysis showed that CIN+ SBCs had higher histochemistry score (H-score) for the cell cycle (DNA damage repair) marker, MSH2, than CIN- SBCs (Supplementary Fig. 5D). These findings suggested that CIN+ could promote tumor cell cycle progression and proliferation in SBC.
A Enrichment analysis of differential expressed proteins (FDR < 0.05) between CIN+ and CIN- SBCs. B Scatterplot showing the Spearman’s correlation coefficient and p-value of the MGPS score versus CIN score (two-sided, 95% CI for the regression band), n = 163. C The proliferation curve of the CIN+ cells and the control cells (n = 3, mean ± SEM, biological replicates). D The flow cytometry analysis showing cell cycle progression of the CIN+ cells compared with the control cells. E ssGSEA scores of known CIN cause pathways between CIN+ (n = 86) and CIN- (n = 77) SBC samples (Student’s t-test, two-sided). The middle bar represents the median, and the box represents the interquartile range; bars extend to 1.5 × the interquartile range. F The heatmap of CIN score and protein abundance of DNA replication stress (RS) markers, n = 163. The Spearman’s correlation p-values between the CIN score and the protein/pathway, and the Student’s t-test p-values (two-sided) between CIN+ and CIN- samples were displaying in asterisks. The significance is defined as: n.s., not significant; *p < 0.05; **p < 0.01; ***p < 0.001. G Scatterplot showing the Spearman’s correlation (two-sided) between the ssGSEA scores of the DNA RS pathway and hallmark pathways. H Scatterplot showing the Spearman’s correlation coefficients (two-sided) of the CIN score versus mRNA expression levels (x axis) and transcription factor (TF) activities (y axis) of E2Fs. I Scatterplot showing the Spearman’s correlation coefficients (two-sided) between the E2F3 TF activity and kinase activities, n = 157. J Heatmap of the multi-omics features related to regulation of cell cycle in CIN + SBC. K Apoptosis pathway expression score are negatively correlated with CIN score in SBC. Spearman’s correlation and p-value are shown (two-sided, 95% CI), n = 163. L The flow cytometry analysis showing decreased apoptosis in the CIN+ cells compared with the control cells. Annexin V-positive cells (early apoptotic cells, Q4) and Annexin V and PI double-positive cells (late apoptotic cells, Q2) are shown.
To investigate the difference in proliferation levels between CIN+ cells and control cells and validate the relationship between CIN and proliferation, we generated monoclonal CIN+ cells through Cytabirine treatment (Methods). These cells were further identified using WES data, and confirmed by MS and FISH analysis. Subsequent experiments were conducted on CIN+ cells and control cells to assess their proliferation. The CellTiter-Glo Luminescent Cell Viability Assay was used to detect the number of surviving cells43 (Methods). By plotting the proliferation curves of CIN+ cells and control cells, we observed increased proliferation rates in all groups of CIN+ cells compared to the control group (Fig. 2C). The results indicated that the proliferation of CIN+ cells were promoted compared with control cells. Furthermore, flow cytometry analysis was performed to investigate the changes in cell cycle progression in CIN+ cells and control cells (Fig. 2D; Methods). The results demonstrated that the percentage of S-phase CIN+ cells was higher that that of the control, which indicated that G1/S transition might be promoted in CIN+ cells. In addition, the G2-phase cells in the control increased compared with the G2-phase CIN+ cells, which demonstrated that the G2/M transition might be upregulated in CIN+ cells. The results demonstrated that cell cycle progression was promoted in CIN+ cells. Taken together, additional experimental results, combined with our previous findings based on proteomic data, provided evidence suggesting that CIN + SBC tumors were associated with enhanced proliferation.
CIN can be induced by several factors, including DNA replication stress (RS) and mitotic errors, among others9,44,45. Thus, to investigate the putative cause of CIN in SBC, we explored pathways associated with known mechanisms of CIN using ssGSEA. The putative causes analyzed in our study were concluded to be the known putative causes of CIN in Drews et al.’s recently published study of the pan-cancer compendium of chromosomal instability9. The results revealed that the replication stress pathway was significantly upregulated (Wilcoxon sum-rank test, p = 9.33E-05; Student’s t-test, p = 1.4E-04) in CIN+ tumors compared with CIN- tumors (Fig. 2E), while other pathways, including chromosome segregation during mitosis, telomere dysfunction, homologous recombination, non-homologous end-joining, and PI3K-AKT activation pathways, did not significantly differ between the CIN+ and CIN- groups, suggesting that replication stress might be the main contributor to the instability of chromosome copy number events in SBC. Furthermore, the ssGSEA score for the DNA RS pathway also strongly correlated with CIN score (Supplementary Fig. 5E; Spearman’s correlation, r = 0.4, p = 2.1e-07), suggesting that DNA RS was likely responsible for CIN in SBC. In our study, we calculated the CIN score based on CNAs derived from WES data, following the method described in previous studies10,46. Specifically, we utilized the CNA-derived “numerical” CIN score for the identification and classification of CIN + SBC tumors. This approach aligned with the methods employed in multiple published studies40,42. Although the only cause showing a significant difference between the CIN+ and CIN- groups in our study was RS, indicating its significance in numerical chromosomal instability (CIN) of SBC, it is important to note that various causes of CIN are interconnected, and other mechanisms may also play crucial roles in different types of CIN.
DNA RS is a state of dysregulation in DNA replication that accompanies many cancers, and can trigger various DNA-related pathways such as DNA strand breaks, DNA damage response, and DNA repair, eventually resulting in CIN44,47. Further analysis showed that the ssGSEA scores for these pathways, together with mRNA and protein expression levels of their associated genes, were positively correlated with CIN score (Supplementary Fig. 5F). RS is a significant hallmark of tumors and a major cause of genomic instability, which has been reported in many studies48. The RS gene set used in our study was consistent with that used in Msaouel et al.’s study49. Here, we presented the gene sets and markers associated with replication stress, which were commonly used in previous studies49,50,51. We found that 85% (12/14) of the RS genes identified in our study were also significantly positively correlated with the CIN score (Supplementary Fig. 5G). Marker genes for RS, such as ORC2 (Student’s t-test, log2FC = 1.72, p = 3.6E-28), CDC7 (Student’s t-test, log2FC = 1.78, p = 3.6E-28), MCM2 (Student’s t-test, log2FC = 1.43, p = 2.66E-21), and RPA1 (Student’s t-test, log2FC = 0.74, p = 6.8E-03) were significantly upregulated in CIN+ tumors compared with CIN- tumors. The Replication Protein A (RPA) complex, proliferating cell nuclear antigen (PCNA) and TP53BP1 can serve as markers of DNA RS52. Interrogation of proteomics data indicated that the expression levels of RPA1 (Student’s t-test, log2FC = 0.74, p = 6.8E-03), PCNA (Student’s t-test, log2FC = 0.74, p = 6.8E-03) and TP53BP1 (Student’s t-test, log2FC = 1.47, p = 9.4E-37) protein levels were all significantly elevated in CIN+ SBCs (Fig. 2F), confirming that DNA RS occurred in these tumors. Histone chaperones are also necessary for genome maintenance and stress tolerance, as key mediators of efficient cellular responses to replication stress53. The phosphorylation of the H2AX protein, an evolutionarily conserved variant of histone H2A, was reported as a marker for RS in previous studies44,54. We analyzed the abundance of the histone H2AX phosphoprotein based on the phosphoproteomic data in our study. The results showed that the level of H2AX phosphoprotein was significantly upregulated in CIN + SBC tumors compared with CIN- SBC tumors (Fig. 2F, Student’s t-test, p = 0.0216, log2FC = 0.302). Together, these results suggested that CIN + SBC tumors displayed increased DNA RS, consistent with previous reports of the RS phenotype in other CIN+ tumors52,55.
To illustrate the mechanism under which DNA RS impact the CIN+ tumors, we calculated the Spearman’s correlation coefficients between ssGSEA scores for hallmark pathways and the DNA RS pathway, which revealed that the DNA RS gene set was most highly correlated with the E2F targets gene set (Fig. 2G; Supplementary Data 3; Spearman’s correlation, r = 0.73, p = 1.6e-32). E2F target genes are the downstream of the E2F transcription factor56. Further investigation of E2F target genes revealed significantly increased expression levels of several E2F target genes associated with RS, including MCM2-7, ORC2 and RPA1 (Supplementary Fig. 5H). Sustained E2F transcriptional activity is reportedly necessary for cell survival under elevated DNA RS conditions56,57. Among all E2F family members, only E2F3, a key E2F activator, showed a positive correlation with the CIN score at mRNA expression, protein expression and transcription factor (TF) activity levels in SBC (Fig. 2H and Supplementary Fig. 5I; Supplementary Data 3). As proteins are functional executors of cells, we further investigated the protein abundance of E2F3 in SBC tumors. The result showed that E2F3 protein expression level was positively correlated with the CIN score (Spearman’s correlation, R = 0.75, p < 2.2e-16) and was significantly increased in the CIN+ group (Student’s t-test, p = 9.24E-69). These results suggested that E2F3 might be responsible for the aberrantly high expression of E2F targets in CIN+ SBCs. Although the MYC targets gene set was also observed to be positively correlated with DNA RS pathway, the expression level of MYC itself was negatively correlated with both the DNA RS pathway and the CIN score; whereas the expression level of E2F3 was positively correlated with both the DNA RS pathway and the CIN score (Supplementary Fig. 5J). Collectively, our findings indicated that E3F targets rather than MYC were related to RS and CIN in SBC.
E2F3 is an established target of cell cycle checkpoint regulation proteins, such as CDKN2A, cyclin-dependent kinases (CDKs), cyclins (CCNs), and RB158. Phosphoproteomic analysis showed that the kinase activity (Methods; Supplementary Data 3) levels of several CDKs, including CDK1, CDK2, CDK4 and CDK5, were positively correlated with E2F3 transcriptional activity (Fig. 2I). In addition, CDK4 kinase activity was significantly correlated with CIN+ SBCs (Supplementary Fig. 5K). We also performed KSTAR analysis59 of the phosphoproteomic data to further predict kinase activities (Methods). The results substantiated our prior findings, revealing significantly elevated kinase activities of CDK1, CDK2, CDK4, and CDK5 in tumors with high E2F3 TF activity compared to those with low E2F3 TF activity (Supplementary Fig. 5L). These results supported our conclusion that the activation of CDKs was associated with increased E2F3 TF activity. In our study, CDKN2A deletion, proposed as a potential biomarker for CDK4 inhibitors60, was detected more frequently in CIN+ tumors compare to CIN- tumors (Supplementary Fig. 6A; Fisher’s exact test, p < 0.001), which aligned well the increased CDK4 kinase activity in CIN + SBC. RB1, which directly binds E2F to suppress its activity, can be inactivated via CDK-RB1-mediated phosphorylation or by deletion of RB1 itself56. Our data revealed that RB1 deletion was enriched in CIN+ SBCs (Supplementary Fig. 6B). In addition, phosphorylation levels of RB1 phosphoprotein (Spearman’s correlation, r = 0.53, p = 2.94E-13) and the phosphorylation sites on RB1, such as RB1 S350, S807 and T373, were significantly correlated with E2F3 TF activity (Supplementary Fig. 6C). Furthermore, we performed IHC to detect the difference in expression level of phospho-Rb1 (Ser807) (8516 T, 1:200; Cell Signaling Technology) between samples with high and low E2F3 TF activity based on the inferred TF activity score (Methods), in order to validate the association between E2F3 TF activity and RB1 phosphorylation. The IHC results showed the expression level of phospho-Rb1 (Ser807) was significantly upregulated in patients with high E2F3 TF activity (Supplementary Fig. 6D and 6E, Student’s t-test, p = 0.002). We also explored the correlations between E2F3 TF activity and all the other related proteins and phosphoproteins (Supplementary Fig. 6C). The results revealed that E2F3 TF activity were significantly correlated with CIN score (R = 0.23, p = 3.38E-3), CDK4 kinase activity (R = 0.26, p = 7.79E-4), RB1 phosphoprotein (R = 0.53, p = 2.94E-13), CDC7 kinase activity (R = 0.25, p = 1.15E-3), MCM2 protein (R = 0.48, p = 8.48E-10), MCM2 phosphoprotein (R = 0.22, p = 4.01E-3), and MCM S27 phosphosite (R = 0.19, p = 0.016). These results indicated that E2F3 TF activity was associated with CDK4 activity, RB1 phosphorylation and CDC7 kinase activity, suggesting that E2F3 TF activity might be important in regulating the response to CIN in SBC. In summary, we performed multi-omics analysis to investigate the regulation of E2F3 TF activity in CIN + SBC tumors, and conducted IHC to validate the relationship between E2F3 TF activity and RB1 phosphorylation. We found that phosphorylation of RB1 was related to E2F3 TF activity in our study, suggesting that a CDK4 activation-mediated suppression of RB1 or RB1 deletion-associated mechanism of E2F3 activation leading to a CIN+ phenotype in SBC (Fig. 2J).
Interestingly, correlation analysis also showed that the kinase activity of CDC7, which can be activated by E2F TF61, was significantly upregulated by E2F3 in our dataset (Supplementary Fig. 6C, Spearman’s correlation, r = 0.27, p = 3.1e-04). CDC7 promotes the initiation of the DNA origin of replication by phosphorylating one or more subunits of the MCM complex, including MCM2, to facilitate the cell cycle transition62. Phosphorylation levels of MCM2 protein and MCM2 S27 phosphosite, which is the CDC7-dependent phosphorylation site, were significantly correlated with CDC7 kinase activity (Supplementary Fig. 6C, Spearman’s correlation, MCM2 phos: R = 0.86, p = 2.83E-46, MCM2 S27: R = 0.78, p = 6.21E-33). The phosphorylation levels of MCM2 and MCM2 S27 were also significantly correlated with the expression level of ASK protein (Supplementary Fig. 6F), as ASK is required for MCM phosphorylation63,64. These results suggested that the activation of E2F3 could promote cell cycle in CIN+ SBCs through CDC7-induced hyper-phosphorylation of MCM2. Additionally, we found that the phosphorylation levels of MCM2 and the S27 site on MCM2 were also significantly correlated with RS (Supplementary Fig. 6G), indicating that the increased phosphorylation of MCM2 might be involved in the response and tolerance to RS. High levels of CIN and sustained DNA RS usually induce apoptosis and cell death in non-transformed cells52. Conversely, our GSEA and ssGSEA analyses indicated downregulation of the apoptosis pathway in CIN+ SBCs (Fig. 2A and K). The deletion or downregulation of apoptosis-related genes, such as TP53, BAK1 and BAD, were also observed in CIN+ tumors (Supplementary Fig. 6H), indicating that CIN + SBC is also accompanied by suppression of apoptosis.
To further validate of our findings, we generated monoclonal CIN + SBC cells after treating UM-Chor1 cells with cytarabine (Methods). WES, proteomics as well as FISH analysis were performed to was conducted on monoclonal cells and control cells separately to analyze their CIN status and arm-level CNAs. LC-MS/MS and FISH analyses were performed to validate the CIN+ status of these cells as determined by WES data, confirming that the cytarabine-treated monoclonal cells were indeed CIN+ cells. Further experiments and analysis were performed to verify the relationship between the increased DNA RS level and the upregulation of E2F transcription in CIN + SBC cells. We performed western blot (WB) to detect the expression level of PCNA, which has been reported to be a marker of DNA RS47, in CIN+ cells and control cells. The results demonstrated that the PCNA expression level was significantly higher in the CIN+ cells than in the control cells (Supplementary Fig. 6I). Additionally, we analyzed the proteomic data obtained from both the CIN+ cells and control cells to compare the expression level of the RS gene set. The result revealed a significant upregulation of the RS pathway in the CIN+ cells compared to the control cells (Supplementary Fig. 6J). Furthermore, based on the proteomic comparative data analysis of the CIN+ cells and control cells, we observed a substantial upregulation of E2F targets in the CIN+ cells compared to the control cells Moreover, based on the MS data analysis of the CIN+ cells and control cells, we observed that the E2F targets pathway was significantly upregulated in the CIN+ cells compared with the control cells (Supplementary Fig. 6K). These results suggested that E2F transcription activity was upregulated in CIN+ cells with increased levels of replication stress. Additionally, to ascertain whether apoptosis was suppressed in CIN+ cells, flow cytometry was conducted on the CIN+ cells and the control cells. The results showed that the percentage of apoptotic CIN + SBC cells (1.56% in late apoptotic cells (Q2) and 0.73% in early apoptotic cells (Q4)) was lower compared with the control cells (9.23% in Q2 and 27.21% in Q4) (Fig. 2L). Taken together, we confirmed that DNA RS was induced in the CIN + SBC cells and that the apoptosis of the CIN+ cells decreased compared with that of the control cells. The corresponding experiments and analysis of CIN + SBC cells revealed elevated RS level and confirmed that the E2F transcription activity of these CIN+ cells was upregulated compared with the control cells.
Overall, this multi-omics analysis demonstrated that E2F transcription is upregulated in response to increased DNA RS, while apoptosis is suppressed in CIN + SBC, which resulted in dysregulation of the cell cycle progression. The collective evidence led us to hypothesize that dependence on E2F3 was a vulnerability that could be exploited by therapeutics targeting E2F3 and its downstream genes (CDC7, etc.) or other cell cycle regulators, such as CDK465.
Chromosome 1q gain led to a worse prognosis in SBC, which associated with mitochondrial protein homeostasis
Our WES analysis also revealed multiple arm-level gains and losses in the SBC samples. In particular, 1q gain was most significantly correlated with poor OS in our study (Fig. 3A, B; Supplementary Data 2), and associated with shorter PFS (Fig. 3B) within primary SBC cohort. We also observed that SBCs with 1q gain showed significantly worse PFS and OS among all SBC tumors (Supplementary Fig. 7A), suggesting that the 1q gain group consistently had a worse prognosis. Based on the copy number alteration events on chromosome 1q, we further divided all samples into three groups: 1q gain (n = 66), 1q WT (n = 86) and 1q loss (n = 11) groups (Supplementary Fig. 7B). There were 66 tumors with 1q gain event and 97 tumors without 1q gain event, including 86 WT tumors and 11 tumors with 1q loss event (Supplementary Fig. 7B). We also observed that 1q gain was a significant arm-level event in SBC (Fig. 1D), while 1q loss event was not significant in SBC, which was consistent with previous studies16. These results indicated a more significant and recurrent occurrence of the 1q gain event in SBC compared with that of the 1q loss event. The presence of “1q loss” in our analysis did not seem to significantly influence the association between 1q gain and CIN. We further observed that the 1q gain group had significant worse OS (Log-rank test, p = 0.0393) and PFS (Log-rank test, p = 0.0178) compared with the 1q WT group, while the 1q loss group showed no difference compared with 1q WT group (Supplementary Fig. 7C), suggesting that the 1q gain group had significantly worse PFS and OS in our study. Additionally, CIN+ tumors carried 1q gain more frequently than CIN- tumors (Fig. 3C, Fisher’s exact test, p < 1e-04), and CIN scores were significantly higher in tumors with 1q gain (Fig. 3D). Compared with WT tumors, tumors with 1q gain exhibited significantly higher CIN score (Supplementary Fig. 7D), consistent with our findings that CIN score were higher in “1q gain” than in “others”, indicating a strong link between chromosome 1q gain, CIN, and worse prognosis in these patients.
A Volcano plot showing significant arm-level CNA events in primary SBCs (n = 106) and their associations with prognosis (Hazard ratio, 95% CI). B Survival Kaplan–Meier curves of primary SBC patients with 1q gain (n = 38) or others (n = 66) (p-value from log rank test). Upper panel, OS; lower panel, PFS. C Stacked bar plot showing the proportions of tumors with or without 1q gain in CIN+ and CIN- SBC (Fisher’s exact test, two-sided, n = 163). D Boxplot showing differential CIN score among primary/recurrent SBC tumors with/without 1q gain (Wilcoxon rank-sum test): primary with 1q gain (n = 35), primary without 1q gain (n = 71), recurrent with 1q gain (n = 25), and recurrent without 1q gain (n = 31). The middle bar represents the median, and the box represents the interquartile range; bars extend to 1.5 × the interquartile range. E Venn diagram showing the significant cis events on chromosome 1q (Spearman’s correlation, two-sided, p < 0.05, Rho > 0.2), n = 163. F Pathways enriched for significant 1q cis-effect genes (q value < 0.05), n = 163. G GSEA plot showing upregulated mitochondrial gene expression in the tumors with 1q gain versus the others. H Scatterplot showing the Spearman’s correlation coefficient and p-value (two-sided) of the CIN score versus the ssGSEA score of mitochondrion gene set (95% CI for the regression band), n = 163. I The histochemistry scores (H-scores) of ATP5A1 (n = 5) and TOMM20 (n = 3) between tumors with 1q gain and tumors with 1q WT (Student’s t-test, two-sided, mean ± SEM). J Scatterplot showing the Spearman’s correlation coefficients (two-sided) of mitochondrial gene set scores versus 1q copy number (x axis, n = 163) and the associations with prognosis (y axis, n = 119). K Heatmap of representative significant cis- and trans-event genes associated with 1q gain in SBC. L Scatterplot showing the p-values for PFS (x-axis, n = 106) and the Spearman’s correlation coefficients (two-sided) of the metabolism-related pathways(n = 187). M A model depicting the multi-level regulation of chromosome 1q copy number alteration.
To identify potential drivers of SBC on chromosome 1q and to define the downstream signaling pathways directly affected by 1q gain, we screened genes located on chromosome 1q that positively correlated with 1q copy number, i.e., cis event genes (Spearman’s correlation, r > 0.2, p < 0.05) (Fig. 3E; Supplementary Data 4). These cis event genes were mostly enriched in mitochondrion-related pathways, including mitochondrion, mitochondrial matrix, and mitochondrial translation (Fig. 3F; Supplementary Data 4). Tumors with 1q gain exhibited significant enrichment of genes involved in mitochondrial gene expression (Fig. 3G, FDR = 0.0058), and the ssGSEA score for mitochondrion gene set were higher in these tumors with 1q gain than in tumors without 1q gain (Supplementary Fig. 7E, Wilcoxon sum-rank test, p < 0.001). Moreover, the ssGSEA score for the mitochondrion gene set also showed positive correlation with CIN score (Fig. 3H, Spearman’s correlation, r = 0.34, p = 7.6e-06). In addition, the expression levels of cis event genes involved in mitochondrial pathways, such as TARS2, DARS2, MRPL24, MRPL9 and MRPS21, were significantly upregulated in 1q gain tumors compared with those in 1q WT tumors or 1q WT/loss tumors (Supplementary Fig. 7F), and these proteins were associated with worse prognosis in the SBC cohort (Supplementary Fig. 7F). Consistent with the increase in mitochondria and related proteins, gene sets enriched for essential mitochondrial functional pathways, including fatty acid oxidation, oxidative phosphorylation, reactive oxygen species (ROS), glutathione metabolism and tricarboxylic acid (TCA) cycle pathways, were also significantly upregulated in tumors with 1q gain (Supplementary Fig. 7G, Wilcoxon rank-sum test, p < 0.05). These results suggested that mitochondria were upregulated in 1q gain tumors. This finding was further supported by IHC for ATP5A1, which is a mitochondrial marker66, and TOMM20, which is a classic mitochondrial membrane matrix marker related to several tumor-associated mitochondrial changes that can be used to assess the overall stability of mitochondrial health67. The H-score of ATP5A1 and TOMM20 were significantly upregulated in tumors with 1q gain (Fig. 3I and Supplementary Fig. 7H, ATP5A1: Student’s t-test, p = 0.0117; TOMM20: Student’s t-test, p = 0.0171). These results demonstrated that the expression level of mitochondrial translation related genes was increased in 1q gain samples, indicating the influence of 1q gain SBC on mitochondrial function.
To further investigate the dominant functional processes in mitochondria that are upregulated by 1q gain and may lead to poor prognosis, we used ssGSEA to calculate the scores of all mitochondrial pathways identified in previously reported MitoCarta3.0 datasets68 for each sample (Supplementary Data 4). We screened all mitochondrial pathways in the MitoCarta3.0 dataset for their associations with 1q chromosome gain and assessed their impacts on the prognosis of patients with 1q gain. Among these mitochondrial pathways, we discovered that mitochondrial protein homeostasis not only showed a significant positive correlation with the copy number of 1q but also exhibited the strongest association with patients’ worse PFS (Fig. 3J; Log-rank test, r = 0.3, p = 3.06e-06). Based on these findings, we hypothesized that the mitochondrial protein homeostasis pathway might contribute to inferior prognosis in patients with 1q gain. The mitochondrial protein homeostasis pathway is one of the overall mitochondrial quality control pathways that plays a central role in maintaining the functional integrity of mitochondria69. The mitochondrial protein hemostasis genes, such as HSP family genes, ensured that the appropriate folding and assembly of proteins was present in the mitochondria for maintaining their normal functions70. We acknowledged that there might be other mitochondria quality control pathways related to 1q gain event, such as mitophagy. Actually, all these mitochondrial pathways were concluded in the MitoCarta dataset68,71. The mitochondrial protein homeostasis pathway was more significantly correlated with both 1q gain and PFS compared with other mitochondrial pathways (Fig. 3J), suggesting that protein homeostasis pathway might be more related to the worse prognosis of 1q gain SBC than other mitochondrial pathways. Overall, among all upregulated pathways in 1q gain tumors, the protein homeostasis pathway showed the most significant correlation with PFS (Fig. 3J); both mRNA and protein levels of related proteins, such as HSPD1, HSPE1, and DNAJA372, were significantly upregulated in these 1q gain tumors, and associated with inferior prognosis (Fig. 3K and Supplementary Fig. 7I). To further validate the function of these three proteins in chordoma cell survival, we generated siRNA-induced HSPD1, HSPE1 and DNAJA3 knockdown (KD) SBC cell lines (Methods). WB was conducted on the knockdown cells and control cells to evaluate the protein expression levels of HSPD1 (12165S, 1:1000; Cell Signaling Technology), HSPE1 (abs146058, 1:1000; Absin), and DNAJA3 (11088-1-AP, 1:1000; Proteintech). The protein expression levels of HSPD1, HSPE1, and DNAJA3 were lower in the KD cells compared with in the control cells (Supplementary Fig. 8A). We also observed significantly decreased cell proliferation in the three KD cell lines than in the control cells (Supplementary Fig. 8B). Additionally, to validate that the upregulation of mitochondrial functions was modulated by 1q gain in SBC, we induced CIN in SBC cell line and screen for the SBC cells displaying 1q gain. To obtain cells with 1q gain, SBC cells were treated with the cytarabine73 to induce CIN and chromosome CNAs (Methods). The Cytarabine-treated cells and the control cells were detected by WES analysis and FISH analysis to identify chromosome CNAs and screen for 1q gain (Methods). As a result, we selected monoclonal SBC cells displaying the 1q gain event among treated cells for further validation. Our proteomic data of 1q gain cells and control cells showed that the scores of mitochondrial gene expression and protein homeostasis gene sets were significantly upregulated in 1q gain SBC cells compared with control cells, and the expression levels of MRPL24, MRPL21 and TARS2 were also significantly higher in 1q gain SBC cells (Supplementary Fig. 8C). WB analysis also revealed that the expression levels of HSPD1 protein and TOMM20 protein were increased in the 1q gain cells compared with the control cells (Supplementary Fig. 8D). These collective data indicated that 1q gain might increase mitochondrial translation related genes, and potentially led to aberrantly high expression of protein homeostasis genes, such as DNAJA3, HSPE1 and HSPD1, which were related to worse prognosis for SBC patients.
Tumor cells exhibited increased metabolic demands and rely on efficient mitochondrial functions to support their high energy requirements74. Thus, we calculated the GSEA scores of all the pathways associated with metabolism in each sample based on the human MitoCarta3.0 dataset68. Then, we compared the differences of these metabolic pathways between SBC tumors with 1q gain and tumors without 1q gain. Among them, we observed that pathways involved in multiple metabolic functions, including amino acid metabolism, carbohydrate metabolism, detoxification, lipid metabolism, metals and cofactors, and vitamin metabolism pathways, were significantly upregulated in SBCs with 1q gain (Supplementary Fig. 9A). Moreover, we surveyed the correlations between the protein homeostasis pathway and all the mitochondrial metabolic pathways. The correlation results showed that the protein homeostasis pathway was positively correlated with metabolic pathways, such as amino acid metabolism (Spearman’s correlation, r = 0.65, p = 1.34E-20), malate aspartate shuttle (Spearman’s correlation, r = 0.62, p = 8.98E-19), lipid metabolism (Spearman’s correlation, r = 0.58, p = 2.95E-16), and pyruvate metabolism (Spearman’s correlation, r = 0.53, p = 2.37E-13) (Supplementary Fig. 9B). Additionally, the higher expression levels of several metabolic pathways, such as malate aspartate shuttle (Log-rank test, p = 2.1E-04), pyruvate metabolism (Log-rank test, p = 2.9E-04) and amino acid metabolism (Log-rank test, p = 3.8E-04) pathways, indicated worse prognosis in SBC patients (Supplementary Fig. 9C), which was consistent with the previous findings in other cancers that the metabolism played an essential role of tumor growth and progression75. Moreover, in order to find the key metabolic pathway connected with both protein homeostasis and poor prognosis, we screened the correlations between these metabolic pathways and protein homeostasis pathway and the associations of these metabolic pathways with PFS. The result revealed that the amino acid pathway showed the strongest correlation with the protein homeostasis pathway, and was associated with worse PFS in SBC patients (Fig. 3L). Among all the genes involved in amino acid metabolism pathways, SHMT2 was highly correlated with protein homeostasis (Supplementary Fig. 9D). Moreover, SBC patients with higher expression level of SHMT2 had significantly shorter PFS (Supplementary Fig. 9E), suggesting that SHMT2 was related to the worse prognosis in 1q gain SBC patients. SHMT2 is the key enzyme involved in amino acid metabolism, and is essential for tumor cell growth and viability in Burkitt lymphoma76. These results suggested that protein homeostasis-related genes upregulated in SBCs with 1q gain might contribute to the enhanced mitochondrial metabolic functions observed in these 1q gain SBC tumors, thereby providing an advantage for adaptation to the tumor microenvironment and enable the rewiring of metabolic pathways to sustain tumor proliferation (Fig. 3M).
RPRD1B expression predicts the response to radiotherapy in SBC
A primary cause of poor prognosis in chordomas is resistance to radiotherapy77. To identify potential biomarkers and downstream mechanisms of radio-resistance, we focused on the multi-omics data from patients with long-term post-radiotherapy follow-up. Among the 91 patients who received radiotherapy, pre-radiotherapy samples were available in 73 of them. To identify potential mechanisms underlying radiotherapy treatment resistance, and avoid bias introduced by radio therapy78,79, the pre-radiotherapy tumor samples (n = 73) obtained from SBC patients before they underwent radiotherapy (Supplementary Fig. 10A) were collected. We divided these tumors (n = 73) into radio-resistant (n = 26) and radio-sensitive groups (n = 47) based on whether patients relapsed within the median 3 year follow-up (Supplementary Fig. 10B). Each group was further divided into high-dose or low-dose subgroups depending on their treatment (high-dose > 60 Gy, low-dose < 60 Gy; Fig. 4A, Methods). Thus, the pre-radiotherapy tumors were divided into four groups based on both the response to radiotherapy and dosage of radiation: low-dose radio-sensitive (n = 26), high-dose radio-sensitive (n = 21), low-dose radio-resistant (n = 19) and high-dose radio-resistant (n = 7) subgroups (Supplementary Fig. 10B).
A Heatmap of differentially regulated (FDR < 0.05, log2FC > 0.3) DNA repair-related proteins between radio-resistant (n = 26) and radio-sensitive groups (n = 47). B CIN scores among high-dose resistant (n = 7), low-dose resistant (n = 19), high-dose sensitive (n = 21), and low-dose sensitive (n = 26) groups. C Proteins significantly correlated with both radio-resistance degree and CIN score, n = 96. D Protein expression levels of RPRD1B among high-dose resistant (n = 7), low-dose resistant (n = 19), high-dose sensitive (n = 21), and low-dose sensitive (n = 26) groups. E, F Chordoma cell viability assays with knockdown of RPRD1B or/and exposure to 32 Gy (E) or 64 Gy (F) of irradiation. Scrambled siRNA: treated with 32 Gy or 64 Gy of irradiation. A: treated with 32 Gy or 64 Gy of irradiation and RPRD1B siRNA1-knockdown. B: treated with irradiation and RPRD1B siRNA2-knockdown. C: treated with RPRD1B siRNA1-knockdown. D: treated with RPRD1B siRNA2-knockdown (n = 6 for each group, biological replicates; mean ± SEM; Student’s t-test, two-sided). G HDR and MMR pathways significantly correlated with CIN score and RPRD1B. H Heatmap showing the copy number/mRNA/proteins/phosphoproteins levels of HDR and MMR related genes (top panel), the ssGSEA score of cell cycle pathway, and the radio-resistance degree (bottom panel), n = 96. I ssGSEA scores of HDR, MMR, G1 phase and S phase, n = 96. J Correlations of cell cycle-related proteins with HDR and MMR, n = 96. K Heatmap showing abundance/kinase activities of MCM2 phosphoprotein, MCM2_S27, CSNK2A1, CDK7, CDK2 and CDC7, n = 96. L A brief model depicting the G1 and S phase genes most affected by CIN score, HDR and MMR (n = 96). The p-values in (C) and (G–K) were calculated by Spearman’s correlation test (two sided). For boxplots in (B) and (D) the middle bar represents the median, and the box represents the interquartile range; bars extend to 1.5 × the interquartile range. Anova and Kruskal−Wallis test were used for comparisons among four groups, Wilcoxon rank-sum test were used for comparisons between two groups. n.s., not significant; *p < 0.05; **p < 0.01; ***p < 0.001.
Radiotherapy is an important cancer treatment strategy that causes DNA damage in tumor cells either directly or indirectly, which prevented tumor cells from dividing and surviving80. DNA repair played a crucial role in maintaining genomic stability by repairing DNA damage induced by radiation from radiotherapy in the development of radiotherapy resistance in cancer81. Thus, we focused on the observation that DNA repair was significantly upregulated in pre-radiotherapy tumors from radiotherapy-resistant patients. We then investigated the differential pathways among different radio-therapy degrees using proteomic data. The result showed that the DNA repair pathway score inferred by proteomic data were significantly upregulated in higher radio therapy degrees compared with low-dose radio-sensitive tumors (Supplementary Fig. 10C, Anova, p = 0.0084). We also surveyed all the proteins related to DNA repair process. There were significant differences in the expression of proteins related to radio-resistance (log2FC > 0.3, FDR < 0.05), including CUL4A, HMGB1, PRKDC, RPRD1B and ATM (Fig. 4A). These results suggested that DNA repair pathway and its associated proteins were significantly upregulated in tumors that were sensitive to radiotherapy, consistent with our original findings. Examination of dose response showed that CIN scores were higher in both the high-dose and low-dose resistant groups than in the low-dose radio-sensitive subgroup (Wilcoxon rank-sum test, high-dose resistant versus low-dose sensitive, p = 0.032; low-dose resistant versus low-dose sensitive, p = 0.048) (Fig. 4B). The proportion of CIN+ and CIN- tumors among the four subtypes is significantly different, in which low-dose radio-sensitive subgroup have a lower proportion of CIN+ SBCs (Supplementary Fig. 10D, Chi-square for trend, p = 0.0405). Based on our follow-up data, we observed a higher proportion of recurrences in CIN+ tumors that received lower dose radiotherapy compared to CIN- tumors treated with higher doses (recurrences in CIN- tumors treated with low-dose radiotherapy: 40.7%; recurrences in CIN- tumors treated with high-dose radiotherapy: 20.3%). Therefore, it can be reasonably inferred that CIN- cohorts treated with higher doses of radio therapy might have a better chance of not relapsing. Several previous studies suggested that administering higher doses of radiotherapy could effectively target and eliminate residual tumor cells, thereby enhancing treatment outcomes and reducing the likelihood of recurrence82,83, which was consistent with our assumption.
Since these findings suggested that the degree of radio-resistance might be related to CIN status, we next conducted correlation analysis, which identified 204 proteins significantly positively correlated with degree of radio-resistance, and 1132 proteins significantly positively correlated with CIN score (Supplementary Fig. 10E, F; Supplementary Data 5). Among them, RPRD1B was significantly correlated with both radio-resistance degree and CIN score (Fig. 4C; Supplementary Data 5), and RPRD1B protein expression was higher in both the high- and low-dose radio-resistant groups compared to the low-dose radio-sensitive group (Wilcoxon rank-sum test, p = 0.0015) (Fig. 4D). Overall, we compared the protein expression differences in pre-radiotherapy tumor samples from patients with varying degrees of response to radiotherapy and observed a significant upregulation of the DNA repair pathway and RPRD1B in the group with the higher degree of radiotherapy resistance (Fig. 4D and Supplementary Fig. 10C). Based on these findings, we proposed that the elevated expression of the DNA repair pathway and RPRD1B might be potential causes of radiotherapy resistance in SBC patients. To demonstrate this assumption, we explored the expression patterns of DNA repair pathway and RPRD1B protein in matched tumor samples collected before and after radiotherapy from the same SBC patients. The results showed that DNA repair pathway-related proteins and RPRD1B were not significantly upregulated in post-radiotherapy samples (Supplementary Fig. 10G, H), which supported our hypothesis that the observed differences might be potential causes and markers of radiotherapy resistance rather than the consequences of radiotherapy.
To further determine whether RPRD1B expression indeed functionally contributed to response to radiotherapy, we silenced RPRD1B in the SBC cell line using siRNA and assessed sensitivity to radiotherapy in vitro. After Western blot confirmation of RPRD1B suppression (Supplementary Fig. 10D), cell viability assays in RPRD1B-silenced and control cells treated with 32 or 64 Gy indicated that cell viability/survival was significantly reduced compared to controls (p < 0.05) (Fig. 4E, F; Supplementary Data 5). Examination of tumor recurrence and patient survival indicated that primary patients (n = 119) with higher RPRD1B expression appeared to have significantly worse OS and PFS (Supplementary Fig. 10I, J). Moreover, the CIN status of the RPRD1B knockdown cells and the control cells were analyzed based on WES data and were validated through FISH analysis (Methods). Analysis of the WES data revealed that the CIN score of the RPRD1B knockdown cells was significantly lower compared with that of the control cells (Supplementary Fig. 11A and 11B). To validate these findings, FISH analysis was performed using the GSP 1q21/1q36 probe to detect 1q copy number alterations in RPRD1B knockdown cells and the control cells (Methods). The FISH results demonstrated a significant decrease in the level of 1q gain in RPRD1B knockdown cells (Supplementary Fig. 11C). Based on our cell counting analysis, we observed that 38% of the randomly counted RPRD1B knockdown cells showed positive 1q gain, while 70% of the control cells were 1q gain positive (Supplementary Fig. 11D). Taken together, our findings indicated that the knockdown of RPRD1B resulted in a slightly lower CIN status, as evidenced by the reduced level of 1q gain compared to the control cells. Further investigation was needed to elucidate the role of RPRD1B in CIN.
Further exploration of the role of RPRD1B through GSEA indicated that proteins significantly correlated with RPRD1B were enriched in the DNA repair pathway (Supplementary Fig. 11E; Supplementary Data 5). Calculation of ssGSEA scores for a set of 276 proteins reportedly involved in 10 major DNA repair pathways84 revealed that homology-dependent recombination (HDR) and mismatch repair (MMR) pathways were significantly correlated with CIN score and RPRD1B levels in our datasets (Fig. 4G; Supplementary Data 5). In light of these findings, we proposed that RPRD1B could be an upstream regulator of the HDR and MMR DNA repair pathways, which aligned with previous studies in other cancers85. In our datasets, HDR-related proteins, including PARP1, RECQL, BARD1, RPA1/2/3, PALB2 and XRCC284, and MMR-related proteins, such as MSH2, MSH6, MSH3, and PMS1/284 were significantly positively correlated with CIN score (Fig. 4H; Supplementary Data 5), which agreed with previous work showing that RPRD1B was involved in DNA damage repair via interacting with RPA1/2/386, and in MMR via interaction with MSH287. In addition, we treated SBC cell line (UM-Chor1) with cytarabine to induce CIN and achieved monoclonal CIN+ cells (Methods). Subsequently, we analyzed the proteomic data and found a significant increase in RPRD1B expression in the CIN+ cells compared to the control (Supplementary Fig. 11F). To further validate this finding, we performed WB analysis of the expression level of RPRD1B in CIN+ cells and the control. The results demonstrated a significant upregulation of RPRD1B expression in CIN+ cells compared to the control (Supplementary Fig. 11G and 11H, Student’s t-test, p = 0.0047). These results indicated that RPRD1B expression was significantly upregulated in induced CIN+ cells compared to the control cells, supporting the hypothesis that CIN might lead to an upregulation of RPRD1B expression. These results together suggested that CIN leads to increased RPRD1B expression to promote DNA repair pathway, especially HDR and MMR pathways in radio-resistant SBCs.
In addition, the ssGSEA scores for the cell cycle gene set were significantly positively correlated with CIN score (Spearman’s correlation, r = 0.28, p = 0.023) (Supplementary Fig. 11I; Supplementary Data 5), with the highest score in the high-dose resistant group (Wilcoxon test, p = 0.0056) (Supplementary Fig. 11J). Moreover, cell cycle-related proteins were all significantly positively correlated with CIN score, including PCNA, replication factor C (RFC), DNA Pol δ1, DNA Pol δ2, DNA Pol δ4, and DNA ligase 1 or DNA ligase 3 (Fig. 4H; Supplementary Data 5), which is reasonable given their function in the final step of DNA gap filling synthesis and ligation. Correlation analysis indicated that HDR and MMR were significantly positively correlated with the cell cycle pathway (Supplementary Fig. 11K), suggesting that radio-resistant tumors continued to proliferate despite the high degree of CIN. This phenomenon led to hypothesize that CIN might activate RPRD1B expression, consequently promoting cell cycle progression, ultimately leading to radio-resistance.
We next used correlation analysis to explore which specific phase of the cell cycle was affected by the HDR and MMR pathways and found that mRNA and protein pathway scores of the G1 and S phases were significantly correlated with CIN score, HDR, and MMR (Fig. 4I; Supplementary Data 5), with the S phase having the strongest correlations (Fig. 4I, J; Supplementary Data 5). Since MCM2 phosphorylation is well-established to promote cell cycle progression, we examined phosphoproteomic data for MCM2, which revealed a significant association between its phosphorylation and HDR (Fig. 4K). Notably, among all MCM2 phosphorylation sites, MCM2_S27 had the strongest correlation with HDR (Fig. 4K). Using substrate phosphorylation levels to infer kinase activities (Methods) implied that CDC7 kinase activity had the highest correlation with MCM2_S27 phosphorylation (Fig. 4K), which aligned well the reported function of CDC7 in activating MCM complex during S phase (Fig. 4L)88. These results together suggested that increased RPRD1B expression, promoting HDR and MMR pathways, potentially resulting in radio-resistance in CIN+ SBCs.
Immune-cold SBCs associated with 9p and 10q losses
To investigate possible roles of the tumor immune microenvironment in SBC, we performed cell type deconvolution analysis with RNA-seq data using xCell89 to infer the relative abundance of different cell types in the tumor microenvironment (Fig. 5A; Supplementary Data 6; Methods). xCell is a computational tool used for quantitative analysis of cell types in tumor tissues or other complex tissues, which was built based on a large amount of transcriptome data collected from various types of cells. Consensus clustering based on inferred immune cell proportions identified three sets of tumors with distinct immune and stromal features: Hot, Cold, and Mix (Fig. 5A, B; Supplementary Data 6). Less immune cell proportions were observed in the Cold subtype (Fig. 5A; Supplementary Data 6), which had a higher CIN score (Supplementary Fig. 12A) and CIN + proportion than the other two subtypes (Supplementary Fig. 12B). Correspondingly, several immune-related pathways, including IL6/JAK/STAT3 signaling, interferon-gamma response, and complement pathways, and key immune cell surface proteins, such as CD3D/E/G, CD8A/B, CD274, PDCD1, and TIGIT, were significantly downregulated in Cold subtype tumors in our dataset (Fig. 5A; Supplementary Data 6). The proteomic results showed that the expression levels of several important immune related proteins, such as CD3D, CD3E, CD3G, CD8A, CD163, PDCD1LG2, TNF, TNFSF10, CXCL10, FASLG, GZMK, HLA-DRA, HLA-DRB1, HLA-DPB1, VWF and ZAP70, were also significantly upregulated in Hot immune subtype (Fig. 5A). The tumor purity of SBCs was not significantly differed among three immune subtypes (Supplementary Fig. 12C). The IHC results of SBC specimens further demonstrated that the expression level of CD3E was downregulated in CIN+ SBCs compared to CIN- SBCs (Supplementary Fig. 12D).
A Heatmap illustrating cell type compositions and abundance of selected key genes/proteins and pathways across the three immune subtypes. The heatmap in the first section illustrates the immune/stromal signatures from xCell (n = 180). The mRNA and protein abundance of key immune-related markers and ssGSEA scores of common pathways and protein-only pathways upregulated in different immune subtypes are illustrated in the remaining sections. B Contour plot of two-dimensional density based on stromal core (y-axis) and immune scores (x-axis) for different immune subtypes. C Kaplan-Meier curve of PFS for six subgroups based on the CIN status (p-value from log-rank test). Hot CIN- = 32, Hot CIN + = 26, Cold CIN- = 16,Cold CIN + = 45, Mix CIIN- = 28, and Mix CIN + = 14. D The scatter plot illustrating the correlation between arm-level copy number and CIN score (x-axis, n = 163), as well as immune score (y-axis, n = 161). E Chromosome arms significantly correlated with immune scores and CIN scores (n = 161). F GSEA plot showing the chromosome 9p had significant positive correlation with inflammatory response and IL6/JAK/STAT3 signaling based on proteomic data (n = 163). G GSEA plot showing chromosome 10q had significant positive correlation with TNF-α signaling via NF-KB and interferon (IFN) alpha response based on proteomic data (n = 163). H Heatmap of copy number loss of chromosomes 9p and the copy number(CN)/mRNA/protein abundance of key interferon receptors genes, IL6/JAK/STAT signaling pathway genes and key immune checkpoints (n = 163). I Heatmap of copy number loss of chromosomes 10q and the copy number(CN)/mRNA/protein abundance of NF-KB related genes and key cytokines (n = 163). J A brief model depicting that combined effect of 9p loss and 10q loss enabled CIN + tumors to escape the immune surveillance. The p-values in (D–F) and (I) were calculated using Spearman’s correlation (two-sided).
To further elucidate the association between immune subtypes and CIN, we divided three immune subtypes into six subgroups according to CIN+ or CIN- status. Clinically, PFS was significantly worse in CIN+ subgroups of the Hot, Cold and Mix tumors, compared to that in corresponding CIN- tumors (Fig. 5C; Supplementary Data 1). Moreover, CIN score was significantly negatively correlated with immune score (Spearman’s correlation, r = −0.42, p = 2.7e-08, Fig. 5D), which was in contrast to the findings observed in other tumors that CIN could activate immune response through the cGAS-STING pathway90,91,92. The cGAS-STING pathway and its key genes were not upregulated in CIN+ SBCs (Supplementary Fig. 12E; Supplementary Data 6). To identify a possible genetic basis underlying reason, correlation analysis with chromosome arm copy number revealed that both immune score and CIN score significantly correlated with chromosome 10q and 9p arm-level copy numbers (Fig. 5E; Supplementary Data 6), indicating that losses of 9p and 10q were associated with immune suppression microenvironment in CIN + SBC tumors.
To better understand how losses of 9p and 10q contributes to immunosuppression in SBC, we performed Spearman’s correlation between expression levels of immune-related genes and 10q/9p copy number (Supplementary Fig. 10F and 12G). Based on the proteomic data, the GSEA results indicated that 9p shared a significant positive correlation with expression of inflammatory response (NES = 1.9, FDR = 0.0186) and IL6/JAK/STAT3 signaling gene sets (NES = 2.3, FDR = 0.003, Fig. 5F; Supplementary Data 6), whereas 10q was positively correlated with TNF-α signaling via NF-kB (NES = 2.1, FDR = 1.6e-6) and interferon (IFN) alpha response gene sets (NES = 1.6, FDR = 0.0286) (Fig. 5G; Supplementary Data 6). The transcriptomic results also showed that the inflammatory response and IL6/JAK/STAT3 pathways were downregulated in 9p loss tumors, and the TNFA signaling via NFkB and interferon alpha signaling pathways were downregulated in 10q loss tumors at both proteomic and transcriptomic levels (Fig. 5F and G, Supplementary Fig. 12H), suggesting that the alterations of immune processes at the protein expression levels were consistent with transcriptomic data. The integration of both RNA-seq and proteome data suggested that the differences of these pathways can be transitioned from transcriptome to proteome, and could be used to comprehensively evaluate the expression levels of the genes of interest. Specifically, copy number of 9p21.3 was positively correlated with mRNA levels of several IFN genes located on this region and IL6/JAK/STAT signaling gene (i.e. JAK2) located on 9p, which also associated with deficiencies in other IFN signaling genes and immune checkpoint genes (Fig. 5H; Supplementary Data 6), suggesting the reduced immune response consistent with previous reports of tumor immune escape via IFN pathway downregulation associated with 9p loss93. Additionally, our above GSEA results suggested that 10q loss could downregulate NF-kB signaling and IFN signaling, since the central pro-inflammatory activators NFKB2 and CHUK94, which are located on 10q, were decreased in 10q loss SBCs (Fig. 5I; Supplementary Data 6). NFKB2 can promote the expression of other cytokines, such as CCL2/4/5/7/8 and CXCL10/12/2/5/995, which were also downregulated in 10q loss SBCs (Fig. 5I; Supplementary Data 6). Consisting with these findings, IHC analysis showed that expression level of NFKB1 and NFKB2 were significantly lower in 10q loss SBCs (Supplementary Fig. 12I). Next, we treated SBC cells with the cytarabine to manually induce random CNAs in the SBC cells as mentioned above (Methods). Then, WES analysis and FISH analysis were introduced to screen for the 9p loss and the 10q loss cell lines (Methods). As a result, SBC cells displaying 10q loss were used for the following analysis. The proteomic data demonstrated that 10q loss SBC cells showed significantly lower expression levels of TNFA signaling via NFKB and inflammatory response pathways compared with SBC control cells (Supplementary Fig. 12J and K). These findings indicated that 9p and 10q losses might drive immune evasion in CIN+ tumors by affecting immune-related pathways including IFN signaling and NF-kB signaling pathways, suggesting that immune checkpoint inhibitor (ICI) therapy could be effective in CIN- SBCs rather than CIN+ SBCs (Fig. 5J). In addition, we performed FISH analysis using GSP 9p21/ CSP 9 probe and GSP 10q23/ CSP 10 probe27,28,29 to assess chromosome 9p and 10q loss in corresponding samples, respectively, to validate samples that had 9p loss or 10q loss. The samples that had WT 9p/10q were used as a reference for comparison in our analysis. Two hundred non-overlapping tumor nuclei were evaluated for each sample. The analysis revealed that the percentage of cells with 9p loss in sample with 9p loss was 81%, significantly higher than that in the control sample (5%). Similarly, the percentage of cells with 10q loss in sample with 10q loss was 77%, which was notably higher than that in the control sample (6%). These FISH results verified the 9p loss or 10q loss identified based on WES data (Supplementary Fig. 12L).
In order to further validate our findings and strengthen the mechanistic understanding of immune evasion in SBC, we conducted additional in vitro experiments. Firstly, we achieved two monoclonal CIN+ cells with 9p loss and 10q loss, respectively (Methods). Moreover, to assess the impact of 9p loss and 10q loss events on the antitumor immune response, we co-cultured the 9p loss and 10q loss SBC cell lines with T cells for a period of 2 weeks, separately. Following the co-culture, we measured the levels of interferon (IFN) produced by the treated CIN+ cells compared to control cells. The results clearly demonstrated a significant decrease in IFN levels in the 9p loss and 10q loss cells (Supplementary Fig. 13A). Furthermore, we evaluated the cytotoxicity of T cells against these CIN+ cells using a CellTiter-Glo Luminescent Cell Viability Assay (Methods). Our findings showed a notable decrease in cytotoxicity against the 9p loss and 10q loss cells (Supplementary Fig. 13B), providing evidence of reduced immune-mediated killing capacity. To investigate the potential of immune checkpoint blockade, we treated the co-cultured cells (SBC cells and T cells) with atezolizumab, a PD-L1 inhibitor commonly used in immunotherapy. The concentration of atezolizumab used was 10 µg/ml, and the treatment duration was 24 h96. We observed a more significant decrease in survival rates in the 9p loss and 10q loss cells compared to control cells following atezolizumab treatment (Supplementary Fig. 13C). These findings suggested that the 9p/10q loss-SBC cells might upregulate PD-L1 as a mechanism to inhibit tumor immunity, which could help explain the poor response to immunotherapy reported in previous studies97,98. Our results provided a potential mechanism for the lack of immune response in SBC patients, which might be attributed to the 9p and 10q losses observed in these individuals.
Proteomic subtypes of SBC
Since no proteomic subtyping of SBC has been reported to date, we sought to classify SBC tumors based on differential protein accumulation to guide clinical prognostic prediction. To this end, we performed consensus clustering based on transcriptomic and proteomic data (Supplementary Fig. 14A and 14B; Methods), which identified four proteomic subtypes among the 187 tumors based on the top 30% most variable proteins (Supplementary Fig. 14A; Methods). These groups were designated P-I (n = 54), P-II (n = 38), P-III (n = 50) and P-IV (n = 45) based on their distinct proteomic profiles and clinical features (Fig. 6A, B; Supplementary Data 7), while transcriptomic clustering was used to classify 180 SBCs into the R-I (n = 53), R-II (n = 77), and R-III (n = 50) subtypes (Supplementary Fig. 14B). In Fig. 6A, the heatmap (upper) showed chromosome arm events, clinical information, different subtypes classification, and the heatmap (below) showed significantly upregulated proteins in each protein subtype. Samples and proteins are displayed as columns and rows, respectively. Subsequent integrated analysis of proteomic and transcriptomic subtypes indicated that the R-II subtype, which predominantly consisted of CIN+ tumors, contained both P-II and P-III subtypes (Supplementary Fig. 14C), suggesting finer resolution of SBC subtypes based on proteomic classification. P-II and P-III subtypes had significantly higher CIN score than P-I and P-IV subtypes (Fig. 6C). Further, ssGSEA analysis exploring differences in molecular features among proteomic subtypes (Fig. 6B; Supplementary Data 7). We observed that the P-I subtype exhibited the highest levels of ECM-related proteins, including those involved in focal adhesion, ECM-receptor interaction, and angiogenesis pathways (Fig. 6B). The higher CIN subtypes (P-II and P-III subtypes) showed upregulation of MYC targets, E2F targets, oxidative phosphorylation, PI3K-AKT-mTOR signaling and DNA replication pathways compared with lower CIN subtypes (P-I and P-IV), further validating correlations between CIN+ features and increased levels of progression-associated processes (Fig. 2A). By contrast, the P-IV subtype had increased protein levels associated with metabolism-related pathways, such as pyruvate metabolism and N-glycan biosynthesis. Evaluation of immune scores in xCell revealed significant differences among the four subgroups, with the lowest immune score found in the Cold tumor-enriched P-II subtype (Fig. 6D, E), suggesting that P-II tumors might be unresponsive to ICI.
A Heatmap illustrating the characterizations of four proteomic subtypes (Kruskal–Wallis test), annotated with clinical features (Fisher’s exact test), n = 187. Fisher’s exact test was used for categorical variables. B Pathways significantly enriched in the proteomic subtypes (FDR < 0.05). C, D Boxplots illustrating CIN score (C) and immune score (D) across proteomic subtypes (Wilcoxon rank-sum test used for comparisons between two subtypes, Anova test and Kruskal–Wallis test used for comparisons among four subtypes; P-I: n = 54; P-II: n = 38; P-III: n = 50; P-IV: n = 45). E Heatmap illustrating the overlap of immune clusters with proteomic subtypes. F, G Survival Kaplan–Meier curves showing (F) OS and (G) PFS of primary tumors within the four proteomic subtypes (log-rank test). P-I = 40, P-II = 19, P-III = 31, and P-IV = 31. H Heatmap of PROGENy pathway scores between P-II and P-III subtypes (Wilcoxon rank-sum test). The p-value is displayed in asterisks. I Boxplot showing lower TRAIL pathway score in P-II subtype compared with P-III subtype (Wilcoxon rank-sum test; P-II: n = 38, P-III: n = 50). J Boxplot showing lower IRF1 TF activity score in P-II subtype compared with P-III subtype (Wilcoxon rank-sum test; P-II: n = 38; P-III: n = 50). K Scatterplot showing the Spearman’s correlation (two-sided) of the IRF1 TF activity score versus TRAIL pathway score, n = 180. L Heatmap showing representative TRAIL pathway related genes significantly downregulated in P-II subtype compared with P-III subtype. M Plot showing qPCR result of IRF1 gene between the IRF1 KD cells and the control cells (n = 2 for each group, biological replicates). N Boxplot showing apoptosis pathway score between the IRF1 KD cells and the control cells (Paired t-test, two-sided; n = 3 for each group, biological replicates). For boxplot in (C, D, I, J, and N) the middle bar represents the median, and the box represents the interquartile range; bars extend to 1.5 × the interquartile range.
Comparison of clinical data from primary patients of each proteomic subtypes showed that patients with higher CIN score subtypes (P-II and P-III) had worse PFS than those with lower CIN score subtypes (P-I and P-IV) (log-rank test, p = 0.0161; Fig. 6F), which was consistent with the observed association between worse PFS and higher CIN scores in this SBC cohort (Fig. 1H). The analysis using clinical data from all patients of each proteomic subtypes also indicated that P-II and P-III subtypes had worse PFS than P-I and P-IV subtypes (Supplementary Fig. 14D).
P-I subtype featured with ECM-related pathways had relatively better prognosis than P-II and P-III subtypes (Fig. 6B, F, and G). In our study, we found that ECM receptor interaction, focal adhesion, and angiogenesis pathways were significantly upregulated in P-I subtype compared to other subtypes (Supplementary Fig. 15A–C, Kruskal−Wallis, p < 2.2e-16, p = 3.8e-09, p = 1.6e-12). Furthermore, we observed that higher expression levels of these pathways were associated with improved patient outcomes (Supplementary Fig. 15D–F). These findings indicated that upregulated ECM-related pathways were associated with favourable outcomes in SBC. Along with these findings, proteins enriched in ECM-related pathways such as ADAM8, AGER, ICAM1 and ITGA4, etc. were observed to show significantly elevated expression in P-I (Supplementary Fig. 15G). Further survival analysis revealed the increased expression of ADAM8, AGER, ICAM1 and ITGA4 were associated with prolonged overall survivals (log-rank test, p-value < 0.05, Supplementary Fig. 15H). Taken together, our study provided insights into the associations between upregulated ECM-related pathways and the better prognosis in the P-I subtype. The upregulation of these pathways might contribute to the better prognosis observed for the P-I subtype relative to the P-II and P-III subtypes, indicating the importance of further research and therapeutic development focused on ECM-related pathways in SBC.
The P-IV subtype, which was enriched with metabolism-related pathways, also showed relatively better prognosis compared with higher CIN score subtypes (P-II and P-III subtypes) (Fig. 6B, F, and G). the metabolism-related pathway, such as N-glycan biosynthesis (Kruskal−Wallis, p = 9.4e-06) and pyruvate metabolism (Kruskal−Wallis, p = 0.016) were significantly upregulated in P-IV subtype compared with other subtypes (Supplementary Fig. 15I, J). Similarly, we screened the previous studies regarding metabolism-related pathways and tumor prognosis. It is reported that metabolic pathways were associated with cancer progression and patients’ clinical outcome. The glycan biosynthesis-related functions and proteins were reported to be associated with good prognosis of patients with bladder cancer99. In our study, we found that higher expression level of proteoglycan biosynthetic process was significantly associated with better prognosis in SBC (Supplementary Fig. 15K), while the pyruvate metabolism was related to worse prognosis. Consistently, the proteins that enriched in the proteoglycan biosynthetic process including FUT8, GNAB, MGAT4A, and MAN1B1 also showed significantly elevated expression in P-IV (Supplementary Fig. 15L). Further survival analysis confirmed the elevated expression of these proteoglycan biosynthetic process-related proteins was associated with prolonged overall survival (Supplementary Fig. 15M). Meanwhile, we evaluated how the expression of these proteoglycan-related proteins related to CIN status. Comparative analysis revealed that proteins such as FUT8, GNAB, MGAT4A, and MAN1B1 showed higher expression levels in the CIN- group (Supplementary Fig. 15N), implying the enhanced proteoglycan biosynthetic process in patients belonging to the CIN- group. Taken together, we suggested that the upregulation of N-glycan biosynthesis pathway might contribute to the relatively better prognostic outcomes of P-IV subtype compared with other subtypes. The upregulation of metabolism-related pathway in P-IV subtype indicated that targeting metabolism could be a potential therapeutic approach for this subtype of SBC tumors.
Interestingly, patients with the P-II, the higher CIN score subtype, had significantly worse OS than patients with P-III subtype, which is the other higher CIN score subtype (Fig. 6G). To demonstrate whether these two higher CIN score subtypes showed differential prognosis, We then identified differential proteins and pathways between the P-II and P-III subtypes, which revealed downregulation of immune-related pathways, including chemokine signaling pathway and JAK-STAT signaling pathway in the P-II subtype (Supplementary Fig. 16A; Supplementary Data 7), which was consistent with the lower immune scores of P-II SBCs compared to others (Fig. 6D). Using pathway activity inferred by PROGENy100 (Supplementary Data 7), we found that inferred activities of apoptosis-related signaling pathways101,102,103,104, such as TRAIL, NF-kB, WNT, and TNF-α, were significantly decreased in the P-II subtype (Wilcoxon rank-sum test, p < 0.05, Fig. 6H), with the greatest decrease detected in TRAIL pathway (Fig. 6I). Additionally, the apoptosis pathway score based on our proteomic data were also lower in P-II than in P-III subtype (Supplementary Fig. 16B).
Further, we investigated the differences of TFs at both inferred TF activity and mRNA expression levels between P-II and P-III subtypes (Supplementary Fig. 16C and 16D; Supplementary Data 7). The comparison results showed that a known tumor suppressor, IRF1105, was significantly downregulated in the P-II subtype (Fig. 6J and Supplementary Fig. 16D; Supplementary Data 7). IRF1 was reported to induces TRAIL expression106. Furthermore, the TF activity score of IRF1 was positively correlated with the activity score of TRAIL pathway (Fig. 6K), whereas several TRAIL pathway genes, including TRAIL (TNFSF10), CASP8/10/3/7, and LMNA, were significantly downregulated in P-II subtype (Fig. 6L). These findings led us to propose that inactivation of IRF1 could result in downregulation of the TRAIL pathway, in turn suppressing apoptotic function, ultimately leading to worse prognosis for P-II subtype patients than P-III subtype patients. To test this possibility, we collected siRNA-induced IRF1 KD SBC cells and control cells for proteomic analysis to identify differential expressed gene sets (Fig. 6M). The ssGSEA analysis showed that apoptosis pathway proteins were indeed downregulated in IRF1 KD SBC samples (Fig. 6N).
Taken together, these findings illustrated distinct molecular mechanisms among the four proteomic subtypes in SBCs, especially between two higher CIN score subtypes, P-II and P-III subtypes, which have markedly different survival outcomes and regulatory activities of apoptosis-related proteins, such as TRAIL. These results suggested that proteomic subtyping could stratify SBC tumors with similar genomic features into different and more precise subtypes (Supplementary Fig. 17), which might benefit clinical treatment.
Pairwise comparison of pre- and post-recurrent SBCs
Gene and protein expression profiles can widely differ between primary and recurrent tumors within an individual patient38,107,108. Here, we conducted genomic, transcriptomic, and proteomic pairwise comparisons between pre- and post-recurrent SBC tumors within an individual patient to validate for potential features related to recurrence.
A total of 17 patients with SBC samples pre- and post- recurrence were included in following analysis, whom had corresponding paired genomic data (Fig. 7A and Supplementary Fig. 18A; Supplementary Data 8). Some post-recurrent tumors displayed genomic divergence from the pre-recurrent tumor, with higher or lower CIN scores than their corresponding pre-recurrent tumors (Fig. 7A; Supplementary Data 8), indicating different degrees of clonal evolution occurred within individual relapsed patients. Among the 17 patients with pre- and post-recurrent SBC samples showed in Fig. 7A, there were four patients (P007, P017, P014 and P020) who transitioned from CIN- to CIN+, three patients (P005, P006 and P016) who transitioned from CIN+ to CIN-, seven patients (P001, P002, P003, P010, P012, P021 and P123) who stayed CIN+ and three patients (P008, P009 and P015) who stayed CIN- (Supplementary Fig. 18A). Then, we investigated the OS and PFS among these four groups of patients. The results showed that there was no significant difference among these four groups of patients in both OS and PFS (Supplementary Fig. 18B). To exclude the influence raised by the PFS difference of pre- and post-recurrent tumors themselves, we further analysed the PFS of pre-recurrent tumors and post-recurrent tumors, respectively. These groups also did not have significant difference of OS and PFS (Supplementary Fig. 18C). We assumed that the lack of the patient number was the limitation for K-M analysis, which resulted in no significant difference among these four groups. In order to observe the trend of the PFS among four groups of patients, we also analysed and summarized the median PFS time of each group before and after their recurrence, respectively. When focusing on the median PFS time of pre-recurrent tumors, we found that patients with CIN- pre-recurrent tumors had longer median PFS time (Median PFS (CIN- to CIN + ) = 1219 days, Median PFS (stay CIN-) = 908 days) than who with CIN+ pre-recurrent tumors (Median PFS (CIN+ to CIN-) = 336 days, Median PFS (stay CIN + ) = 606 days), which consistent with our finding that CIN+ tumors had worse clinical outcomes compared with CIN- tumors. Moreover, we focused on the difference of the median PFS time between pre- and post-recurrent tumors in each group of patients. The CIN- post-recurrent tumors (Median average PFS = 323 days) showed relatively longer median PFS time than the CIN- pre-recurrent tumors (Median PFS = 336 days). Interestingly, when comparing the median PFS time between pre- and post-recurrent tumors, our results revealed that the CIN+ post-recurrent tumors (Median PFS = 124 days) showed obviously shorter median PFS time than the CIN- pre-recurrent tumors (Median PFS = 1219 days), indicating that the patients transitioned from CIN- to CIN+ had worse prognosis after recurrence. Taken together, these results suggested that the CIN status transition of the recurrent tumors could influence the patients’ clinical outcomes and lead to worse prognosis in patients who transitioned from CIN- to CIN + . Collectively, the results showed the trend that tumors transitioned to CIN+ after recurrence had shorter PFS, which were also consistent with our previous findings that CIN+ patients were associated with worse prognosis; whereas the more patients with paired tumors were needed for further validation. We further compared the median PFS between CIN+ pre-recurrent tumors and CIN- post-recurrent tumors. We found that CIN- post-recurrent tumors had similar median PFS (323 days) compared with the CIN+ pre-recurrent tumors (3336 days), while CIN+ post-recurrent tumors had shorter median PFS (124 days) compared with the CIN- pre-recurrent tumors (1219 days) (Supplementary Fig. 18D), suggesting that the CIN+ post-recurrent tumors might contribute to the worse the prognosis compared with the CIN- pre-recurrent tumors.
A Clinical sample types and genomic characterization of 17 pairs of pre- and post-recurrent tumors (top panel). Differences in ssGSEA scores between pre- and post-recurrent tumors (i.e., ssGSEA score of post-recurrent tumor subtracted from ssGSEA score of pre-recurrent tumor) of key molecular pathways at mRNA and protein levels associated with difference of CIN score (i.e., CIN score of post-recurrent subtracted from CIN score of pre-recurrent) (bottom panel). The coefficients and p-values were calculated by Spearman’s correlation test (two-sided). B A brief model showing that hyperactivation of E2F target genes promoted DNA RS. DNA RS tolerance resulted in CIN+, which in turn elevated DNA RS (top panel). The four dashed boxes showing the four major effects of CIN+ (bottom panel), namely, affecting mitochondrial protein homeostasis, making SBC resistant to radiotherapy, causing immune escape, and could be further subdivided into two proteomic subtypes, P-II had worse prognosis due to downregulation of TRAIL pathways.
According to the radiotherapy information of patients, we found compared to primary tumors or recurrent tumors without radiotherapy, the CIN scores were increased compared to primary tumors or recurrent tumors without radiotherapy in P020, P017, P123, P001 and P021, whereas decreased in a small proportion (P016 and P002) (Fig. 7A). Combining the significant increase with the slight decrease in a small portion of these samples suggested that the CIN score majorly increased in patients after radio-therapy with recurrence. Moreover, we explored the follow-up data of these two patients with lower CIN score after receiving radiotherapy (P016 and P002). We found that it took a longer time for the tumors of these two patients (P016 and P002) undergoing next operation after receiving radiotherapy (P016: 1465 days and P002: 1845 days) compared with other five patients (P020: 360 days, P017: 983 days, P123: 434 days, P001: 160 days and P021: 937 days). This difference in time interval between receiving radiotherapy and undergoing next operation might indicate that there was specific mechanisms leading to recurrence which caused their lower CIN status. We also observed that among the four patients who had both CIN- pre-recurrent tumors and CIN+ post-recurrent tumors, two patients (P017 and P020) exhibited resistance to radiotherapy, one patient (P014) showed sensitivity to high-dose radiotherapy, and one patient (P007) did not receive radiotherapy. We also investigated these patients who had CIN+ pre-recurrent tumor and CIN- post-recurrent tumor. There were three patients (P005, P006, P016) who had CIN+ pre-recurrent tumor and CIN- post-recurrent tumor (Supplementary Fig. 18A). Among these three patients, one patient (P005) was sensitive to low-dose radiotherapy, while two patients (P016 and P006) were resistant to low-dose radiotherapy (Supplementary Fig. 18A). Due to the limited number of patient samples, we did not find statistically significant differences based on clinical radiotherapy response data. Additionally, in order to infer the tumor’s response to radiotherapy, we compared the expression levels of protein enriched in DNA repair pathway and RPRD1B between tumors before and after recurrence in patients had CIN+ pre-recurrent tumor and CIN- post-recurrent tumor. The result revealed that the expression levels of DNA repair pathway was significantly downregulated in CIN- post-recurrent tumors compared with CIN+ pre-recurrent tumors (Supplementary Fig. 19A, Paired t-test, p = 0.012). The expression level of RPRD1B was also significantly downregulated in CIN- post-recurrent tumors compared with CIN+ post-recurrent tumors (Supplementary Fig. 19A, Paired t-test, p = 0.0065), indicating that the CIN- post-recurrent tumors might be more vulnerable to radiotherapy. To further explore the effect of CIN status on the response to radiotherapy, we performed in vitro validation experiments on UM-Chor1 (one of SBC cell lines) and patient-derived primary cells. The wild type UM-Chor1 cells (as the control), treated UM-Chor1 cells, which were identified as CIN+ cells (Methods), and CIN+ patient-derived primary cells all received 8 Gy dose of X-ray. After 2 days culture, the survival rates of cell lines and patient-derived primary cells after receiving radiation were detected through CellTiter-Glo Luminescent Cell Viability Assay (Methods). These results showed that the survival rates of CIN+ cells were significantly higher than the control (Supplementary Fig. 19B). Consistently, the survival rates of CIN+ patient-derived cells were significantly increased (Supplementary Fig. 19C). These results might indicate that samples who transitioned from CIN- to CIN+ tended to be more insensitive to radiotherapy.
We next found that ssGSEA scores of E2F targets gene set, DNA RS gene set and DNA repair related gene sets increased with elevated CIN score., while apoptotic pathway and immune related pathways were upregulated in post-recurrent tumors with decreased CIN score (Fig. 7A; Supplementary Data 8). In addition, we found 3 out of 4 patients who had CIN- pre-recurrent tumor and CIN+ post-recurrent tumor also had different immune microenvironment subtypes before and after recurrence, which altered from Hot to Cold, consistent with the link between CIN+ and immune suppression (Supplementary Fig. 19D; Supplementary Data 8). Furthermore, we found that 2 out of 4 patients that had CIN- pre-recurrent tumors and CIN+ post-recurrent tumors, were resistant to radiotherapy (Supplementary Fig. 18A; Supplementary Data 8). Protein homeostasis pathway was downregulated in 1q wildtype tumor compared to 1q gain tumor from the same patient (Supplementary Fig. 19E). We also observed that IL6/JAK/STAT3 pathway was downregulated in 9p/10q loss post-recurrent tumor compared to 9p/10q wildtype pre-recurrent tumor from the same patient (Supplementary Fig. 19F and G). The pairwise analysis provided complementary evidence to our findings. Our study demonstrated strong associations of E2F targets, mitochondrial protein homeostasis and immune microenvironment with CIN from both large sample cohort and pairwise perspectives. The different changing trends of CIN score after recurrence revealed different recurrence patterns of SBCs, indicating that recurrent tumors could have distinct tumorigenesis mechanisms.
To further explicate the intention of the comparisons between pre- and post-recurrent SBC tumors within an individual patient, we also investigated the correlation between pre- and post-recurrent proteome profile pairs from the same individuals (Supplementary Fig. 19H). The average correlations of paired tumors from patients, whose pre- and post-recurrent tumors stayed CIN+ or stayed CIN-, were 0.72, while the average correlations of paired tumors form patients who transitioned from CIN+ to CIN- and who transitioned from CIN- to CIN+ were 0.67. The correlations of paired tumors form patients who transitioned from CIN+ to CIN- and who transitioned from CIN- to CIN+ were significantly lower than the correlations of paired tumors form patients who stayed CIN+ and who stayed CIN- (Supplementary Fig. 19I), indicating that the pre-recurrent tumors from patients who transitioned from CIN+ to CIN- or CIN- to CIN+ might have more differences with the paired post-recurrent tumors than which in patients who stayed CIN+ or CIN-. The results that the pre- and post-recurrent pairs were not highly correlated with each other at the proteomics level supported the idea that recurrence (or progression) of a tumor could have different tumorigenesis mechanisms. Based on these observations, an approach that assessed the molecular properties of recurrent events independent of the primary tumor seems to be warranted. The proteome data of tumors closely reflected the alterations of protein, which could guild the clinical treatment and indicate the potential therapeutic targets.
In conclusion, our study showed that hyperactivation of E2F target genes promoted DNA RS tolerance to overcome CIN. Prognostic indicators such as DNAJA3, HSPD1, and HSPE1, as well as therapeutic targets such as RPRD1B and IRF1, have been preliminarily validated in SBC cell lines. CIN+ associated immune escape could result in CIN+ SBCs unresponsive to ICI therapy. These collective findings are summarized in a brief model (Fig. 7B), bringing a global perspective for understanding biological progress and clinical treatment of SBCs. Based on the proteomics and genomics profiles of 17 pairs of surgical samples from distinct tumor progresses (pre- and post- recurrence) of the same individuals in our cohort, we tried to address the question of whether the recurrent tumors should be considered independent tumors during treatment evaluation. These results suggested that we might carry on de novo analysis of recurrent tumors, which might guide further clinical strategies.
Discussion
SBC is a rare bone tumor with poor prognosis because of the difficulty in complete resection and its characteristics of radio-resistance and chemo-resistance1. Currently, there is no clear clinical classification and recognized prognosis indicators of the SBC. Several genomic alterations, including mutations or CNAs, were proposed to be relevant with the outcome of SBC patients in previous studies, but most of these studies were restricted by the cohort size or limited within the genomic sequencing level7,8,16. In our study, we conducted a large-scale multi-omics analysis on a SBC cohort in order to explore the potential prognostic markers and the underlying mechanisms. Importantly, we discovered that the CIN status significantly correlated with clinical outcomes of SBC patients, including the PFS, OS, and the sensitivity to radiotherapy of SBC, and identified potential therapeutic targets. In addition, immune subtyping and proteomic subtyping were performed based on our comprehensive multi-omics data, and CIN status was also related to the outcomes and potential therapeutic targets of distinct subtypes. We also found that SBC patient with CIN+ tumor, especially with incomplete resection CIN+ tumor, should receive more intense follow-up or further post-surgical treatment. Collectively, our study demonstrated the significance of CIN status in predicting the prognosis and guiding following treatment strategies of SBC patients.
According to previous studies, CIN can be caused by many factors, including DNA RS and chromosome missegregation via defective mitosis and/or telomere dysfunction, including defects in separation of sister chromatids, centrosome, microtubule, sister chromatid cohesion and mitotic spindle pathways45, which have been researched in other cancers, such as colorectal cancers44 and breast cancer109, etc. Combined with our results, we observed that only DNA RS was significantly upregulated in CIN+ SBCs across putative CIN causes mentioned above, suggesting that CIN in SBC was mainly caused by DNA RS. This result revealed a significant upregulation of replication stress pathway in numerical CIN+ SBCs, consistent with previous studies emphasizing the association of replication stress with CIN44,45. Our finding indicated that replication stress was the most prominently upregulated pathway contributing to numerical CIN in SBCs, compared to other putative causes. In previous studies, Dreyer et al. demonstrated the link between upregulated replication stress and genomic instability in pancreatic cancer50. Arlt et al. highlighted the importance of RS as a mechanism for generating CNAs110. Their findings were consistent with our results. Other studies have also suggested that multiple causes might collectively contribute to various types of CIN, and the role of other causative factors in SBC still required further investigation. CIN+ status was reported as one of the consequences of DNA RS and oncogenic activation caused by CIN would further promote DNA RS47. In normal cells, high level of DNA RS tended to induce cell apoptosis57. However, in tumor cells, CIN+ would facilitate cell proliferation due to the existence of DNA RS tolerance mechanism, such as the upregulation of E2F transcription activity and E2F targets56. In our study, E2F targets gene set had the strongest correlation with DNA RS. Thus, we inferred that the DNA RS tolerance mechanism in SBC mainly associated with E2F-dependent cell-cycle transcription. The upregulation of E2F transcription activity was observed in various cancers, which was mostly activated by CDK-RB1-E2F axis56. The activation of E2F3, a E2F activator, also reported to upregulate transcription of several E2F target genes56. In SBC, the integration of proteomic and phosphoproteomic data proposed that CDK-E2F3 regulation played an important role in the cell survival maintaining of CIN+ tumors in response to DNA RS-mediated CIN, which caused the poor outcomes of CIN+ patients. E2F3 was involved in the progression of liver111, breast112 and non-small cell lung cancer113 in previous studies, and several drugs targeting E2F3 was under development114. Thus, E2F3 might be a potential drug target of CIN+ patients in SBC.
Understanding the diversity of genomic CNA was essential for personalized medicine approaches and tailoring treatment strategies of tumor patients based on individual CNA profiles115. CNAs occurring on specific chromosomal arms may lead to amplification or deletion of tumor-related genes, affecting key biological processes such as cell proliferation, differentiation, metastasis, and treatment sensitivity116. Integrating arm-level amplifications and deletions arm-level amplifications and deletions with clinical parameters can potentially provide valuable insights into the underlying mechanisms driving SBC aggressiveness, aiding in the development of more effective prognostic markers and targeted therapeutic strategies. Chromosome 1q gain was demonstrated in multiple tumors with more metastasis and poorer prognosis, such as multiple myeloma117, breast cancer118, and glioma119. In our data, chromosome 1q gain was mainly detected in CIN+ samples, and had significant relation with poor prognosis. Upregulated mitochondrial functions have been reported in several cancers, while the genetic reasons of these abnormalities remain unknown (Zong et al., 2016). Here, we demonstrated that chromosome 1q copy number gain in SBC associated with the upregulation of mitochondrial functions, especially protein homeostasis pathway. Our analysis and in vitro experiments confirmed that chromosome 1q gain played a significant role in SBC cell survival through overexpression of mitochondrial protein homeostasis related proteins, such as HSPD1, HSPE1 and DNAJA3, which agreed with the fact that mitochondrial protein homeostasis process and its key regulator proteins can facilitate tumor cell progression in other tumors120. The enrichment of mitochondrial protein homeostasis-related genes in SBCs with 1q gain suggested their potential involvement in supporting tumor proliferation and progression. Moreover, the significance of protein homeostasis-related genes in the context of cancer metabolism might imply in their crucial role in maintaining mitochondrial functions, such as amino acid metabolism, and adaptations to metabolic stressors. Mitochondria, which are related to the initiation and development of tumors or diseases, have been increasingly concerned in recent years121. Altogether, our results further explored the downstream mechanism and provided a potential treatment target for SBC patients with 1q gain.
In SBC patients, radio-resistance is quite common and frequently lead to poor outcomes of patients77. It was reported that radiotherapy could induce DNA damage122. There were several factors that led to radio-resistance in other tumors, including DNA repair, cell cycle arrest, and alterations of oncogenes and tumor suppressors122. In our study, CIN status was found to be relevant with the sensitivity to radio-therapy, which had also been observed in other tumors (e.g. glimoas)123. Additionally, DNA repair pathways and related genes were upregulated in both CIN+ and radio-resistant subgroup patients. Thus, we proposed that DNA repair might play an important role in radio-resistance in SBC. It was reported that DNA repair pathways included ten major pathways84, which have been reported to lead to radio-resistance in different types of tumors124,125,126. RPRD1B was found to be significantly correlated with CIN score and radio-resistance degree across all genes in this study, whose relationship with radio-resistance had not been reported before85,86. Our in vitro experiments showed that RPRD1B KD could increase the radio-sensitivity of SBCs. We further uncovered that RPRD1B was correlated with DNA repair pathways in SBC. In addition, among ten DNA repair pathways, only HDR and MMR were significantly associated with both RPRD1B and CIN score in our dataset, which agreed with the role of RPRD1B in HDR and MMR in previous studies85,86. In our study, we pointed out the DNA repair pathway was the potential radio-resistance mechanism of SBC in a large-scale clinical cohort, and specifically, PRRD1B can be a indicator of DNA repair and a potential target to further enhance SBC radiotherapy sensitivity. We found that RPRD1B might be an upstream regulator of the HDR and MMR DNA repair pathways. This finding was consistent with previous findings in other cancers, such as breast cancer85, while the association between RPRD1B and HDR/MMR has not been mentioned in SBC before. Our findings suggested that RPRD1B had a close association with DNA repair in SBC, and also provided guidance of targeting specific DNA repair processes for treatment. The higher expression level of DNA damage repair genes, such as RPRD1B, in pre-radiotherapy tumors might benefit the development of resistance for radiotherapy. By understanding the role of RPRD1B in DNA repair, it might be possible to develop strategies to impair the efficacy of DNA repair in SBC tumors or sensitize SBC tumors to DNA-damaging treatments such as radiotherapy.
In previous studies on other tumor types, CIN tended to enhance immune related signaling pathways and play a significant role in crosstalk between the tumor and its microenvironment in many tumors, such as colon cancer93. Moreover, multiple studies have demonstrated that micronuclei generated by CIN could activate the cGAS-STING pathway, and thereby activate immune signaling pathways90,91,92. Interestingly, we found that immune associated pathways were significantly suppressed in CIN+ SBCs. Combined with multi-omics analysis, we found that the losses of chromosome 9p and 10q was the most significant arm events correlated with the immune Cold phenotype in SBC. Consistent with previous studies that the deletion of chromosome 9p may lead to resistance to ICI therapy127. In our study, we further confirmed that 9p loss led to the down-regulation of immune-related pathways through the deletion of IFN genes and JAK-STAT gene located on 9p. Although 10q deletion has been widely observed in many types of tumors128,129, whose relationship with immune microenvironment remains unknown. In our study, we found that chromosome 10q downregulated IFN alpha pathway and TNFa signaling by losing key regulators of the NF-KB pathway genes located on 10q. Thus, CIN- SBCs with Hot immune subtype and overexpression of immune checkpoint markers, such as PD-1, PD-L1 and CD8, might benefit from ICI therapy, while ICI therapy might not be useful for CIN+ patients with Cold immune subtype, suggesting the need for other therapeutic strategies in CIN+ patients. Together, these findings revealed the diversity of multipronged effects between the tumor and its microenvironment resulted from CIN, and indicated that CIN could act as a genomic source for immune escape in SBC.
In our study, unsupervised proteomic subtyping classified four proteomic subtypes across all SBCs with distinct molecular features. The usage of proteomic subtypes had advantages over CIN + /- groups. The proteomic classification showed a further refinement to CIN+ SBCs, dividing higher CIN score SBCs into two subtypes (P-II and P-III). The P-II and P-III subtypes, both had relatively higher CIN score than other two subtypes, but showed differential prognosis and distinct molecular characteristics. Although P-II and P-III subtypes both showed inferior prognosis than P-I and P-IV subtypes, P-II subtype had significantly worse prognosis compared with P-III subtype. Moreover, apoptosis-related TRAIL pathway was significantly downregulated in P-II subtype, suggesting that P-II SBCs suppressed apoptosis function through TRAIL pathway to overcome CIN-imposed stresses, which also provided rationale for targeting apoptosis pathway in CIN+ SBCs. Additionally, P-I and P-IV subtypes showed relatively better prognosis compared with P-II and P-III subtypes. The P-I subtype and P-IV subtype exhibited enrichment for ECM-related pathways, such as ECM-receptor interaction, and metabolic pathways, such as glycan biosynthesis pathway, respectively. Published studies have reported similar findings in other cancer types. For example, in clear cell renal cell carcinoma130 and gastrointestinal stromal tumors131, the upregulation of ECM-related pathways, such as ECM-receptor interaction and focal adhesion, has been associated with improved patient outcomes. Moreover, ECM-associated functions were reported to be represent promising drug targets against in other cancers, such as breast cancer and melanoma132,133. In our study, the high levels of ECM pathways in P-I suggested that targeting ECM-related functions might be a promising therapeutic strategy for SBC. It was reported that aberrant signaling cascades and disrupted metabolic pathways might be a novel targeted approach for SBC134, consistent with our finding that the metabolism dysregulation could be a potential therapeutic target for SBC patients within P-IV subtype. The proteomic subtyping stratified SBC tumors with similar genomic features into different and more precise subtypes, which might benefit clinical treatment.
Previous work has reported distinct patterns between initial and recurrent tumors of the same individual as well135. In our study, genomic divergence between pre- and post-recurrent SBC tumors suggested dynamic changes in tumor characteristics. The different changing trends of CIN score after recurrence revealed different recurrence patterns of SBCs, indicating that the recurrent tumors might possess different tumorigenesis mechanisms. In addition, association between CIN scores and molecular pathways aligned with our previous findings and highlighted the interplay between genomic instability and cellular pathways. Combining the significant increase with the slight decrease in a small portion of paired samples, we considered that the CIN score majorly increased in patients after radio-therapy with recurrence. Due to the limited number of patients with paired samples, our finding might have certain one-sidedness and individual differences. The observed lower CIN scores in patients after radiotherapy with recurrence might seem contrary to the argument that CIN- SBC are more susceptible to radiotherapy and should therefore exhibit clonal selection towards becoming CIN + . However, the relationship between CIN and radiotherapy was complex and could vary among individual patients. We reviewed previous studies and found that the CIN status was reported to be decreased in patients with solid tumors after receiving adiotherapy136. In their study, the CIN score decreased in 13 patients (56.5%), while it increased in eight patients (34.8%) among 21 patients.
In addition, we found that CIN- post-recurrent tumors might be more vulnerable to radiotherapy through paired samples and cell experiments. In our study, the median PFS time of CIN+ post-recurrent tumors was shorter (124 days) than that of CIN- pre-recurrent tumors (1219 days). We also analyzed the PFS and OS between the CIN- to CIN+ patients (patients who had CIN- pre-recurrent tumors and CIN+ post-recurrent tumors) and the CIN+ to CIN- patients (patients who had CIN+ pre-recurrent tumor and CIN- post-recurrent tumor), in order to compare the difference of prognosis between patients with distinct transition of CIN status before and after recurrence. The PFS and OS showed no significant difference between these two groups. The limited number of patients might limit the investigation of patients’ prognosis. Based on the proteomics and genomics profiles of 17 pairs of surgical samples from distinct tumor progresses (pre- and post- recurrence) of the same individuals in our cohort, we tried to address the question of whether the recurrent tumors should be considered independent tumors during treatment evaluation.
Taken together, our study revealed the significance of CIN status in the prognosis and clinical treatment decisions of SBC patients based on our multi-omics data. Both specific CNA events and prognostic markers of SBC patients should be detected for precise therapy of SBC patients. This integrative proteogenomic analysis substantially expands the current understanding of SBC molecular features and can guide the development and selection of effective treatment strategies.
Methods
Our research complies with all relevant ethical regulations. The Research Ethics Committees of Huashan Hospital, Fudan University approves this study (KY2021-499).
Sample selection
We screened patients who underwent resection surgery for the treatment of SBC at Huashan Hospital, Fudan University (Shanghai, China) from October 2006 to September 2020. Electronic medical records were screened retrospectively. In total, 162 patients with available diagnostic and clinical information were consecutively recruited in our cohort. The cohort consisted of 85 male patients and 77 female patients, with a median age of 45.5 years (range, 11–80 years). A total of 187 skull-base chordoma tumor samples were collected from 162 patients, including 121 primary tumors, 38 recurrent tumors without radiotherapy and 28 recurrent tumors after radiotherapy. Primary tumors were collected from treatment naïve chordoma patients. Recurrent tumors without radiotherapy were collected from recurrent chordoma patients who did not have a history of radiotherapy before this surgery. Recurrent tumors after radiotherapy were collected from recurrent SBC patients who received pre-surgery radiotherapy. Skull-base chordoma tumor tissues were surgically resected and formalin-fixed paraffin-embedded (FFPE). We retrieved and scanned all the available diagnostic pathological slides. All the histological and haematoxylin and eosin (H&E) slides were independently reviewed by at least two experienced pathologists to verify the diagnostic results. Acceptable SBC tissue segments had to contain >70% tumor cell nuclei at the top and bottom of histological sections decided by two pathologists. Tumor segments with high tumor purity (>70%) were micro-dissected appropriately. The IHC staining (TBXT marker) was performed to verify the tumor purity (Supplementary Fig. 20). In addition, 85 patients had matched whole-blood samples, which were also collected. The clinical information regarding gender, age, date of surgical resection, patients’ overall survival (OS) and progression-free survival (PFS), radiotherapy dose and radiotherapy response along with relevant diagnostic information were obtained from Huashan Hospital and the baseline characteristics of SBC patients were summarized in Supplementary Data 1. Median follow-up was 2217 days (74 months). At the last follow-up, 39 patients (24%) had died of SBC. The Research Ethics Committees of Huashan Hospital, Fudan University approved this study (KY2021-499) and written informed consent was obtained from all the involved patients. The study was performed in accordance with the Declaration of Helsinki.
Among 162 patients, one sample, two samples and three samples were collected in 139, 21 and 2 patients, respectively. There were 19 patients who had one primary tumor and one matched recurrent sample, and 2 patients who had one primary tumor and two matched recurrent samples. Except for these 21 patients, there were two more patients (P122 and P123) who had one recurrent sample before radiotherapy and one matched sample after radiotherapy. The recurrent tumor without radiotherapy and the matched recurrent tumor after radiotherapy collected form the same patient were collected before the patient receiving radiotherapy and after the patient receiving radiotherapy, respectively. We considered that the recurrent tumor without radiotherapy and the recurrent tumor after radiotherapy collected form the same individuals were paired tumors. Thus, the patients, P122 and P123, were also patients with paired tumors. Taken together, there were a total of 23 patients who had paired tumor samples in our study (Figure RL30A). The paired patients who also had matched WES data were used in the analysis in Fig. 7. The tumor types of the samples were annotated in the Fig. 7A. New research IDs were assigned to each sample and patient, and the patient pathology reports were de-identified.
Tumor purity
According to our previous single-cell RNA sequencing data, the percentage of tumor cells was appropriate 66.7%137. In order to increase the tumor purity of our samples in this research, we performed IHC stain on every FFPE samples and defined the selection areas of every sample based on the separate identification by two different pathologists (Supplementary Fig. 20). According to a previous study about prognostic subtypes of chordoma138, the median of their calculated tumor purity is 66%, which roughly equivalent to our results. In addition, we also reviewed literature on tumors similar to the pathological histology of chordoma, such as osteosarcoma. Related studies have also reported that the median tumor purity of osteosarcoma is ~75%139,140. ABSOLUTE algorithms were utilized to evaluate the overall computational purity score for each sample. Computational tumor purity was inferred by R package ABSOLUTE141 using WES data. The tumor purity of each sample is presented in Supplementary Data 1 (median = 78%). Based on the evidence above, the median tumor purity of 78% in our study was considered reasonable and appropriate for SBC.
Radio-resistance degree definition
Radiotherapy operated on skull-base chordoma included low-dose (<60 Gy) radiotherapy such as proton beam (PB) therapy, or high-dose (> 60 Gy) radiotherapy such as gamma knife stereotactic radiation (GKSR) therapy. Patients who relapsed after radiotherapy were defined as radio-resistant patients, while patients who did not relapse after radiotherapy were defined as radio-sensitive patients. Among 162 patients, 91 (56%) patients obtained detailed radiotherapy records including radiotherapy dose and radiotherapy outcome. Among these 91 patients, 73 patients with available pre-radiotherapy tumor samples were included for the subsequent analysis in Fig. 4. Then, we divided 73 patients with radiotherapy records into four subgroups based on radiotherapy dose and their response to radiotherapy: low-dose radio-sensitive (n = 26), high-dose radio-sensitive (n = 21), low-dose radio-resistant (n = 19) and high-dose radio-resistant (n = 7) subgroups. High-dose resistant, low-dose resistant, high-dose sensitive and low-dose sensitive were designated “4”, “3”, “2” and “1”, respectively.
Sample preparation
FFPE specimens were prepared and provided by Huashan Hospital. A 3 μm slide from each FFPE block was used for H&E staining. For genomic, proteomic, and phosphoproteomic sample preparation, 10 μm slides were deparaffinized with xylene and washed with gradient ethanol. For transcriptomic sample preparation, 10 μm slides were prepared from the samples without xylene deparaffination or gradient ethanol wash. The specimens were selected according to H&E staining status and scraped. All materials were aliquoted and stored at −80°C.
Whole-exome sequencing
DNA extraction
DNA isolated from FFPE tumor samples was used for WES, and matched germline DNA was obtained from whole-blood samples. After FFPE tumor sections were scraped into 1.5 mL micro centrifuge tube, deparaffinization solution was used to remove paraffin. Then, Maxwell 16 FFPE Plus LEV DNA Purification Kit (Promega) was used to extract FFPE DNA according the protocol. Total DNA was extracted from 1 mL blood samples using QIAamp DNA Blood Mini Kit (Qiagen-51106) according to the manufacturer’s instructions. Then, the integrity and concentration of the total DNA was determined by agarose electrophoresis and Qubit 3.0 fluorometer dsDNA HS Assay (Thermo Fisher Scientific). OD260/OD280 was measured by NanoDrop2000 (Thermo Fisher Scientific). About 300 ng high-quality DNA sample (OD260/280 = 1.8 ~ 2.0) was used to construct sequencing library.
WES library preparation
The 300 ng genomic DNA concentrations were sheared with Covaris LE220 Sonicator (Covaris) to target of 150–200 bp average size. DNA libraries were prepared using SureselectXT reagent kit (Agilent). The fragments were repaired the 3’ and 5’ overhangs using End repair mix (component of SureselectXT) and purified using Agencourt AMPure XP Beads (Beckman). The purified fragments were added with ‘A’ tail using A-tailing Mix (component of SureSelectXT) and then ligated with adapter using the DNA ligase (component of SureselectXT). The adapter-ligated DNA fragments were amplified with Herculase II Fusion DNA Polymerase (Agilent). Finally, the pre-capture libraries containing exome sequences were captured using SureSelect Human All Exon V5kit (Agilent).
Illumina sequencing
DNA concentration of the enriched sequencing libraries was measured with the Qubit 3.0 fluorometer dsDNA HS Assay (Thermo Fisher Scientific). Size distribution of the resulting sequencing libraries was analyzed using Agilent BioAnalyzer 4200 (Agilent). Paired-end sequencing is performed using an Illumina NovaSeq6000 system following Illumina-provided protocols for 2 × 150 paired-end sequencing. WES was conducted with mean coverage depths of 200X for tumor samples and 100X for blood samples.
WES data analysis
Whole-exome sequencing quality control
Quality control was conducted on each sample to ensure that raw data had good metrics and no significant biases which may affect following analysis. In our project, read quality was calculated for all samples using FastQC (v0.11.9) software with the default parameters.
Filter of raw data
Fastp (v0.22.0) software was used to remove the adapter sequence of raw data (Fastq) and the reads whose length was >75 bp were selected after removing adapters. Then the selected reads, named as clean reads, were used for downstream analysis.
Sequence alignment
The clean reads of each sample were mapped to the human (Homo sapiens) genome (version hg19) by using the BWA-MEM (v0.7.17) algorithm to obtain the bam file, followed by marking the PCR reads in the bam, rearranging the regions that may have Indel mutations, and recalibrating the quality of each base pair.
Somatic variant calling
Gene variants refer to changes in the base of genome, including point mutations caused by single base changes, or deletions, duplications, insertions of multiple bases. The workflow of Sentieon (20201001) was carried out to detect nonsynonymous somatic variants, including single nucleotide variants (SNVs) and small insertions and deletions (indels). Then, the variants were annotated by Annovar (Date 20180416). To get somatic variants of high confidence, stringent downstream filters were used. We first exclude the nine longest genes (TTN, MUC16, SYNE1, NEB, MUC19, CCDC168, FSIP2, OBSCN, GPR98) as they tend to acquire numerous mutations by chance142. Variants were excluded if they did not pass all of the following filters: variant allele fraction (VAF) in normal/VAF in tumor < 0.2, total read count in tumor > = 5, VAF in tumor > = 0.05, and ExAC frequency < = 0.001.
Tumor Mutation Burden (TMB)
TMB was defined as the number of somatic mutations in the coding region per megabase (mutations/Mb), including SNVs and indels. We compared our chordoma tumors to other tumor cohorts obtained from TCGA MC3 study143 using maftools (v2.4.12).
Somatic Copy Number Alteration (CNA) analysis
CNVkit software (version 0.99) was used to analyze the CNA of single sample and paired tumor samples, and a 200 bp bin size was used to analyze the whole-genome CNA. CNAs were called by following the somatic CNA calling pipeline in GATK’s (GATK4) Best Practice. Genomic Identification of Significant Targets in Cancer (GISTIC2.0) algorithm144 was used to identify significantly amplified or deleted focal-level or arm-level events across all samples. To exclude false positives, relatively stringent cutoff thresholds were used with parameters: -ta 0.1 -tb 0.1 -brlen 0.98 -conf 0.99. Other parameters were the same as the default values. Based on the published literature, a log2 ratio cutoff of 0.1 and −0.1 was used to define CNA amplification and deletion, respectively. Every gene of each sample was assigned a thresholded copy number level, ranging from −2 to 2, that reflected the magnitude of its deletion or amplification.
Co-occurrence and mutual exclusivity analysis of mutations
In our dataset, Fisher’s exact test was used to investigate cooccurrence and mutually exclusive CNA events.
Classification of samples with Chromosome instability (CIN)
It is reported that WES data can be used to infer CIN in tumor studies21,22,23.To classify the tumor samples into CIN + samples and CIN- samples, we calculated the CIN score, which is defined as the length of all segments that have copy number (as inferred by CNVkit) different from diploidy (-ta 0.1 or -tb 0.1) divided by the total length of the genome22,23,46. The resulting CIN score showed a bimodal distribution. We dichotomized the samples into two CIN status using a cutoff of 0.341, which has the minimal local density separating CIN+ and CIN- populations.
RNA-seq
RNA extraction
RNA was extracted from tissues by using TIANGEN® RNAprep Pure FFPE Kit (#DP439) according to the reagent protocols. For library preparation of RNA sequencing, a total amount of 500 ng RNA per sample was used as the input material for the RNA sample preparations. Sequencing libraries were generated using Ribo-off® rRNA Depletion Kit (H/M/R) (Vazyme #N406) and VAHTS® Universal V6 RNA-seq Library Prep Kit for Illumina (#N401-NR604) following the manufacturer’s recommendations and index codes were added to attribute sequences to each sample. The libraries were sequenced on an Illumina platform and 150 bp paired-end reads were generated.
RNA-Seq data analysis
RNA-seq raw data quality was assessed with the FastQC (v0.11.9) and the adaptor was trimmed with Trim_Galore (version 0.6.6) before any data filtering criteria was applied. Reads were mapped onto the human reference genome (GRCh38.p13 assembly) by using STAR software (v2.7.7a). The mapped reads were assembled into transcripts or genes by using StringTie software (v2.1.4) and the genome annotation file (hg38_ucsc.annotated.gtf). For quantification purpose, the relative abundance of the transcript/gene was measured by a normalized metrics, FPKM (Fragments Per Kilobase of transcript per Million mapped reads). Transcripts with an FPKM score above one were retained, resulting in a total of 18,788 gene IDs. All known exons in the annotated file were 100% covered.
Peptide preparation for MS analysis
Protein extraction and tryptic digestion
Lysis buffer [0.1 M Tris-HCl (pH 8.0), 0.1 M DTT (Sigma, 43815), 1 mM PMSF (Amresco, M145)] was added to the extracted tissues, and subsequently sonicated for 1 min (3 s on and 3 s off, amplitude 25%) on ice. The supernatants were collected, and the extracted tissues were then lysed with 4% sodium dodecyl sulfate (SDS) and kept for 2–2.5 h at 99 °C with shaking at 180 rpm. The solution was collected by centrifugation at 12,000 × g for 5 min. A 4-fold volume of acetone was added to the supernatant and kept in −20 °C for a minimum of 4 h. Subsequently, the acetone-precipitated proteins were washed three times with cooled acetone. Filter-aided sample preparation (FASP) procedure was used for protein digestion145. The proteins were resuspended in 200 μL 8 M urea (pH 8.0) and loaded in 30 kD Microcon filter tubes (Sartorius) and centrifuged at 12,000 g for 20 min. The precipitate in the filter was washed three times by adding 200 μL 50 mM NH4HCO3. The precipitate was resuspended in 50 μL 50 mM NH4HCO3. Protein samples underwent trypsin digestion (enzyme-to-substrate ratio of 1:50 at 37 °C for 18–20 h) in the filter, and then were collected by centrifugation at 12,000 g for 15 min. Additional washing, twice with 200 μL of MS water, was essential to obtain greater yields. Finally, the centrifugate was pumped out using the AQ model Vacuum concentrator (Eppendorf, Germany).
The enrichment of phosphorylated peptides
For the phosphoproteomic analysis, the peptides were extracted from the FFPE slides after trypsin digestion using the methods described above. The tryptic peptides were then enriched with High-Select™ Fe-NTA Phosphopeptides Enrichment Kit (Thermo Fisher Scientific) following the manufacturer’s recommendations. Briefly, the peptides were suspended with binding/wash buffer (provided in the enrichment kit), mixed with the equilibrated resins, and incubated at 21 − 25 °C for 30 min. After incubation, the resins were washed thrice with binding/wash buffer and twice with water. The enriched peptides were eluted with elution buffer (contained in the enrichment kit) and dried in a vacuum drier at 30 °C.
ESI-LC-MS/MS analysis
Proteome and phosphoproteome analysis with Liquid chromatography–tandem mass spectrometry
The Orbitrap Exploris 480 Mass Spectrometer (Thermo Fisher Scientific) is equipped with an Easy nLC-1200 (Thermo Fisher Scientific) and a Nanoflex source (Thermo Fisher Scientific). The peptides were re-dissolved in 12 μL loading buffer (5% methanol and 0.2% FA). Peptide samples were loaded onto a trap column (100 μm × 2 cm, homemade; particle size, 3 μm; pore size, 120 Å; SunChrom, USA), separated by a homemade silica microcolumn (150 μm × 30 cm, particle size, 1.9 μm; pore size, 120 Å; SunChrom, USA) with a gradient of 4–100% mobile phase B (80% acetonitrile and 0.1% formic acid) at a flow rate of 600 nL/min for 150 min. We used the data dependent acquisition (DDA) strategy of LC–MS/MS based proteome and phosphoproteome in this study. MS was operated under a data-dependent acquisition mode. LC–MS/MS based proteomic and phosphoproteomic experiments were conducted with Field Asymmetric Ion Mobility Spectrometry (FAIMS). FAIMS voltages were set to −45 V and −65 V, respectively, and other parameters were consistent and set as follows: protein quantification consisted of an MS1 scan at a resolution of 120,000 (at 400 m/z). The automatic gain control (AGC) for full MS and MS/MS was set to 3E6 and 5E4, respectively, with maximum ion injection times of 80 and 22 ms, respectively.
Database searching for proteomic and phosphoproteomic MS raw data
Peptide identification and protein quantification
Peptide identification was processed with the one-stop proteomic cloud platform “Firmiana”146 against the homo sapiens RefSeq protein database (updated on 06-09-2021) in the National Center for Biotechnology Information. The maximum number of missed cleavages was set to two. In our study, all the proteomic analysis was performed utilizing Orbitrap Exploris 480 Mass Spectrometer (Thermo Fisher Scientific) mass spectrometer with FAIMS (Thermo Scientific). The dispersion voltage (DV) was set to −45 V and −65 V. MS analysis was conducted with one full scan (300 – 1,400 m/z, R = 120,000 at 200 m/z) at automatic gain control (AGC) target of 3e6 ions, followed by up to 20 data-dependent MS/MS scans with higher-energy collision dissociation (target 5e4 ions, max injection time 20 ms, isolation window 1.6 m/z, normalized collision energy of 27%). Detection was performed using Orbitrap (R = 7,500 at 200 m/z) and data were acquired using Xcalibur software (Thermo Fisher Scientific). Moreover, to demonstrate the high accuracy of our mass measurements, we presented the ppm of identified peptide sequences in the search results of our quality control samples. The results revealed that all peptide sequences had ppm values within 10 ppm (Supplementary Fig. 21A). The instrument used in our study has been meticulously maintained and monitored to ensure precise mass measurements. To maintain the stability of our mass spectrometer’s mass accuracy, we implemented strict quality control measures on a daily basis for the mass spectrometry instrument used in the study. The instrument was calibrated using standard calibration solutions to ensure deviation was controlled within 3ppm (Supplementary Fig. 21B and 21C), allowing us to closely monitor and validate the mass accuracy of our instrument. A mass tolerance of 10 ppm for precursor was allowed, consistent with the acceptable tolerance level in the proteome community. The rigorous quality control measures, including regular instrument calibration, were employed to maintain stability and accuracy throughout the study.
For phosphoproteomic data, a label-free quantification analysis was performed using Proteome Discover (version 2.3). The fixed modification was carbamidomethyl (C), and the variable modifications were oxidation (M), acetylation (protein N-term), and phospho (S/T/Y). The cutoff FDR, using a target-decoy strategy, was set at 1% for both the proteins and peptides.
Quality control of the MS data
Quality control of the MS platform
The HEK293T cell (National Infrastructure Cell Line Resource) lysate was used for the standard sample. The standard samples were digested and analyzed using the same method and conditions as the SBC samples. The proteome and phosphoproteome data acquisition process of our study took 45 days in total. The standard samples were measured every 3 days for the quality control of MS performance. There were a total of 15 quality control runs during the proteome and phosphoproteome data acquisition process. Pearson’s correlation coefficients were calculated for all 15 quality control runs, and the results are shown in Supplementary Fig. 1F. The above results demonstrated the consistent stability of the MS platform. The average correlation coefficient of the QC samples was 0.97 (range, 0.96–0.99), validating the consistency and stability of our mass spectrometry (MS) platform.
Quality control and assessment of LCMS/MS data
A label-free quantification algorithm, MaxLFQ algorithm, was used for protein quantification. Values of LFQ calculated by MaxQuant (version 2.2.0.0) software were quantile normalized. The density plot of the normalized intensities of the proteins identified in each sample showed that all samples passed the quality control with an expected unimodal distribution (dip statistic test. PCA analyses of both proteomic and phosphoproteomic profiles showed no significant batch effects). Proteins identified in over 20% of all samples were used in subsequent analysis. The threshold of 20% allowed us to capture the heterogeneity of the tumors while ensuring the reliability of our conclusions, and was consistent with previous published studies147,148. The NA values were replaced with 1e-5 to adjust extremely small values.
For the phosphoproteomic data, the intensities of the phosphopeptides were extracted from the Proteome Discover (version 2.3). For the phosphoprotein abundance calculation, the non-redundant phosphopeptide list was used to assemble the proteins by following the parsimony principle. The ptmRS was used to determine phosphosite confidence, and phosphosite probability >0.75 is considered as confident phosphosites149 to ensure the inclusion of highly reliable and confidently identified phosphorylation events.
Global heatmap
Expression value of each gene in the global proteomic expression matrix was transformed to a z-score across all the samples. The z-score-transformed matrix was visualized using the “pheatmap” (version 1.0.12) R package.
Differential protein analysis
Wilcoxon rank-sum test was applied to compare the differentially expressed proteins between two groups, and the p-values were adjusted by Benjamini-Hochberg method. The adjusted p-values can be used to determine whether there is a statistically significant difference between two groups of samples. The adjusted p-values can be used to determine whether there is a statistically significant difference between two groups of samples. The fold change was calculated as the median log2 fold change. The upregulated or downregulated proteins in a group were identified as differentially expressed proteins compared with the other group (log2 fold change > 0.3 or <−0.3, Benjamini-Hochberg adjusted p < 0.05). ANOVA test was applied to compare the differentially expressed proteins among more than two subgroups, and the p-values were adjusted by Benjamini-Hochberg method.
Pathway enrichment analysis
Gene sets of molecular pathways from the KEGG/Hallmark/Reactome databases were applied as background. Differentially expressed proteins defined in different subtypes or subgroups (i.e. CIN+ vs. CIN-) were subjected to pathway enrichment analysis in “clusterProfiler” (version 4.0.5) R package.
Functional enrichment analysis of multi-omics data using GSVA/ssGSEA analysis
To further analyze biological characteristics of different samples, we performed single-sample gene set enrichment (ssGSEA/GSVA) analysis. Gene expression data of proteome or RNA-seq data across different samples were used to achieve enrichment scores over gene sets (i.e. KEGG, Reactome, Gene Ontology and HALLMARK) downloaded from the MsigDB (v7.4, https://data.broadinstitute.org/gseamsigdb/msigdb/release/7.4/) and MitoCart3.068 with at least 10 overlapping genes via the R/Bioconductor package GSVA. GSEA analysis was performed by the GSEA software (https://www.gseamsigdb.org/gsea/index.jsp). Gene sets including KEGG, Reactome, Gene Ontology and HALLMARK downloaded from the MsigDB (v7.4, https://data.broadinstitute.org/gsea-msigdb/msigdb/release/7.4/) were set as background.
Consensus clustering analysis for proteome and transcriptome
Consensus clustering was performed to identify proteomic clusters of SBC using the ConsensusClusterPlus and CancerSubtypes package in R. For the clustering of proteomic data, a total of 1354 proteins (the top 30% most varied protein within 187 tumor samples) were selected. The following parameters were used for clustering: reps = 1000, pItem = 0.8, pFeature = 0.8, clusterAlg = “pam”, distance = “spearman”, and clustering with up to 10 clusters. For the clustering of transcriptomic data, 1,471 mRNAs (the top 10% most varied mRNAs) were selected in 180 tumor samples. Parameters used for clustering were reps = 1000, pItem = 0.8, pFeature = 0.8, clusterAlg = “pam”, distance = “pearson”, and clustering with up to 10 clusters. The methods and parameters of consensus clustering were commonly used in tumor multi-omic studies130,150. The consensus matrices for k = 3, 4, and 5 clusters are shown in our study (Supplementary Fig. 11A). By focusing on the average pairwise consensus matrix within consensus clusters, the delta plot of the relative change in the area under the cumulative distribution function (CDF) curve, and the average silhouette distance for consensus clusters were calculated (Supplementary Fig. 11A, B). We chose four proteomic subtypes and three transcriptomic subtypes based on 4 factors: consensus matrices, consensus cumulative distribution function (CDF) plot, delta area plot (inflection point), and silhouette plot148,150. We determined the consensus matrix of k = 4 as the best solution for proteomic clustering and k = 3 as the best solution for transcriptomic clustering, since it deemed to be the cleanest consensus matrices background, the largest AUC in CDF plot, and the largest average silhouette width (0.74 in proteomic cluster and 0.84 in transcriptomic cluster), and the obvious inflection point (delta area plot) among all clusters (Supplementary Fig. 11A, B). Thus, we chose k4 for proteomic subtypes and k3 for transcriptomic subtypes based on unsupervised clustering as the best solution for clustering for it deemed to be a cleanest separation among clusters. In addition, the largest average silhouette width suggested the highest similarity of samples in each cluster allocated by it.
Proteomic subtype and clinical feature associations
The association between clinical information and proteomic subtypes was evaluated using Fisher’s exact test for categorical data and Wilcoxon rank-sum test for continuous data. Log-rank tests and Kaplan-Meier survival curves were used to compare the OS and PFS among the proteomic subtypes.
Kinase activity prediction via PTM-SEA
Kinase activity scores were inferred from phosphorylation sites by employing PTM signature enrichment analysis (PTM-SEA) using the PTM signatures database (PTMsigDB) v1.9.0 (https://github.com/broadinstitute/ssGSEA2.0). Sequence windows flanking the phosphorylation site by 7 amino acids in both directions were used as unique site identifiers. Only fully localized phosphorylation sites as determined by Spectrum Mill software were taken into consideration. Phosphorylation sites on multiply phosphorylated peptides were resolved using the approach described in Krug et al. 84 resulting in a total of 29,406 phosphorylation sites that were subjected to PTM-SEA analysis using the following parameters:
gene.set.database = “ptm.sig.db.all.flanking.human.v1.9.0.gmt”
sample.norm.type = “rank”
weight = 0.75
statistic = “area.under.RES”
output.score.type = “NES”
nperm = 1000
global.fdr = TRUE
min.overlap = 5
correl.type = “z.score”
Phosphopeptide analysis–kinase and substrate regulation
KSEA and KSTAR algorithm was used to estimate the kinase activities based on the abundance of phosphosites. KSEA and KSTAR estimate changes in a kinase’s activity by measuring and averaging the amounts of its identified substrates instead of a single substrate, which enhances the signal-to-noise ratio from inherently noisy phosphoproteomics data59.
Cell cycle analysis
Multi-Gene Proliferation Scores (MGPS) were calculated from the normalized RNA-seq data34,35. In our study, MGPS was calculated as the mean expression level of all cell cycle-regulated genes identified by Whitfield et al35. in each sample.
Estimation of stromal and immune scores
The xCell analysis (https://xcell.ucsf.edu/)95were used to infer immune scores based on the RNA-seq data.
TF activity inference
We applied the TF activity inference method provided by Alonso et al.151. This method of the prediction of TF activities from the gene expression of their targets (i.e., TF regulon) was commonly used to characterize the functional status of transcriptional regulatory circuits152. In our study, TF activities for 187 SBC tumors were computed using ssGSEA153 via the GSVA154 package. TF targets obtained from DoRothEA (v1.6.0)151 were set as background.
PROGENy scores
PROGENy100 was used to generate activity scores for EGFR, VEGF, Hypoxia, etc. based on RNA expression data. Tumor RNA expression values were submitted to PROGENy.
Survival analysis
All the survival analysis presented in this manuscript (e.g., OS and PFS of the proteomic and phosphoproteomic sub-types, etc.), were based on Kaplan-Meier survival curves (log-rank test).
Statistics and reproducibility
Quantification methods and statistical analysis methods for proteomic and integrated analyses were mainly described and referenced in the respective subsections. Additionally, standard statistical tests were used to analyze the clinical data, including but not limited to Student’s t-test, Fisher’s exact test, Kruskal-Wallis test, log-rank test. All statistical tests were two-sided, and statistical significance was considered when p-value < 0.05. To account for multiple-testing, the p-values were adjusted using the Benjamini–Hochberg FDR correction. Kaplan–Meier plots (log-rank test) were used to describe overall survival. Variables associated with overall survival were identified using univariate Cox proportional hazards regression models. Statistics used in the manuscript includes moderated t-test, wilcoxon test, One-way ANOVA, Kruskal-Wallis test, Fisher’s exact test, and Log-rank test. All the analyses of clinical data were performed in R and GraphPad Prism. Most of them used broadly applied R packages and others used self-made R scripts according published papers: ConsensusClusterPlus (v1.50.0) for consensus clustering, Hmisc (v4.5-0) for spearman’s correlation calculating, ggplot2 (v3.3.5) for scatter plot, clusterProfiler (v4.0.5) for pathway enrichment analysis. For WES, BWA (Li H et al.), SAMtools (Li H et al.) and Picard (http://broadinstitute.github.io/picard/) were used to genome alignment, and muTect Software (Cibulskis K et al. 2013) was used for targeting Somatic SNV sites, and Strelka was used to test Somatic INDEL information. For RNA-Seq, raw data quality was assessed with the FastQC (v0.11.9) and the adaptor was trimmed with Trim_Galore (version 0.6.6). Reads were mapped by using STAR software (v2.7.7a). The mapped reads were assembled into transcripts or genes by using StringTie software (v2.1.4). For functional experiments, each was repeated at least three times independently, and results were expressed as mean ± standard error of the mean (SEM).
Immunohistochemistry (IHC)
Tumor samples were fixed in 4% paraformaldehyde for 24 h and then embedded in paraffin. Paraffin blocks were cut into 5um sections and used for hematoxylin and eosin (HE), immunohistochemistry (IHC), or Immunofluorescence (IF) staining. For IHC, slides were deparaffinized through xylenes and graded ethanol, then performed antigen retrieval using citrate buffer at pH 6.0. After washing, slides were blocked with 0.3% H2O2 and 5% normal goat serum sequentially, followed by staining with primary antibody at 4°C overnight. Next, slides were incubated with EnVision FLEX/HRP (SM802, DAKO, Glostrup, Denmark) at RT for 20 min, followed by using EnVison FLEX DAB + CHROMOGEM and EnVision FLEX substrate buffr (DM827 and SM803, DAKO, Glostrup, Denmark) to visualize staining signals under light microscopy, finally counterstained using hematoxylin solution. Finally, stained slides were scanned using Ocus (Grundium, Tampere, Finland) and analyzed with Qupath software. The following antibodies were used: Anti-TBXT (ab209665, abcam, 1:2000), anti-ATP5A (ab14748; abcam, 1:1000), anti-MSH2 (ab70270; abcam, 1:500), anti-TOMM20 (42406S; CST, 1:400), and Phospho-Rb (Ser807/811) (8516 T; CST, 1:500).
Immunofluorescence (IF) staining of anaphase bridge
Tumor samples were fixed in 4% paraformaldehyde for 24 h and then embedded in paraffin. Paraffin blocks were cut into 5 μm sections and used for IF staining. For IF, slides were deparaffinized through xylenes and graded ethanol, then performed antigen retrieval using citrate buffer at pH 6.0. First, slides were incubated with primary antibody, Rabbit Anti-ERCC6L (PICH) antibody (bs-6380R, Bioss, 1:100), and Rabbit anti-BLM antibody (HPA005689, Sigma-Aldrich, 1:50) at 4 °C overnight. After washing, slides were immediately covered with 100 μl of the diluted secondary antibody and incubated for 2 h at room temperature and protect from light. Finally, the slides were counterstained with DAPI in an antifade solution (DAPI Fluoromount-G, 0100-20, SouthernBiotech) and then mounted. Images were taken with Leica SP8 confocal microscope.
Functional experiments
Cell culture
The UM‑Chor1 cell line was purchased from the American Type Culture Collection (CRL-3270; ATCC, Manassas, VA, USA). UM‑Chor1 cells were cultured in IMDM: (12440053; Gibco): RPMI-1640 (A1049101; Gibco) 4:1 medium supplemented with 10% FBS (10099141 C; Gibco) and 1% antibiotic mixture (15240062; Gibco). The cells were grown in a humidified 5% CO2 atmosphere at 37 °C. As for the authentication of the cell lines used in the study, the cell line UM-Chor1 was acquired from ATCC (CRL-3270), passage number 5–8. The mycoplasma testing of cell lines used in the study was performed using MycoBlue Mycoplasma Detector (D101-01, vazyme).
Cell transfection
The siRNA sequences of target gene markers were synthesized by GenePharma. Cells were seed in a 6-well plate with a density of 5 × 105 cells/well. After 24 h and 70%–80% confluence, the cells were added with siRNA (50 nM) in serum-free medium using RNAiMAX (13778030; Invitrogen) per manufacturer’s instructions. After incubation for 20 min at RT, the medium in each well was then changed with complete medium with 10% heat-inactivated fetal bovine serum for another 48 h.
Radiation of cell lines
Seeded onto 6-well plates were 3 × 105 UM‑Chor1 cells. Once cells reached 90% confluence, cells were irradiated by using a special platform (Small animal radiation research platform, SARRP, Gulmay Medical Co., Ltd), with the following parameters: 3.845 Gy/min at 220 kV, 13 mA; the source-to-skin distance (SSD) for a fixed fluoroscopy unit was 35 cm, and the irradiation area was 15 cm × 15 cm. Cells were exposed to irradiation or normal control. Then cells were observed for 48 h and the culture medium was changed with the cells washed 3 times in serum-free medium.
CIN induction experiment
The CIN + SBC cells were achieved through the following steps: (1). The SBC cell line (UM-Chor1) was treated with cytarabine at a concentration of 10 nM and cultured for 3 days. (2). The treated cells were then planted into a 10 cm dish for 7 days. (3). After 7 days of culture, monoclonal selection was performed to sort different monoclonal cells. (4). The monoclonal cells were individually amplified and passaged for subsequent experiments. (5). The CIN status of these monoclonal cells was determined through three approaches: WES analysis, FISH analysis, and LC-MS/MS analysis. After amplification and passage, WES was conducted on different UM-Chor1 monoclonal cells and control cells separately. We calculated the CIN score of these monoclonal cells and analyzed their CNA events based on WES data. The results revealed that monoclonal cell lines treated with cytarabine had significantly higher CIN scores compared to the control cells without treatment of cytarabine (Supplementary Fig. 22A). We identified arm-level CNAs, such as 1q gain (Cell line I), 9p loss (Cell line II) and 10q loss (Cell line III), in treated cell lines (Supplementary Fig. 22B). Then, FISH analysis were performed to illustrate the 1q gain, 9p loss and 10q loss in these monoclonal cells using GSP 1q21/ 1p36 probe GSP 9p21/ CSP 9 probe and GSP 10q23/ CSP 10 probe, respectively (Supplementary Fig. 22C–H). We evaluated two hundred non-overlapping tumor nuclei from each sample. In treated cell line I, the percentage of cells with 1 q gain (75%) was significantly higher than the control (3%) (Supplementary Fig. 22D). Similarly, in cell line II, the percentage of cells with 9p loss (89%) was notably higher compared to its corresponding control (3%) (Supplementary Fig. 22F). Additionally, in cell line III, the percentage of cells with 10q loss (77%) was also considerably higher than the control (5%) (Supplementary Fig. 22H). These results revealed that the treated cell line I showed 1q gain, cell line II showed 9p loss, and cell line III had 10q loss event. The FISH results were consistent with the findings based on WES data. We also conducted proteomic profiling on control UM-Chor1 cells and UM-Chor1 monoclonal cells treated with cytarabine using LC-MS/MS (Supplementary Fig. 22I-L). These results confirmed molecular features of the upregulation or downregulation of related proteins and pathways in these monoclonal cells were consistent with their arm-level CNAs observed by the analysis of WES and FISH.
Fluorescence in situ hybridization (FISH) assay
FISH for chromosome 1q gain was performed using commercial 1q21/1p36 probes (GSP 1q21, Anbiping company, Guangzhou, China) on FFPE sections (3 μm) to manufacturers’ instructions. FISH for chromosome 9p loss and 10q loss was performed using commercial 9p21/ CSP 9 probe and 10q23/ CSP 10 probe respectively (GSP 9p21 and GSP 10q23, Anbiping company, Guangzhou, China) on FFPE sections (3μm). Two hundred nonoverlapping tumor nuclei were evaluated.
Western blotting
Proteins were extracted by SDS cell lysis buffer (P0013G; Beyotime) supplemented with protease inhibitor cocktail (87785; Thermo Scientific). Protein quantification was measured by the Pierce BCA protein assay kit (23225; Thermo Fisher Scientific). The protein bands were detected by conventional protocols for western blotting. Proteins were detected by using specific primary antibodies against secondary antibodies (Cell Signaling Technology, 1:2000). The following antibodies were used: monoclonal anti-GAPDH (ab181602, 1:4000; abcam), monoclonal anti-alpha tubulin (PTM-5442, 1:2000; ptmbiolabs), anti-rabbit IgG (7074, 1:2000; Cell Signaling Technology), and anti-mouse IgG (7076, 1:2000; Cell Signaling Technology), anti-RPRD1B (GTX119969, 1:1000; GeneTex).
Quantitative RT-PCR
Total RNA was extracted from tissue samples and cells using TRIzol reagent (15596018; Invitrogen) after washing with PBS. cDNA was synthesized from purified RNA using a SuperScript III First-Strand cDNA synthesis system (18080051; Invitrogen) according to the manufacturer’s instructions. SYBR Green PCR Master Mix (Q331-02; Vazyme) was used for PCR amplification and a real-time PCR machine (iQ5, Bio-Rad Laboratories) was used to quantify the expression of mRNAs. GAPDH was used as endogenous control and the expression levels were quantified using 2 − ∆∆Ct method. The qPCR primers sequences are as follows:
HSPD1 forward:5’- ATGCTTCGGTTACCCACAGTC −3’
HSPD1 reverse:5’- AGCCCGAGTGAGATGAGGAG-3’
HSPE1 forward:5’- ATGGCAGGACAAGCGTTTAGA-3’
HSPE1 reverse:5’- TGGAAGCATAATGCCTCCTTTG-3’
DNAJA3 forward:5’- TCACCCTGACACAAATAAGGATG −3’
DNAJA3 reverse:5’- AGGATGAGAACTCGCCAAAGAT −3’
RPRD1B forward:5’- GGCAAGAACGAAGTGTGTATGG −3’
RPRD1B reverse:5’- CTGCCAGGGTAGTCGTCATC −3
GAPDH forward:5’- GGAGCGAGATCCCTCCAAAAT −3’
GAPDH reverse:5’- GGCTGTTGTCATACTTCTCATGG −3’
ACTB forward:5’- CATGTACGTTGCTATCCAGGC −3’
ACTB reverse:5’- CTCCTTAATGTCACGCACGAT −3’
Analysis of cell proliferation
To test the cell viability, a total of 3 × 103 cells were plated into 96-well plate cells. The following day, 100 μl of fresh medium containing the corresponding concentration of various inhibitors was added to each well to replace the growth medium for 72 h drug exposure. Cell Counting Kit-8 (Yeasen, #40203ES92) was used to estimate the cell inhibition with the absorbance at 450 nm (A450).
Cell cycle and apoptosis assay
UM-Chor1 cells were seeded at a concentration of 1 × 106 cells/well in a 6-well plate. For the cell cycle assay, cells were collected and re-suspended in 70% ethanol overnight at 4 °C. Then, the samples were washed with PBS and stained with propidium iodide (PI, Cat. No. A211-01, Vazyme Biotech) for 30 min at room temperature. For the apoptosis assay, cells were incubated with a FITC-labeled annexin V and propidium iodide for 10 min. BD FACSCalibur (BD Pharmingen) was applied to analyze the cell cycle phase distribution and apoptosis according to the manufacturer’s protocol.
Cell viability assay
The CellTiter-Glo Luminescent Cell Viability Assay43 was used to detect the survival cells. CIN+ and the control cells were planted into 6-well plates with 3000 cells per well, separately. We assessed cell viability every 2 days using the CellTiter-Glo Luminescent Cell Viability Assay.
Patient-derived primary cells
The patient-derived primary cells were obtained through the following steps: The patient samples were cut into pieces of 1 mm in diameter. Then the samples were dissociated using a Human Tumor Dissociation Kit (Miltenyi Biotec, Bergisch Gladbach, Germany) per manufacturer guidelines. Cell suspensions were filtered using a 70 μm filter (Thermo Fisher Scientific), and dissociated cells were planted into 6 cm dished with IMDM: 1640 4:1 medium supplemented with 10% FBS for culture and following experiments.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium (https://proteomecentral.proteomexchange.org) via the iProX partner repository155,156 with the dataset identifier PXD053550 (http://www.iprox.org/page/project.html?id=IPX0005448000). The raw WES data and Transcriptomic data have been deposited in the National Genomics Data Center (GSA) database (https://ngdc.cncb.ac.cn/gsub/) under accession code HRA005316. The raw sequencing data are available under controlled access due to data privacy laws related to patient consent for data sharing and the data should be used for research purposes only. Access can be obtained by approval via their respective DAC (Data Access Committees) in the GSA-human database. According to the guidelines of GSA-human, all non-profit researchers are allowed access to the data and the Principle Investigator of any research group is allowed to apply for Controlled access of the data. The user can register and login to the GSA database website (https://ngdc.cncb.ac.cn/gsa-human/) and follow the guidance of “Request Data” to request the data step by step (https://ngdc.cncb.ac.cn/gsa-human/document). The approximate response time for accession requests is about 2 weeks. The access authority can be obtained for Research Use Only. The user can also contact the corresponding author directly. Once access has been granted, the data will be available to download for 3 months. The remaining data are available within the Article, Supplementary Information, or Source Data file. The human reference genome (GRCh38.p13 assembly) was downloaded from NCBI. The information of kinase-substrate relationships were available in PhosphoSite [https://www.phosphosite.org/homeAction.action]157, Phos-pho.ELM [http://phospho.elm.eu.org/dataset.html]158, and PhosphoPOINT [http://kinase.bioinformatics.tw/]159. Source data are provided with this paper.
References
Walcott, B. P. et al. Chordoma: current concepts, management, and future directions. Lancet Oncol. 13, e69–e76 (2012).
Crockard, H. A. et al. A multidisciplinary team approach to skull base chordomas. J. Neurosurg. 95, 175–183 (2001).
Santegoeds, R. G. C. et al. Ectopic recurrence of skull base chordoma after proton therapy. Curr. Oncol. 29, 2364–2375 (2022).
Stacchiotti, S. & Sommer, J. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 16, e71–e83 (2015).
Groschel, S. et al. Defective homologous recombination DNA repair as therapeutic target in advanced chordoma. Nat. Commun. 10, 1635 (2019).
Cahill, J. et al. Gamma knife stereotactic radiosurgery for the treatment of chordomas and chondrosarcomas. Acta Neurochir. (Wien) 163, 1003–1011 (2021).
Tarpey, P. S. et al. The driver landscape of sporadic chordoma. Nat. Commun. 8, 890 (2017).
Yang, X. R. et al. T (brachyury) gene duplication confers major susceptibility to familial chordoma. Nat. Genet. 41, 1176–1178 (2009).
Drews, R. M. et al. A pan-cancer compendium of chromosomal instability. Nature 606, 976–983 (2022).
Steele, C. D. et al. Signatures of copy number alterations in human cancer. Nature 606, 984–991 (2022).
Song, T. et al. Integrative identification by Hi-C revealed distinct advanced structural variations in lung adenocarcinoma tissue. Phenomics 3, 390–407 (2023).
Ott, M., Prins, R. M. & Heimberger, A. B. The immune landscape of common CNS malignancies: implications for immunotherapy. Nat. Rev. Clin. Oncol. 18, 729–744 (2021).
Bai, J. W. et al. Mid-term follow-up surgical results in 284 cases of clival chordomas: the risk factors for outcome and tumor recurrence. Neurosurg. Rev. 45, 1451–1462 (2022).
Sanusi, O., Arnaout, O., Rahme, R. J., Horbinski, C. & Chandler, J. P. Surgical resection and adjuvant radiation therapy in the treatment of skull base chordomas. World Neurosurg. 115, e13–e21 (2018).
Wang, B., Tian, F. & Tong, X. Clinical grading system, surgical outcomes and prognostic analysis of cranial base chordomas. J. Korean Neurosurg. Soc. 65, 469–478 (2022).
Bai, J. et al. Whole genome sequencing of skull-base chordoma reveals genomic alterations associated with recurrence and chordoma-specific survival. Nat. Commun. 12, 757 (2021).
Le, L. P. et al. Recurrent chromosomal copy number alterations in sporadic chordomas. PLoS ONE 6, e18846 (2011).
Diaz, R. J. et al. High-resolution whole-genome analysis of skull base chordomas implicates FHIT loss in chordoma pathogenesis. Neoplasia 14, 788–U141 (2012).
Scheil, S. et al. Genome-wide analysis of sixteen chordomas by comparative genomic hybridization and cytogenetics of the first human chordoma cell line. U CHI. Gene Chromosome Canc. 32, 203–211 (2001).
Lukow, D. A. et al. Chromosomal instability accelerates the evolution of resistance to anti-cancer therapies. Dev. Cell 56, 2427–2439 e2424 (2021).
Dong, L. Q. et al. Spatial and temporal clonal evolution of intrahepatic cholangiocarcinoma. J. Hepatol. 69, 89–98 (2018).
Lepage, C. C., Morden, C. R., Palmer, M. C. L., Nachtigal, M. W. & McManus, K. J. Detecting chromosome instability in cancer: approaches to resolve cell-to-cell heterogeneity. Cancers (Basel) 11, 226 (2019).
Biermann, J. et al. Dissecting the treatment-naive ecosystem of human melanoma brain metastasis. Cell 185, 2591–2608.e30 (2022).
Chen, J. et al. A complete telomere-to-telomere assembly of the maize genome. Nat. Genet. 55, 1221–1231 (2023).
Mao, Y. F. & Zhang, G. J. A complete, telomere-to-telomere human genome sequence presents new opportunities for evolutionary genomics. Nat. Methods 19, 635–638 (2022).
Tang, G. L. et al. Cytogenetic profile in monoclonal gammopathy of undetermined significance, smoldering and symptomatic multiple myeloma: a study of 1087 patients with highly purified plasma cells. Cancers 15, 5690 (2023).
Brat, D. J. et al. Analysis of 1p, 19q, 9p, and 10q as prognostic markers for high-grade astrocytomas using fluorescence in situ hybridization on tissue microarrays from radiation therapy oncology group trials. Neuro Oncol. 6, 96–103 (2004).
Casorzo, L. et al. Fluorescence hybridization (FISH) evaluation of chromosomes 6, 7, 9 and 10 throughout human melanocytic tumorigenesis. Melanoma Res. 15, 155–160 (2005).
Vital, A. L. et al. Intratumoral patterns of clonal evolution in gliomas. Neurogenetics 11, 227–239 (2010).
Krupina, K., Goginashvili, A. & Cleveland, D. W. Causes and consequences of micronuclei. Curr. Opin. Cell Biol. 70, 91–99 (2021).
Chan, Y. W., Fugger, K. & West, S. C. Unresolved recombination intermediates lead to ultra-fine anaphase bridges, chromosome breaks and aberrations. Nat. Cell Biol. 20, 92–103 (2018).
Chmielewska, M. et al. The programmed DNA elimination and formation of micronuclei in germ line cells of the natural hybridogenetic water frog. Sci. Rep. Uk 8, 7870 (2018).
Ranieri, M. et al. Green olive leaf extract (OLE) provides cytoprotection in renal cells exposed to low doses of cadmium. PLoS ONE 14, e0214159 (2019).
Ellis, M. J. et al. Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the American college of surgeons oncology group Z1031 trial (Alliance). J. Clin. Oncol. 35, 1061–1069 (2017).
Whitfield, M. L. et al. Identification of genes periodically expressed in the human cell cycle and their expression in tumors. Mol. Biol. Cell 13, 1977–2000 (2002).
Whitfield, M. L., George, L. K., Grant, G. D. & Perou, C. M. Common markers of proliferation. Nat. Rev. Cancer 6, 99–106 (2006).
Yuan, J. Z. et al. Single-cell transcriptome analysis of lineage diversity in high-grade glioma. Genome Med. 10, 57 (2018).
Petralia, F. et al. Integrated proteogenomic characterization across major histological types of pediatric brain cancer. Cell 183, 1962–1985.e31 (2020).
Wang, D. et al. A novel PLK1 inhibitor onvansertib effectively sensitizes MYC-driven medulloblastoma to radiotherapy. Neuro Oncol. 24, 414–426 (2022).
Ben-David, U. & Amon, A. Context is everything: aneuploidy in cancer. Nat. Rev. Genetics 21, 44–62 (2020).
Carter, S. L., Eklund, A. C., Kohane, I. S., Harris, L. N. & Szallasi, Z. A signature of chromosomal instability inferred from gene expression profiles predicts clinical outcome in multiple human cancers. Nat. Genetics 38, 1043–1048 (2006).
Davoli, T. et al. Cumulative haploinsufficiency and triplosensitivity drive aneuploidy patterns and shape the cancer genome. Cell 155, 948–962 (2013).
Wang-Bishop, L. et al. Inhibition of AURKA reduces proliferation and survival of gastrointestinal cancer cells with activated KRAS by preventing activation of RPS6KB1. Gastroenterology 156, 662–675.e7 (2019).
Burrell, R. A. et al. Replication stress links structural and numerical cancer chromosomal instability. Nature 494, 492–496 (2013).
Gordon, D. J., Resio, B. & Pellman, D. Causes and consequences of aneuploidy in cancer. Nat Rev Genet 13, 189–203 (2012).
Clark, D. J. et al. Integrated proteogenomic characterization of clear cell renal cell carcinoma. Cell 179, 964–983.e31 (2019).
Gaillard, H., Garcia-Muse, T. & Aguilera, A. Replication stress and cancer. Nat Rev Cancer 15, 276–289 (2015).
da Costa, A. A. B. A., Chowdhury, D., Shapiro, G. I., D’Andrea, A. D. & Konstantinopoulos, P. A. Targeting replication stress in cancer therapy. Nat. Rev. Drug Discov. 22, 38–58 (2023).
Msaouel, P. et al. Comprehensive molecular characterization identifies distinct genomic and immune hallmarks of renal medullary carcinoma. Cancer Cell 37, 720–734.e13 (2020).
Dreyer, S. B. et al. Targeting DNA damage response and replication stress in pancreatic cancer. Gastroenterology 160, 362–377.e13 (2021).
Saxena, S. & Zou, L. Hallmarks of DNA replication stress. Mol. Cell 82, 2298–2314 (2022).
Macheret, M. & Halazonetis, T. D. DNA replication stress as a hallmark of cancer. Annu. Rev. Pathol. 10, 425–448 (2015).
Hsu, C. L., Chong, S. Y., Lin, C. Y. & Kao, C. F. Histone dynamics during DNA replication stress. J. Biomed. Sci. 28, 48 (2021).
Papamichos-Chronakis, M. & Peterson, C. L. Chromatin and the genome integrity network. Nat. Rev. Genet. 14, 62–75 (2013).
Zhang, J., Dai, Q., Park, D. & Deng, X. Targeting DNA replication stress for cancer therapy. Genes (Basel) 7, 51 (2016).
Kent, L. N. & Leone, G. The broken cycle: E2F dysfunction in cancer. Nat. Rev. Cancer 19, 326–338 (2019).
Bertoli, C., Herlihy, A. E., Pennycook, B. R., Kriston-Vizi, J. & de Bruin, R. A. M. Sustained E2F-dependent transcription is a key mechanism to prevent replication-stress-induced DNA damage. Cell Rep. 15, 1412–1422 (2016).
Malumbres, M. & Barbacid, M. Cell cycle, CDKs and cancer: a changing paradigm. Nat. Rev. Cancer 9, 153–166 (2009).
Crowl, S., Jordan, B. T., Ahmed, H., Ma, C. X. & Naegle, K. M. KSTAR: An algorithm to predict patientspecific kinase activities from phosphoproteomic data. Nat. Commun. 13, 32017–5 (2022).
Middleton, G. et al. The national lung matrix trial of personalized therapy in lung cancer. Nature 583, 807–812 (2020).
Aguda, B. D. Kick-starting the cell cycle: from growth-factor stimulation to initiation of DNA replication. Chaos 11, 269–276 (2001).
Tenca, P. et al. Cdc7 is an active kinase in human cancer cells undergoing replication stress. J. Biol. Chem. 282, 208–215 (2007).
Sato, N. et al. Cell cycle regulation of chromatin binding and nuclear localization of human Cdc7-ASK kinase complex. Genes Cells 8, 451–463 (2003).
Masai, H. et al. Human Cdc7-related kinase complex -: phosphorylation of MCM by concerted actions of Cdks and Cdc7 and that of a critical threonine residue of Cdc7 by Cdks. J. Biol. Chem. 275, 29042–29052 (2000).
Liu, T. et al. CDK4 expression in chordoma: a potential therapeutic target. J. Orthop. Res. 36, 1581–1589 (2018).
Hopp, A. K. et al. Mitochondrial NAD(+) controls nuclear ARTD1-Induced ADP-Ribosylation. Mol. Cell 81, 340–354 e345 (2021).
Baker, M. J., Frazier, A. E., Gulbis, J. M. & Ryan, M. T. Mitochondrial protein-import machinery: correlating structure with function. Trends Cell Biol. 17, 456–464 (2007).
Rath, S. et al. MitoCarta3.0: an updated mitochondrial proteome now with sub-organelle localization and pathway annotations. Nucleic Acids Res. 49, D1541–D1547 (2021).
Schulte, U. et al. Mitochondrial complexome reveals quality-control pathways of protein import. Nature 614, 153 (2023).
Ruan, L. H. et al. Mitochondria-associated proteostasis. Annu. Rev. Biophys. 49, 41–67 (2020).
Antonicka, H. et al. A high-density human mitochondrial proximity interaction network. Cell Metab. 32, 479 (2020).
Shpilka, T. & Haynes, C. M. The mitochondrial UPR: mechanisms, physiological functions and implications in ageing. Nat. Rev. Mol. Cell Biol. 19, 109–120 (2018).
Shabashvili, D. E., Feng, Y., Kaur, P., Venugopal, K. & Guryanova, O. A. Combination strategies to promote sensitivity to cytarabine-induced replication stress in acute myeloid leukemia with and without DNMT3A mutations. Exp. Hematol. 110, 20–27 (2022).
Martínez-Reyes, I. & Chandel, N. S. Cancer metabolism: looking forward. Nat. Rev. Cancer 21, 669–680 (2021).
Faubert, B., Solmonson, A. & DeBerardinis, R. J. Metabolic reprogramming and cancer progression. Science 368, 152 (2020).
Wilke, A. C. et al. SHMT2 inhibition disrupts the TCF3 transcriptional survival program in Burkitt lymphoma. Blood 139, 538–553 (2022).
Stacchiotti, S. et al. Best practices for the management of local-regional recurrent chordoma: a position paper by the chordoma global consensus group. Ann. Oncol. 28, 1230–1242 (2017).
Jiang, Y. Z. et al. Genomic and transcriptomic landscape of triple-negative breast cancers: subtypes and treatment strategies. Cancer Cell 35, 428–440.e5 (2019).
Li, Y. et al. Proteomic characterization of gastric cancer response to chemotherapy and targeted therapy reveals new therapeutic strategies. Nat. Commun. 13, 5723 (2022).
Huang, R. X. & Zhou, P. K. DNA damage response signaling pathways and targets for radiotherapy sensitization in cancer. Signal Transduct. Target Ther. 5, 60 (2020).
Huang, R. X. & Zhou, P. K. DNA damage repair: historical perspectives, mechanistic pathways and clinical translation for targeted cancer therapy. Signal Transduct. Target Ther. 6, 254 (2021).
Castle, K. D. & Kirsch, D. G. Establishing the impact of vascular damage on tumor response to high-dose radiation therapy. Cancer Res. 79, 5685–5692 (2019).
Favaudon, V. et al. Ultrahigh dose-rate FLASH irradiation increases the differential response between normal and tumor tissue in mice. Sci. Transl. Med. 6, 245ra93 (2014).
Knijnenburg, T. A. et al. Genomic and molecular landscape of DNA damage repair deficiency across the cancer genome atlas. Cell Rep. 23, 239–254 e236 (2018).
Motea, E. A. et al. Kub5-Hera (RPRD1B) deficiency promotes “BRCAness” and vulnerability to PARP inhibition in BRCA-proficient breast cancers. Clin. Cancer Res. 24, 6459–6470 (2018).
Li, M., Ma, D. & Chang, Z. Current understanding of CREPT and p15RS, carboxy-terminal domain (CTD)-interacting proteins, in human cancers. Oncogene 40, 705–716 (2021).
Patidar, P. L. et al. The Kub5-Hera/RPRD1B interactome: a novel role in preserving genetic stability by regulating DNA mismatch repair. Nucleic Acids Res .44, 1718–1731 (2016).
Labib, K. How do Cdc7 and cyclin-dependent kinases trigger the initiation of chromosome replication in eukaryotic cells? Genes Dev. 24, 1208–1219 (2010).
Aran, D., Hu, Z. & Butte, A. J. xCell: digitally portraying the tissue cellular heterogeneity landscape. Genome Biol. 18, 220 (2017).
Dou, Z. et al. Cytoplasmic chromatin triggers inflammation in senescence and cancer. Nature 550, 402–406 (2017).
Santaguida, S. et al. Chromosome mis-segregation generates cell-cycle-arrested cells with complex karyotypes that are eliminated by the immune system. Dev. Cell 41, 638–651 e635 (2017).
Sheltzer, J. M. et al. Single-chromosome gains commonly function as tumor suppressors. Cancer Cell 31, 240–255 (2017).
Bakhoum, S. F. & Cantley, L. C. The multifaceted role of chromosomal instability in cancer and its microenvironment. Cell 174, 1347–1360 (2018).
Liu, T., Zhang, L., Joo, D. & Sun, S. C. NF-kappaB signaling in inflammation. Signal Transduct. Target Ther. 2, 17023 (2017).
Taniguchi, K. & Karin, M. NF-kappaB, inflammation, immunity and cancer: coming of age. Nat. Rev. Immunol. 18, 309–324 (2018).
Cha, E., Wallin, J. & Kowanetz, M. PD-L1 inhibition with MPDL3280A for solid tumors. Semin. Oncol. 42, 484–487 (2015).
Traylor, J. I., Pernik, M. N., Plitt, A. R., Lim, M. & Garzon-Muvdi, T. Immunotherapy for chordoma and chondrosarcoma: current evidence. Cancers 13, 2408 (2021).
Wang, X. et al. Immunotherapy as a promising option for the treatment of advanced chordoma: a systemic review. Cancers 15, 264 (2023).
Ishimura, H. et al. N-acetylglucosaminyltransferase V and β1-6 branching-linked oligosaccharides are associated with good prognosis of patients with bladder cancer. Clin. Cancer Res. 12, 2506–2511 (2006).
Schubert, M. et al. Perturbation-response genes reveal signaling footprints in cancer gene expression. Nat. Commun. 9, 20 (2018).
Dolcet, X., Llobet, D., Pallares, J. & Matias-Guiu, X. NF-kB in development and progression of human cancer. Virchows Arch. 446, 475–482 (2005).
Maiuri, M. C., Zalckvar, E., Kimchi, A. & Kroemer, G. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat. Rev. Mol. Cell Biol. 8, 741–752 (2007).
Oikonomou, E. & Pintzas, A. The TRAIL of oncogenes to apoptosis. Biofactors 39, 343–354 (2013).
Taciak, B., Pruszynska, I., Kiraga, L., Bialasek, M. & Krol, M. Wnt signaling pathway in development and cancer. J. Physiol. Pharmacol. https://doi.org/10.26402/jpp.2018.2.07 (2018).
Clarke, N., Jimenez-Lara, A. M., Voltz, E. & Gronemeyer, H. Tumor suppressor IRF-1 mediates retinoid and interferon anticancer signaling to death ligand TRAIL. EMBO J. 23, 3051–3060 (2004).
Papageorgiou, A., Dinney, C. P. & McConkey, D. J. Interferon-alpha induces TRAIL expression and cell death via an IRF-1-dependent mechanism in human bladder cancer cells. Cancer Biol. Ther. 6, 872–879 (2007).
Ding, L. et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature 481, 506–510 (2012).
Morrissy, A. S. et al. Divergent clonal selection dominates medulloblastoma at recurrence. Nature 529, 351–357, (2016).
Thompson, S. L. & Compton, D. A. Chromosomes and cancer cells. Chromosome Res. 19, 433–444 (2011).
Arlt, M. F. et al. Replication stress induces genome-wide copy number changes in human cells that resemble polymorphic and pathogenic variants. Am. J. Hum. Genet. 84, 339–350 (2009).
Liu, G. D. et al. E2F3 promotes liver cancer progression under the regulation of circ-PRKAR1B. Mol. Ther.Nucl Acids 26, 104–113 (2021).
Jusino, S. et al. E2F3 drives the epithelial-to-mesenchymal transition, cell invasion, and metastasis in breast cancer. Exp. Biol. Med. 246, 2057–2071 (2021).
Wu, L. et al. Expression and prognostic value of E2F3 transcription factor in non-small cell lung cancer. Oncol. Lett. 21, 411 (2021).
Lee, J. M., Heo, M. J., Lee, C. G., Yang, Y. M. & Kim, S. G. Increase of miR-199a-5p by protoporphyrin IX, a photocatalyzer, directly inhibits E2F3, sensitizing mesenchymal tumor cells to anti-cancer agents. Oncotarget 6, 3918–3931 (2015).
Bhattacharya, A. et al. Transcriptional effects of copy number alterations in a large set of human cancers. Nat. Commun. 11, 715 (2020).
Davoli, T., Uno, H., Wooten, E. C. & Elledge, S. J. Tumor aneuploidy correlates with markers of immune evasion and with reduced response to immunotherapy. Science 355, eaaf8399 (2017).
Rajkumar, S. V. & Kumar, S. Multiple myeloma current treatment algorithms. Blood Cancer J. 10, 94 (2020).
Fabris, V. T. From chromosomal abnormalities to the identification of target genes in mouse models of breast cancer. Cancer Genet. 207, 233–246 (2014).
DeSisto, J. et al. Comprehensive molecular characterization of pediatric radiation-induced high-grade glioma. Nat. Commun. 12, 5531 (2021).
Mohanraj, K., Nowicka, U. & Chacinska, A. Mitochondrial control of cellular protein homeostasis. Biochem. J. 477, 3033–3054 (2020).
Zong, W. X., Rabinowitz, J. D. & White, E. Mitochondria and cancer. Mol. Cell 61, 667–676 (2016).
Tang, L. et al. Role of metabolism in cancer cell radioresistance and radiosensitization methods. J. Exp. Clin. Cancer Res. 37, 87 (2018).
Dokic, I. et al. High resistance to X-rays and therapeutic carbon ions in glioblastoma cells bearing dysfunctional ATM associates with intrinsic chromosomal instability. Int. J. Radiat Biol. 91, 157–165 (2015).
Kinsella, T. J. Coordination of DNA mismatch repair and base excision repair processing of chemotherapy and radiation damage for targeting resistant cancers. Clin. Cancer Res. 15, 1853–1859 (2009).
Vens, C. & Begg, A. C. Targeting base excision repair as a sensitization strategy in radiotherapy. Semin. Radiat. Oncol. 20, 241–249 (2010).
Zhu, Y., Hu, J., Hu, Y. & Liu, W. Targeting DNA repair pathways: a novel approach to reduce cancer therapeutic resistance. Cancer Treat. Rev. 35, 590–596 (2009).
Han, G. et al. 9p21 loss confers a cold tumor immune microenvironment and primary resistance to immune checkpoint therapy. Nat. Commun. 12, 5606 (2021).
Matsuyama, H. et al. Clinical significance of chromosome 8p, 10q and 16q deletions in prostate cancer. Prostate 54, 103–111 (2003).
Ohgaki, H. Genetic pathways to glioblastomas. Neuropathology 25, 1–7 (2005).
Qu, Y. Y. et al. A proteogenomic analysis of clear cell renal cell carcinoma in a Chinese population. Nat. Commun. 13, 2052 (2022).
Sun, M. et al. Proteomic characterization identifies clinically relevant subgroups of gastrointestinal stromal tumors. Gastroenterology 166, 450–465.e433 (2024).
Marusak, C. et al. Targeting extracellular matrix remodeling restores BRAF inhibitor sensitivity in BRAFi-resistant melanoma. Clin. Cancer Res. 26, 6039–6050 (2020).
Jiang, Y. F. et al. Targeting extracellular matrix stiffness and mechanotransducers to improve cancer therapy. J. Hematol. Oncol. 15, 34 (2022).
Sommer, J. et al. Methylthioadenosine phosphorylase and activated insulin-like growth factor-1 receptor/insulin receptor: potential therapeutic targets in chordoma. J. Pathol. 220, 608–617 (2010).
Northcott, P. A. et al. The whole-genome landscape of medulloblastoma subtypes. Nature 547, 311 (2017).
Cho, W. K. et al. Liquid biopsy using cfDNA to predict radiation therapy response in solid tumors. Radiat. Oncol. J. 41, 32–39 (2023).
Zhang, Q. L. et al. Single-cell transcriptome reveals cellular hierarchies and guides p-EMT-targeted trial in skull base chordoma. Cell Discov. 8, 94 (2022).
Zuccato, J. A. et al. DNA methylation-based prognostic subtypes of chordoma tumors in tissue and plasma. Neuro Oncology. 24, 442–454 (2022).
Li, X. et al. Identification of TNFRSF21 as an inhibitory factor of osteosarcoma based on a necroptosis-related prognostic gene signature and molecular experiments. Cancer Cell Int. 24, 14 (2024).
Lei, T., Qian, H., Lei, P. F. & Hu, Y. H. Ferroptosis-related gene signature associates with immunity and predicts prognosis accurately in patients with osteosarcoma. Cancer Sci. 112, 4785–4798 (2021).
Carter, S. L. et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 30, 413–421 (2012).
Hristov, B. H. & Singh, M. Network-based coverage of mutational profiles reveals cancer genes. Cell Syst. 5, 221–229 e224 (2017).
Ellrott, K. et al. Scalable open science approach for mutation calling of tumor exomes using multiple genomic pipelines. Cell Syst. 6, 271–281.e7 (2018).
Mermel, C. H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, r41 (2011).
Wisniewski, J. R., Zougman, A., Nagaraj, N. & Mann, M. Universal sample preparation method for proteome analysis. Nat. Methods 6, 359–U360 (2009).
Feng, J. et al. Firmiana: towards a one-stop proteomic cloud platform for data processing and analysis. Nat. Biotechnol. 35, 409–412 (2017).
Krug, K. et al. Proteogenomic landscape of breast cancer tumorigenesis and targeted therapy. Cell 183, 1436 (2020).
Satpathy, S. et al. A proteogenomic portrait of lung squamous cell carcinoma. Cell 184, 4348 (2021).
Xu, J. Y. et al. Integrative proteomic characterization of human lung adenocarcinoma. Cell 182, 245 (2020).
Jiang, Y. et al. Proteomics identifies new therapeutic targets of early-stage hepatocellular carcinoma. Nature 567, 257 (2019).
Garcia-Alonso, L., Holland, C. H., Ibrahim, M. M., Turei, D. & Saez-Rodriguez, J. Benchmark and integration of resources for the estimation of human transcription factor activities. Genome Res. 29, 1363–1375 (2019).
Essaghir, A. et al. Transcription factor regulation can be accurately predicted from the presence of target gene signatures in microarray gene expression data. Nucleic Acids Res. 38, e120 (2010).
Barbie, D. A. et al. Systematic RNA interference reveals that oncogenic-driven cancers require TBK1. Nature 462, 108–U122 (2009).
Hänzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-Seq data. Bmc Bioinform. 14, 7 (2013).
Chen, T. et al. iProX in 2021: connecting proteomics data sharing with big data. Nucleic Acids Res. 50, D1522–D1527 (2022).
Ma, J. et al. iProX: an integrated proteome resource. Nucleic Acids Res. 47, D1211–D1217 (2019).
Hornbeck, P. V., Chabra, I., Kornhauser, J. M., Skrzypek, E. & Zhang, B. Phosphosite: A bioinformatics resource dedicated to physiological protein phosphorylation. Proteomics 4, 1551–1561 (2004).
Diella, F., Gould, C. M., Chica, C., Via, A. & Gibson, T. J. Phospho.ELM: a database of phosphorylation sites - update 2008. Nucleic Acids Res. 36, D240–D244 (2008).
Yang, C. Y. et al. PhosphoPOINT: a comprehensive human kinase interactome and phospho-protein database. Bioinformatics 24, I14–I20 (2008).
Acknowledgements
This work is supported by National Key Research and Development Program of China (2022YFA1303200 [C.D.], 2022YFA1303201 [C.D.], 2018YFA0507500 [Q.Z.], 2018YFA0507501 [Q.Z.], and 2017YFC0908404 [Q.Z.]), National Natural Science Foundation of China (32330062 [C.D.], 31972933 [C.D.], 32201212 [Y.Z.W.], 32471498 [Y.Z.W.], 32201215 [J.W.F.], U21A20389 [Y.Z.], U21A20389 [Y.Z.], 82073640 [N.Q.], and 82373119 [Q.Z.]), sponsored by Program of Shanghai Academic/Technology Research Leader (22XD1420100 [C.D.]), the Major Project of Special Development Funds of Zhangjiang National Independent Innovation Demonstration Zone (ZJ2019-ZD-004 [C.D.]), Shanghai Municipal Science and Technology Major Project (2023SHZDZX02 [C.D.]), the Fudan Original Research Personalized Support Project [C.D.], CAMS Innovation Fund for Medical Sciences (CIFMS) (2019-12M-5-063 [F.C.H.], 2021-I2M-C&T-A-025 [Y.Z.], and 2023-I2M-C&T-B-125 [Y. Wang]), the China Pituitary Adenoma Specialist Council (CPASC) to Y.Z., the National High Technology Research and Development Program of China (863 program, 2014AA020611 to Y.Z.), the Chang Jiang Scholars Program to Y.Z., the National Program for Support of Top-Notch Young Professionals to Y.Z., the National Science Fund for Distinguished Young Scholars (81725011 [Y.Z.]), Clinical Research Plan of SHDC (SHDC2020CR2004A [Y.Z.]), Clinical Research Plan of SHDC (2020CR2004A [Y.Z.]), supported by National Key Research and Development Program of China (2023YFC2505900 [J.W.F.]), sponsored by Shanghai Sailing Program (22YF1403100 [J.W.F.]), and a Cancer Research Institute/Chordoma Foundation CLIP Grant (CRI5105 [Q.Z.]). This work is supported by Shanghai Municipal Science and Technology Major Project and the Human Phenome Data Center of Fudan university.
Author information
Authors and Affiliations
Contributions
Q.Z. provided expertise and feedback, contributed to the analysis, and wrote the manuscript. Z.X. performed experiments, conducted formal analysis and wrote the manuscript. R.Ha. provided expertise and feedback, conducted validation experiments and wrote the manuscript. Yunzhi.W. conducted data interpretation, contributed to the analysis, and manuscript editing. J.Zhu. conducted fomal analysis in Fig. 5. Z.F. conducted formal analysis in Fig. 6. J.Zha. conducted analysis in Figs. 4 and 7. F.H., Z.Y., Y.C., B.Y., Z.Q., W.R., R.Hu. Yo.W., N.Q., J.F., Y.Z., and W.R. provided expertise. Q.Z., Z.X., R.H., Yu.W., Z.F. and J.Zhu. contributed to revision. C.D. conceived experiments, wrote the manuscript, provided expertise and secured funding. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Rafael Contreras-Galindo, Ashok Kumar Jayavelu, Souren Paul, Georgios Zenonos and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Q., Xu, Z., Han, R. et al. Proteogenomic characterization of skull-base chordoma. Nat Commun 15, 8338 (2024). https://doi.org/10.1038/s41467-024-52285-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-024-52285-7
This article is cited by
-
TP53 mutations as drivers of chordoma progression and hallmarks of aggressive chordoma
Acta Neuropathologica Communications (2025)