Abstract
Here we report results of a phase 1 multi-institutional, open-label, dose-escalation trial (NCT02744287) of BPX-601, an investigational autologous PSCA-directed GoCAR-T® cell product containing an inducible MyD88/CD40 ON-switch responsive to the activating dimerizer rimiducid, in patients with metastatic pancreatic (mPDAC) or castration-resistant prostate cancer (mCRPC). Primary objectives were to evaluate safety and tolerability and determine the recommended phase 2 dose/schedule (RP2D). Secondary objectives included the assessment of efficacy and characterization of the pharmacokinetics of rimiducid. Thirty-three patients received BPX-601 with or without rimiducid, 24 patients with mPDAC and 9 with mCRPC. Two dose-limiting toxicities and two treatment-related deaths occurred in the highest-dose mCRPC cohort, after which the study was terminated, without determination of the RP2D. Two mCRPC patients experienced partial responses (one unconfirmed), and 56% of mCRPC patients achieved ≥50% reduction in prostate-specific antigen. BPX-601 cell expansion, long-term persistence in peripheral blood, and tumor infiltration were observed. Rimiducid increased circulating inflammatory cytokines/chemokines consistent with GoCAR-T® cell activation. These results suggest that pharmacological activation of GoCAR-T® cells is feasible and may offer a promising avenue to control chimeric antigen receptor-T cell activity with continued dose-optimization to improve tolerability.
Similar content being viewed by others
Introduction
Chimeric antigen receptors (CARs) are synthetic receptors that redirect the specificity and improve the efficacy of T cells. In recent years, the adoptive transfer of CAR T cells has become a well-established treatment for certain hematologic malignancies, with remarkable response rates, leading to six clinical approvals of CAR T cells targeting CD19 or BCMA1. The most well-described toxicities associated with cellular therapies are cytokine release syndrome (CRS) and neurotoxicity (immune effector cell-associated neurotoxicity syndrome [ICANS]). In addition, toxicities resembling hemophagocytic lymphohistiocytosis (carHLH), characterized by fever, hyperferritinemia, coagulopathy, hepatic dysfunction, and cytopenias have been described as a secondary inflammatory wave after initial improvement in CRS symptoms and are frequently life-threatening2.
However, the success of CAR T cell therapies against solid tumors remains elusive, likely due to limited CAR T cell fitness, expansion, and persistence; susceptibility to T cell exhaustion; poor trafficking and infiltration into tumors; and/or the immunosuppressive tumor microenvironment3. Further, the selection of target antigens with heterogeneous tumor expression and off-tumor expression can lead to incomplete response and on-target off-tumor toxicity. Finally, severe adverse events (AEs) linked to over-activation of the therapeutic cells and/or host immune system also limit efficacy in patients4.
To address some of the limitations of constitutively activated CAR T cell approaches in solid tumors, we developed a novel approach to drive antitumor activity through the pharmacological activation of CAR T cells. BPX-601 is an investigational genetically modified, autologous GoCAR-T® cell product that targets prostate stem cell antigen (PSCA)-expressing cells through a first-generation anti-PSCA CAR with which cytotoxicity (T cell signal 1) is directed by CD3ζ. BPX-601 co-expresses an engineered cytoplasmic molecular ON-switch, the inducible MyD88/CD40 (iMC) construct, that is activated by dimerization induced by the clinically validated, specific, and otherwise biologically inactive small molecule rimiducid (formerly AP1903) (Supplementary Fig. 1A)5,6. This activation switch places the T cell co-stimulatory signal (T cell signal 2) under the tunable control of the pharmacologic agent rimiducid. In the presence of rimiducid, iMC dimerization activates Toll-like receptors and CD40 signaling pathways and triggers strong pro-survival, activation, and expansion signals in the GoCAR-T® cells (Supplementary Fig. 1B). iMC activation alone is not sufficient to drive expansion of transduced primary human T cells without synergy with an activated CAR or T cell receptor bound to its target7,8,9. Thus, iMC represents a potent genetic tool to pharmacologically control CAR T cell activation and modulate therapeutic activity.
PSCA is a small glycosylphosphatidylinositol-anchored cell surface protein belonging to the Thy-1/Ly-6 family. PSCA is overexpressed in ~50% of metastatic pancreatic ductal adenocarcinomas (mPDAC) and 80% of prostate cancers10, including nearly 100% of bone lesions from metastatic castration-resistant prostate cancer (mCRPC), with limited normal expression in the epithelial cells of the bladder, kidneys, skin, esophagus, stomach, and placenta11,12,13,14,15, making PSCA an attractive immunotherapeutic target16,17,18,19. Furthermore, PSCA expression in prostate cancer is positively correlated with tumor stage, grade, and independence from androgen signaling20.
Here we show the results from a multi-center, open-label, single-arm phase 1 dose-escalation clinical trial of PSCA-directed, genetically modified, autologous BPX-601 GoCAR-T® cells with pharmacological activation by rimiducid in patients with mPDAC or mCRPC. The safety and efficacy of BPX-601 plus rimiducid in patients with advanced solid tumors is reported in detail. We demonstrate the expansion and persistence of BPX-601 cells in peripheral blood (PB), their activation by rimiducid, and their infiltration in tumors. Collectively, these data show that pharmacological activation of GoCAR-T® cells with rimiducid is feasible and with continued dose optimization to improve tolerability may offer an avenue to control CAR T activity. Conclusions regarding efficacy and correlative outcomes are limited by small patient numbers in each cohort and the early-stage nature of this trial and should be viewed as hypothesis generating.
Results
Clinical trial design and patient characteristics
Our phase 1 study (NCT02744287) evaluated the safety and efficacy of BPX-601, a PSCA-directed, autologous GoCAR-T® cell product, administered with and without rimiducid in a 3 + 3 dose-escalation design (Supplementary Fig. 2A). Patients with mPDAC were screened to confirm PSCA mRNA expression prior to enrollment. Patients with mCRPC were enrolled without selection for PSCA given the high prevalence of expression in this disease; PSCA mRNA expression was retrospectively confirmed in the evaluable pre-treatment biopsies obtained from four of the nine mCRPC patients. PSCA protein expression could not be quantified by the time of study closure, limiting the interpretation of antigen expression/response relationship.
In the dose-escalation phase of the clinical trial, lymphodepletion (LD) regimens consisting of cyclophosphamide (Cy) (mPDAC cohorts 0, 3, 4, and 5A, n = 13) or Cy/fludarabine (Cy/Flu) (cohorts 5B and 5C: PDAC, n = 11 and mCRPC, n = 9), BPX-601 cell dose (1.25 × 106–5 × 106 cells/kg in mPDAC patients, 5 × 106 cells/kg in mCRPC patients) and rimiducid administration schedule (none, once at day 7, or weekly starting at day 7) at 0.4 mg/kg, were evaluated (Supplementary Fig. 2A). Twenty-four mPDAC and 9 mCRPC patients received BPX-601 (Supplementary Fig. 2B) and composed the population evaluable for safety (n = 33); among them 29 patients (88%) received rimiducid in some capacity, 19 patients as a single dose and 10 patients as weekly doses (number of doses ranged from 2 to 48).
Patients’ clinical and disease characteristics are presented in Supplementary Table 1. The median age at study entry was similar for the two tumor types. The median number of prior treatment regimens was 2 for patients with mPDAC (range 1–6) and 8 for patients with mCRPC (range, 5–9). All patients with mCRPC had received prior androgen receptor signaling inhibitor therapy and taxane-based chemotherapy; all patients with soft tissue disease had received prior immunotherapy.
Safety and tolerability of BPX-601 CAR T cells with rimiducid
At least one treatment-emergent adverse event (TEAE) was reported in all patients irrespective of relationship to investigational therapy (Supplementary Tables 2 and 3). The most frequent grade ≥3 TEAEs (≥20%) were neutropenia (45.8% and 55.6%), leukopenia (37.5% and 44.4%), and anemia (20.8% and 77.8%) for the mPDAC and mCRPC cohorts, respectively. These myelosuppressive AEs are commonly observed with the chemotherapy administered for LD, and many of these events were attributed to LD by the investigators.
CAR T cell therapy commonly results in two primary toxicities: CRS and neurologic toxicity/ICANS. CRS of any grade occurred in 12.5% of mPDAC and 100% of mCRPC patients (Supplementary Table 3 and Supplementary Fig. 3). Grade ≥3 ICANS was reported in 1/24 (4.2%) mPDAC and 2/9 (22.2%) mCRPC patients. CRS and neurotoxicity events were observed only in patients who received the highest tested dose of BPX-601 (5 × 106 cells/kg) following Cy/Flu LD. In the mPDAC cohorts, CRS was not reported following BPX-601 alone, in contrast to 44.4% (4/9) of mCRPC patients, who experienced manageable grades 1 or 2 CRS that typically began 1–3 days after cell infusion. All patients with mCRPC experienced CRS after the first dose of rimiducid (grades 1–3), with onset of fever beginning the day after rimiducid administration (median time to onset 1 day [range: 1–3 days]). Grade ≥3 CRS or ICANS events were reported only following the first or second dose of rimiducid; none occurred after the third or later rimiducid administration. Rimiducid was delayed in one patient with mCRPC and discontinued in four patients with mPDAC for related AE. Routine supportive care for the management of CRS and/or ICANS included corticosteroids (four mPDAC and four mCRPC patients), tocilizumab (three mPDAC and five mCRPC patients, half of whom received more than one dose), and siltuximab (one mPDAC and two mCRPC patients).
Four patients (two patients each in the mPDAC and the mCRPC cohorts) experienced dose-limiting toxicities (DLT, criteria provided in the “Methods” section) (two grade 4 CRS, one grade ≥3 ICANs [lasting >7 days] and one fatal sepsis) at the BPX-601 5 × 106 cell/kg dose level (Supplementary Tables 3 and 4). Following the second DLT event in the mCRPC cohorts, the trial was discontinued. The maximum tolerated dose was 5 × 106 cells/kg with a single dose of rimiducid, and the RP2D was not defined. The planned evaluation of lower BPX-601 cell dose (2.5 × 106 cells/kg) with weekly rimiducid, expected to better support CAR T expansion and persistence through weekly dosing, was not explored due to early study discontinuation.
Clinical antitumor efficacy
Antitumor response, evaluable in 26 patients, is reported in Table 1. No objective radiographic responses were observed in mPDAC patients; modest tumor shrinkage was reported in three patients. There were two partial responses in mCRPC patients (Fig. 1A, C), one of which was unconfirmed due to patient death.
a Waterfall plot depicting maximum fold change in tumor target lesion (per RECIST 1.1) (open bars) and PSA (closed bars) for individual mCRPC patients (n = 9) treated in cohort 5B (orange) and 5C (purple). * indicates patients who received steroids during treatment. Horizontal dash lines indicate 30% decrease in tumor size (−30%) and PSA decrease of 50% (PSA50) and 90% (PSA90). b Spider plot showing the kinetics of PSA response per patient within the 1st month after BPX-601 cell infusion. c Computed tomography scans demonstrating tumor reduction in patient mCRPC-5B-3 following administration of BPX-601 cells and a single rimiducid infusion. Radiologic images were obtained before therapy and at day 42 after BPX-601 cells. The tumor site is indicated by the orange arrow. Source data are provided as a Source Data file.
Antitumor responses in the mCRPC cohorts were also evaluated by measuring maximum declines from baseline in serum prostate-specific antigen (PSA) (Fig. 1A, B). A decrease in PSA of at least 50% (PSA50 response) was observed in five (55.6%) patients. Four of these patients experienced a decrease in PSA levels of at least 90% (PSA90 response). Biochemical responses were rapid, with the maximum decrease in PSA often observed on or before the first protocol-defined timepoint of day 28 (Fig. 1B).
Two patients with mCRPC with bone-only disease were evaluated for response by Prostate Cancer Working Group 3 (PCWG3) criteria, with one demonstrating clinical progression with rising PSA, confirmed at week 16 and the second experiencing stable-to-improving radiographic disease for ~6 months following a PSA90 response (Fig. 1A).
BPX-601 cell expansion and persistence
BPX-601 cells expanded in the PB of all patients, with an initial expansion phase peaking within 14 days after BPX-601 cell infusion, followed by a variable decline (Fig. 2 and Supplementary Fig. 4). The magnitude of BPX-601 peak expansion in mPDAC patients generally increased with cell dose and use of Cy/Flu LD compared to Cy alone (Supplementary Fig. 5A, B). Greater cell expansion after Cy/Flu was most likely due to increased levels of the lymphocyte-stimulating cytokine IL-15 (Supplementary Fig. 5C), as expected21. Maximal BPX-601 cell expansion after Cy/Flu was similar for mPDAC and mCRPC patients who received 5 × 106 cells/kg and either single or weekly doses of rimiducid (Fig. 2A, B and Supplementary Figs. 4, 5A, B).
CAR T cell expansion and persistence in peripheral blood of a mPDAC (n = 11) and b mCRPC (n = 9) patients enrolled in cohorts 5B (orange) and 5C (purple) measured by qPCR-based detection vector copy number (VCN) in genomic DNA. BPX-601 pharmacokinetics over the 1st month for all subjects and beyond that time for evaluable patients are shown. LLOQ lower limit of quantitation. Effect of rimiducid on CAR T cell and cytokine production in patients with c mPDAC (n = 11) or d mCRPC (n = 9, except n = 8 for rimiducid PK) enrolled in cohorts 5B and 5C after first rimiducid dose. Rimiducid PK (black), VCN (red), and IFN-γ concentration (orange) in peripheral blood (mean ± SD) are shown to illustrate the effect of rimiducid dosing on VCN and IFN-γ production (as an example of multiple cytokines’/chemokines’ response to rimiducid infusion). Main figure shows data during the first 14 days of treatment, and inserts highlight data during the day after rimiducid dosing, with timeline (days) adjusted to align BP-601 and rimiducid infusions across all patients. Cytokine and chemokine response during 1st month in patients with e mPDAC (n = 11) or f mCRPC (n = 9) enrolled in cohorts 5B and 5C. Median maximum fold change from pretreatment for each cytokine/chemokine is shown for the first 4 weeks of treatment, plotted as pre-dose and peak observed after each infusion (BPX-601 or rimiducid, as indicated). Baseline and peak cytokines of patients from cohorts 5B and 5C are shown for BPX-601 and first rimiducid dose, then only patients from cohort 5C are shown for rimiducid doses 2 and 3. Source data are provided as a Source Data file.
BPX-601 cells persisted in the PB of patients with mPDAC and mCRPC up to 250 days after infusion; some patients with detectable BPX-601 DNA at last measurement were lost to follow-up, and BPX-601 cells persistence in those patients was not established (Fig. 2A, B). BPX-601 cells kinetics were not statistically different in mCRPC patients with ≥PSA50 responses (Supplementary Fig. 5D).
Rimiducid pharmacokinetics and impact on BPX-601 cells and circulating inflammatory markers
Rimiducid was given to patients at a dose of 0.4 mg/kg infused over 2 h. Rimiducid’s pharmacokinetic parameters were evaluated in cohorts 5B and 5C and were generally consistent between cohorts, with plasma concentrations increasing rapidly during the 2-h infusion, then showing rapid distribution, declining to low or undetectable levels within 24 h after infusion (Supplementary Fig. 6), consistent with a prior report22.
Following rimiducid infusion, a rapid decrease in BPX-601 cell levels in PB was observed, followed by variable recovery over the following week (Fig. 2C, D). The timeline of decrease of BPX-601 cells in the PB after rimiducid infusion suggests that BPX-601 cells marginate out of circulation after iMC activation, rather than undergo potential activation-induced cell death, although the later hypothesis cannot be formally eliminated. The subsequent re-increase in BPX-601 may be explained as return of the cells in circulation or proliferation/expansion. Interestingly, while a rapid rebound of BPX-601 was observed within a few hours to 1 day in most mPDAC patients, rebound was generally slower and/or less profound in patients with mCRPC, potentially suggesting a more efficient engagement of BPX-601 cells with the tumor. An increase in pro-inflammatory cytokines and chemokines commonly associated with CAR T cell activation was observed after rimiducid infusion, most frequently peaking within the day following rimiducid infusion and returning to baseline within a week (Fig. 2C, D).
CAR T cell activation and inflammatory cytokines/chemokines
The release of inflammatory cytokines and chemokines commonly associated with CAR T cell activation (e.g., IFN-γ, TNF-α, GM-CSF, IL-6) after BPX-601 cell infusion alone was detectable but limited, consistent with reports of first-generation CAR T cells23. Rimiducid infusions led to higher elevations of the serum levels of these multiple cytokines and chemokines. Weekly dosing of rimiducid led to repeat cycles of increase and normalization of these cytokines and chemokines, consistent with CAR T cell activation (Fig. 2E, F and Supplementary Figs. 7, 8). Levels of inflammatory cytokines and chemokines generally normalized to pre-treatment levels between BPX-601 and rimiducid infusions or weekly rimiducid doses. Levels of circulating cytokines/chemokines induced by rimiducid were much higher in patients with mCRPC than in patients with mPDAC (for example, the median fold induction of IFN-γ was eightfold [range 1–157-fold] in mPDAC patients versus 102-fold [range 5–1816-fold] in mCRPC patients after the first dose of rimiducid) (Fig. 2E, F), potentially suggesting greater tumor engagement and consistent with increased activity in mCRPC. In general, the first few rimiducid doses led to the strongest and most consistent induction of cytokine/chemokine release in PB; later doses were characterized by more limited or undetected IFN-γ increases, while other markers such as TNF-α, GM-CSF, IL-6, or MCP-1 continued to transiently increase with rimiducid dosing.
Exploratory analyses of peripheral biomarkers associated with toxicities and clinical activity in mCRPC
Owing to the greater clinical responses and immune activity observed in mCRPC, translational correlative analyses were focused on this indication. Grade ≥2 CRS or ICANS events occurred in three mCRPC patients after BPX-601 and/or the first two rimiducid infusions, which resulted in higher circulating levels of cytokines/chemokines associated with immune activation (IFN-γ, IL-6, IL-2, IL-8, IL-10, GM-CSF) than was observed in patients with no or grade 1 toxicity (Fig. 3A, B and Supplementary Figs. 7, 8). In two of these patients, CRS evolved to carHLH, with high ferritin levels (≥10,000 ng/mL) without CRP elevation and strong and sustained elevations in cytokines/chemokines canonically elevated in carHLH cases (IFN-γ, TNF-α, IL-6, IL-8, IP-10 [CXCL10], MCP-1, MIP-1β, soluble IL-2R [sCD25])2,24,25. A rapid increase in BPX-601 cells in the PB was observed in one of these patients (~300-fold in 6 days); the clonality of the expanded cells was not evaluable. Both patients had PSA90 responses at the time of carHLH symptoms (Supplementary Fig. 9).
a Heatmap grouped by individual patient depicting maximum grade of cytokine release syndrome (CRS) or immune effector cell-associated neurotoxicity syndrome (ICANS), peak inflammation marker/cytokine/chemokine levels, and biochemical response (PSA) per infusion during the 1st month in mCRPC patients (n = 9). b Box plots presenting peak inflammation marker/cytokine/chemokine levels grouped per pretreatment and maximum immune-related adverse event grade (n = 9 patients, n = 21 measurements Gr0-1, n = 6 measurements Gr2-4). c Box plots presenting maximum inflammation marker/cytokine/chemokine levels grouped per biochemical response in patients with mCRPC (n = 4 patients <PSA50, n = 5 patients >PSA50). Box plots show minimum, lower quartile, median, upper quartile, and maximum. Source data are provided as a Source Data file.
Higher peak circulating cytokine/chemokine levels were associated with higher grades of immune-related AEs and PSA response (Fig. 3). In contrast, while elevated CRP and ferritin levels were associated with higher grades of immune-related AEs only, they were not with tumor response (Fig. 3B, C).
All three mCRPC patients who experienced grade ≥3 CRS and/or carHLH after rimiducid infusion had grades 1–2 CRS 1–3 days following BPX-601 infusion. These low-grade CRS symptoms after cell infusion were concomitant with elevations in inflammation markers, including CRP, IFN-γ, TNF-α, GM-CSF, IL-6, IL-8, IL-10, and IP-10 (CXCL10), that were much greater than in patients without high-grade immune-related AEs after rimiducid (Fig. 4A). While symptoms resolved, circulating levels of some markers, such as IL-6, remained elevated at the time of rimiducid administration (Fig. 4B). Elevation of these markers was consistent with strong BPX-601 cell activation and suggestive of cell engagement in these patients after BPX-601 cell infusion and prior to the first dose of rimiducid, and may be used as biomarkers predictive of potential safety risk post rimiducid infusion.
a Radar graph showing peak cytokine/chemokine response after BPX-601 cell infusion grouped per maximal CRS or ICANS grade after rimiducid. Increases in circulating levels of a constellation of inflammatory markers after BPX-601 infusion were significantly higher in patients who later experienced grades 3–4 CRS or ICANS after the first or second rimiducid infusion, compared to patients who experienced no or grade 1 CRS or ICANS after rimiducid infusion. Radar graph shows minimum, mean, and maximum level for each marker in the patient group. b Levels of IL-6 after BPX-601 administration were significantly elevated in the three patients with mCRPC who experienced grade ≥3 CRS or ICANS after the first or second dose of rimiducid (shown in red) compared to patients who experienced a maximum of grade 1 CRS or ICANS (shown in black). * indicates the two patients with carHLH who died during the study. Timeline (days) has been adjusted to align BP-601 and rimiducid infusions across all patients. Rim rimiducid. Source data are provided as a Source Data file.
CAR T trafficking to tumor
Tumor infiltration of non-transduced T cells and BPX-601 cells was assessed in pre- and post-treatment tumor biopsies from six patients (three mPDAC and three mCRPC). CD3+ T cells were detected in all samples, and BPX-601 cells were detectable in all three mPDAC and two of three mCRPC biopsies. In one mCRPC patient, sequential tumor biopsies were obtained on day 24 after cell infusion and at the end-of treatment (day 147). Infiltration of BPX-601 cells was observed at day 24, accompanied by intense T cell infiltration in the tumor nests and surrounding stroma. In the end-of-treatment biopsy of the same lesion, very rare BPX-601 cells were detected, and the overall T cell infiltration was comparatively reduced and excluded from tumor nests (Fig. 5C).
Discussion
BPX-601 CAR T cells were designed as first-generation CAR T cells with pharmacologically controlled activation by rimiducid. While standard first-generation CAR T cells showed poor expansion, persistence, and cytokine induction in patients23, the pharmacodynamic characteristics of BPX-601 cells observed in this study, such as expansion, persistence up to 250 days in PB, induction of cytokines and chemokines associated with IFN-γ-driven antitumor activity, and infiltration into tumors, were comparable or superior to those of other programs that used constitutively activated and/or armored CAR T cells in solid tumors25,26,27. These favorable characteristics of BPX-601 cells can likely be attributed to the pro-survival, proliferation, and activation signals delivered from rimiducid-induced iMC signaling5,6,7,8.
This study was initiated in mPDAC patients, with the evaluation of LD regimens, cell dose-escalation, and rimiducid activity. Given the manageable toxicity observed, the trial was extended to mCRPC patients. Despite similar cell expansion, a much higher induction of inflammatory cytokines and more limited rebounds in BPX-601 cell counts after rimiducid was observed in mCRPC compared to mPDAC, suggesting that BPX-601 margination/extravasation and tumor infiltration and engagement were more efficient in mCRPC, a hypothesis also supported by the higher antitumor activity observed in this population. This is perhaps due to differences in CAR T cell access and trafficking and homing to tumor, which are determinants of response in other malignancies28. Unfortunately, the low number of evaluable tumor samples collected and the absence of PSCA protein measurement prevent the evaluation of the relationship between target antigen expression and pharmacodynamic and clinical response to BPX-601 with and without rimiducid.
Antitumor activity of BPX-601 with rimiducid in heavily pretreated mCRPC patients was encouraging, with five of nine (55.6%) patients experiencing PSA50 decreases—including four with PSA90 responses, two partial responses (one confirmed) in six efficacy-evaluable patients (33.3%), one patient with stable nodal disease for more than 1 year, and one PSA90 response with stable-to-improving bone scans for 6 months in one of two patients with bone-only disease. These efficacy results compare positively to other CAR T cell programs in prostate cancer targeting prostate-specific membrane antigen (PSMA) or PSCA, whose results included: 2 of 5 (40%) patients with PR and PSA50 reductions29, 2 of 7 (28.6%) patients with stable disease for >6 months30, 4 of 13 (30.8%) patients with PSA reduction ≥30% with no objective responses25, and 4 of 14 (28.6%) patients with PSA decrease including one PSA50 decline and no objective response19. While both PSMA and PSCA are associated with mCRPC, the overlap of co-expression remains unknown and PSCA might represent an additional target for patients who received prior PSMA targeted therapy.
Toxicities specific to PSCA-directed therapies are still under evaluation. In another study of PSCA-directed CAR T cells in mCRPC, two patients experienced severe cystitis, which may be due to PSCA expression in bladder tissue, although a role of cyclophosphamide LD was also explored. The cyclophosphamide dose was reduced from 500 to 300 mg/m2, after which no grade >2 AEs of cystitis were reported in five patients19. In our study, one case of grade 3 hematuria and no severe cystitis (grade ≥ 3) was reported, despite the use of cyclophosphamide at a dose of 500 mg/m2. One patient experienced grade 3 cholecystitis, which may represent on-target activity of BPX-601; tissue was not available for evaluation of PSCA expression or presence of tumor. Given the small sample size and unknown target antigen expression in this study, continued evaluation of gastrointestinal toxicities is warranted. Finally, respiratory toxicities and failures were observed in the setting of immune-mediated AEs. Since PSCA is not reported to be expressed on normal lung tissue (www.proteinatlas.org) and no grade ≥3 respiratory AEs were reported in the study of PSCA-directed antibody or other PSCA-directed CAR T cell therapies, the respiratory toxicities observed in this study are unlikely related to on-target effects, and rather common CAR T cell-related AEs16,17,19. Therefore, PSCA remains a promising therapeutic target due to its differential expression in tumor versus normal tissues, and association with tumor progression and aggressiveness15,20.
Evaluation of predictors of CAR T toxicity is an active area of research. Studies in hematologic malignancies have reported an association between the severity of CRS and higher tumor burden31,32; however, high tumor burden did not appear to be associated with toxicity in our study. Additional risks factors for severe AEs include cell dose, LD regimen, and target antigen levels2,24,25. In our study, high-grade immune-related AEs occurred in patients who received the highest tested dose of BPX-601 cells (5 × 106 cells/kg) following Cy/Flu LD and had higher expression of inflammatory cytokines; as stated above, target antigen measurement could not be completed by the time of study termination.
A delicate balance of benefit-risk exists between efficacy and toxicities of cellular therapies, especially in a primarily elderly patient population with comorbidities, as age is a known risk factor for immune-mediated toxicity33,34. While chemotherapy preconditioning has dramatically improved the efficacy of cellular therapies, it is not without toxicity, and which LD regimen is the most effective and safe remains under intense evaluation in clinical studies21,35. In this study, the addition of Flu to the cyclophosphamide-based LD regimen increased IL-15 serum levels and cell proliferation as previously reported21,36,37, and may have contributed to the observed efficacy; it also resulted in myelosuppression potentially increasing the risk of opportunistic infection. Since three deaths due to sepsis occurred in the highest cell dose cohorts following Cy/Flu LD, one must consider the relationship of LD to toxicity and evaluate potential mitigation strategies. While granulocyte colony-stimulating factor (G-CSF) may be used to mitigate LD-induced neutropenia, there is no consensus on the recommended strategy for the use of growth factors following CAR T administration or in the setting of CRS38 (www.nccn.org/professionals/physician_gls/pdf/growthfactors.pdf). Use in this context has been limited due to hypothesized but largely unknown risks of exacerbating CAR T-related toxicities39,40. In this protocol, routine use of G-CSF was not mandated; however, it could be implemented at the physician’s discretion.
While immune activation remained limited after infusion of BPX-601 cells, and no severe AEs were observed, the first one to two infusions of rimiducid led to significant increases in circulating inflammatory cytokines and chemokines and occurrence of higher grade immune-related AEs in a subset of patients. Patients with mCRPC who experienced grade ≥2 CRS after BPX-601/rimiducid also showed deep and rapid biochemical responses and tumor shrinkage. In these patients, we retrospectively observed markedly higher induction of inflammation markers after BPX-601 cell infusion, and that rimiducid was infused when circulating levels of some inflammatory cytokines were high, indicating that ongoing strong immune activation and inflammation was still occurring, which likely contributed to the occurrence of immune-related AEs in these patients. Monitoring levels of inflammation markers such as IL-6 and CRP during the week following BPX-601 infusion and prior to rimiducid dosing may identify patients at risk for immune-related toxicity. Delay of rimiducid infusion, and therefore BPX-601 re-activation, until after the prior wave of CAR T cells activation has receded and inflammatory markers have normalized, may limit or abrogate the occurrence of high-grade immune-related AEs, without significantly impacting antitumor activity.
While it is acknowledged that there were severe treatment-related events in this study, given the observed efficacy, lack of dose-limiting on-target off-tumor toxicity, and paucity of treatment options for patients with mCRPC, additional evaluation of BPX-601 with rimiducid to explore strategies to improve the therapeutic window is warranted. Potential approaches to optimize benefits versus risk may include modifying the LD regimen, cell dose, or dosing interval between rimiducid administrations; monitoring inflammatory markers prior to first few infusions of rimiducid and delaying rimiducid in patient with ongoing immune activation; and exclusion of patients with elevated baseline inflammatory markers (e.g., CRP, ferritin). Continued careful evaluation of patient selection with focus on comorbidities and consideration of pre-emptive toxicity management is an important area of research for administration of CAR Ts for the treatment of hematologic malignancies41, and our understanding of how to manage these complexities in patients with solid tumors continues to evolve. Pharmaceutical activation of CAR T cells may become an avenue to gain additional activity and control over CAR T cell activity, in addition to other strategies currently explored such as targeting multiple tumor antigens or armoring CAR T cells.
In conclusion, in this phase 1 trial, we demonstrated pharmacologic activation of PSCA-targeted BPX-601 GoCAR-T cells through rimiducid-induced activation of iMC signaling, providing the co-stimulatory signals needed to drive T cell activation and enhance antitumor activity, potentially overcoming some barriers to efficacy for CAR T cells in solid tumors such as reduced activation and CAR T cell exhaustion in the inhibitory tumor microenvironment. While limited pharmacodynamics, clinical activity, and toxicity were observed in mPDAC patients, BPX-601 with rimiducid led to encouraging pharmacodynamic and clinical activity in mCRPC, although complicated by the occurrence of serious immune-related events. Our findings lay the foundation for future development of iMC-enabled CAR T cell therapy, including optimization of the therapeutic window by incorporating enhanced toxicity mitigation strategies and expansion on observed efficacy in mCRPC through evaluation of predictors of response and/or mechanisms of resistance.
Methods
Study overview
This study evaluated the safety, clinical activity, and translational activity of BPX-601 with rimiducid in patients with metastatic pancreatic and prostate cancers.
This multi-center, phase 1 dose-escalation trial (NCT02744287) was conducted in accordance with the United States Food and Drug Administration, International Conference on Harmonization Guidelines for Good Clinical Practice, Declaration of Helsinki, and applicable institutional review board requirements. The study was open at 13 sites in the USA; the list is available in Supplementary Table 5. All patients provided written informed consent in accordance with local regulatory review. Between November 29, 2016 and November 29, 2022, patients were enrolled on the IRB-approved protocol (see Supplementary Information for full protocol). The protocol underwent four key amendments to optimize treatment strategies. A protocol amendment (June 27, 2018) limited the number of prior lines of therapy for patients with mPDAC. An amendment on May 1, 2019 added repeat-dose rimiducid infusion schedule. An amendment on July 15, 2020 enabled enrollment of patients with metastatic prostate cancer and another on November 9, 2021 adjusted the dose and duration of rimiducid infusion (no patients were treated on this revised dosing schedule due to early termination). These amendments aimed to refine the protocol and to maximize potential patient outcomes based on evolving clinical insights.
The trial was discontinued early on March 14, 2023 following a second DLT event in the ongoing cohort impacting access to continued financing to support further dose optimization. Final data extraction was taken June 1, 2023.
Screening
Patients with mPDAC were screened to confirm PSCA mRNA expression prior to enrollment. PSCA prevalence in this population is ~ 50%, resulting in a high number of patients screened. Notably, 38% of mPDAC patients screened did not have sufficient PSCA mRNA expression for enrollment or expression could not be determined from the tissue provided. Patients with mCRPC were enrolled without selection for PSCA given the high prevalence of expression in this disease (~80%); PSCA mRNA expression was retrospectively confirmed in pre-treatment biopsies from a subset of mCRPC patients with evaluable tumor (four of nine). Additional details on the reasons for patient screen failure are presented in Supplementary Fig. 2.
Patient eligibility
Patients eligible for inclusion in this study had to meet all the following criteria:
Eligible patients included those with mPDAC or histologically confirmed mCRPC with evidence of progressive disease according to PCWG2 criteria. Additional enrollment criteria included: (i) metastatic mPDAC with disease progression within 6 months of the most recent anticancer treatment, documented positive tumor expression of PSCA, and measurable disease (≥1 target lesion) per RECIST v1.142 at baseline; (ii) evidence of progressive castrate-resistant prostate adenocarcinoma (as defined by castrate levels of testosterone ≤ 50 ng/mL) with or without the use of androgen deprivation therapy and evidence of one of the following measures of progressive disease in the 12 weeks preceding study enrollment: measurable disease by RECIST 1.1 criteria at baseline or bone-only metastasis with measurable PSA (≥1 ng/mL) at baseline (per PCWG3 criteria43), increase in serum PSA of at least 25% and an absolute increase of 2 ng/mL or more from nadir (per PCWG3 criteria); (iii) previous therapy with at least one standard 17α-hydroxylase inhibitor or second-generation anti-androgen therapy for the treatment of mCRPC; (iv) age ≥18 years; (v) Eastern Cooperative Oncology Group performance status of 0–1; (vi) adequate organ function, as defined by serum creatinine ≤1.5 mg/dL or creatinine clearance >50 mL/min; (vii) serum total bilirubin ≤1.5× upper limit of normal and serum aspartate transaminase/alanine transaminase <2.5× upper limit of normal; (viii) adequate hematologic reserve within 4 weeks of study enrollment, as defined by hemoglobin ≥ 9 g/dL, platelet (thrombocyte) count ≥100 k/μL, absolute neutrophil count ≥1.0 k/μL, and subjects must not be transfusion dependent; (ix) provision of written informed consent; (x) subjects of reproductive potential had to agree to use acceptable birth control methods.
Exclusion criteria included: (i) malignant disease other than that being treated in this study; (ii) subjects who require the chronic use of systemic corticosteroid therapy; (iii) subjects with impaired cardiac function or clinically significant cardiac disease; (iv) subjects who have undergone a major surgical procedure, other than for diagnosis, within 4 weeks prior to enrollment; (v) subjects with symptomatic, untreated, or actively progressing central nervous system metastases; (vi) subjects with history or presence of clinically relevant central nervous system pathology; (vii) history of active or severe autoimmune disease requiring immunosuppressive therapy; (viii) patients with ongoing or active infection; (ix) patients with known bovine product allergy; (x) patients with active hepatitis B, hepatitis C, or human immunodeficiency virus infection; and (xi) receipt of prior CAR T or other genetically modified T cell therapy.
Study design and dose escalation
Dose escalation was initiated in mPDAC patients. Patients received a single infusion of BPX-601 GoCAR-T® cells, per the 3 + 3 dose-escalation design, with the following dose levels. In the lead-in cohort 0, three patients received a single dose of BPX-601 (1.25 × 106 cells/kg) on day 0 following the Cy LD regimen (three daily doses of cyclophosphamide 500 mg/m2 on days −5 to −3) and did not receive rimiducid. Based on the favorable safety profile and early clearance of BPX-601 T cells demonstrated in cohort 0, a single dose of rimiducid (0.4 mg/kg) on day 7 after BPX-601 cell infusion was added to the investigational treatment regimen. Cohort 3 was the initial starting cohort for cell-dose escalation with BPX-601 (1.25 × 106 cells/kg) administered after Cy LD and followed with a single dose of rimiducid (0.4 mg/kg) on day 7. Cohort 4 received an increased BPX-601 T cell dose (2.5 × 106 cells/kg) administered after Cy LD and followed with a single dose of rimiducid (0.4 mg/kg) on day 7. Cohort 5A received an increased BPX-601 T cell dose (5.0 × 106 cells/kg) administered after Cy LD and followed with a single dose of rimiducid (0.4 mg/kg) on day 7. In cohort 5B, the LD regimen was changed to cyclophosphamide plus fludarabine (Cy/Flu, three daily doses of cyclophosphamide 500 mg/m2 followed by Flu 30 mg/m2 on days −5 to −3) to increase BPX-601 cells’ engraftment and persistence. Cohort 5B received 5.0 × 106 cells/kg BPX-601 T cells administered after Cy/Flu LD and followed with a single dose of rimiducid (0.4 mg/kg) on day 7. Cohort 5C received 5.0 × 106 cells/kg BPX-601 T cells administered after Cy/Flu LD and introduced weekly dosing of rimiducid (0.4 mg/kg) starting on day 7. Additional cohorts were planned to explore rimiducid at higher doses with a longer infusion time.
Enrollment of patients with mCRPC was initiated after patients with mPDAC completed the safety evaluation period in cohort 5B and initiated with the last safe dose determined safe in mPDAC, ie cohort 5B (5.0 × 106 cells/kg BPX-601 T cells administered after Cy/Flu LD, and followed with a single dose of rimiducid (0.4 mg/kg) on day 7). After three patients were evaluated for safety in mCRPC cohort 5B, cohort 5C enrollment was initiated, with 5.0 × 106 cells/kg BPX-601 T cells administered after Flu/Cy LD, and weekly dosing of rimiducid (0.4 mg/kg) started on day 7. The study was prematurely terminated after two DLT were observed in mCRPC Cohort 5C. For the purposes of cohort-specific safety analyses mPDAC and mCRPC were considered separately.
Objectives and endpoints
The primary objective of the phase 1 portion of the study was to determine the safety, tolerability, and MTD and/or recommended phase 2 dose and schedule of BPX-601 and rimiducid. The maximum tolerated dose was defined as the highest BPX-601 T cell dose level and/or rimiducid dose and infusion duration at which <33% of subjects experience a DLT during the DLT evaluation period. For this study, DLT were defined as any of the following unless clearly due to disease progression or extraneous causes: any treatment-emergent grades 4 or 5 CRS, any treatment-emergent grade 3 CRS that did not resolve to grade ≤2 within 7 days, any grade ≥ 3 infusion reaction that did not resolve within 7 days, any grade ≥ 3 organ toxicity (cardiac, dermatologic, gastrointestinal, hepatic, pulmonary, renal/genitourinary, neurologic or autoimmune) not pre-existing or due to the underlying malignancy that did not resolve to grade ≤2 within 7 days.
To assess the safety of BPX-601 and rimiducid in this study population, AEs were graded using CTCAE v4.1 and ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells44 and summarized descriptively. Objective tumor treatment responses for patients with soft tissue disease were scored by RECIST 1.1 criteria. Patients with mCRPC with bone-only disease were evaluated for response by PCWG3 criteria. Exploratory objectives included characterization of the pharmacodynamics of BPX-601 T-cells administered with and without rimiducid and exploration of the relationship between rimiducid PK and BPX-601 pharmacodynamic biomarkers. Due to the early termination of the program, the exploratory objective to characterize immunogenicity was not completed.
Specimen collection
Whole blood samples were collected at multiple protocol-mandated times before and after infusion of BPX-601 cells for pharmacokinetic and pharmacodynamic exploratory analyses.
Archival or fresh pre-treatment tumor biopsies were collected from mPDAC patients for PSCA expression testing prior to enrollment; post-treatment biopsies were collected for pharmacodynamic analyses. Archival and fresh pre- and post-treatment biopsies were collected from mCRPC patients for predictive and pharmacodynamic biomarkers analyses. Nine on-treatment biopsies (from patients in mPDAC cohort 5B [n = 3] and mCRPC cohorts 5B [n = 2] and 5C [n = 4]) were collected after BPX-601 cell infusion and at least one rimiducid infusion, as well as one end-of-treatment (mCRPC cohort 5B patient) biopsy. Biopsies collected from bone metastases of four mCRPC patients in cohort 5C did not contain tumor cells. Paired pre- and on-treatment biopsies from three mPDAC and three mCRPC patients were tested for pharmacodynamic exploratory analyses. PSCA protein expression was not determined at the time of study closure due to the lack of a reliable analytical method.
Quantitative PCR analyses of PSCA expression for enrollment in mPDAC cohort
Formalin-fixed paraffin-embedded (FFPE) archival tumor samples were collected for evaluation of PSCA mRNA expression for study eligibility; when not available, a fresh pre-treatment tumor biopsy was required. Samples were tested with qRT-PCR or at Molecular MD (Portland, OR) with ddPCR. Total RNA was extracted using RNeasy FFPE Kit, or RNEasy Mini Kit (Qiagen) using the Maxwell CSC instrument. qRT-PCR was performed for PSCA and hACTB as control using specific primers. 103 PSCA copies/106 hACTB copies was used as positivity threshold for determination and inclusion into the BP-012 clinical trial. ddPCR was performed using the QX200 ddPCR instrument (Bio-Rad) and the One-Step RT-ddPCR Advanced Kit for Probes (Bio-Rad), in duplicate wells with the reference gene IPO8, using 5 ng RNA/well. A minimum droplet count of 9000 ensured data integrity. The PSCA/IPO8 ratio of 0.024 was used as positivity threshold for determination and inclusion into the BP-012 clinical trial.
PSCA forward primer: CAAAGCCCAGGTGAGCAA; PSCA reverse primer: AGTCATCCACGCAGTTCAAG; PSCA probe: 56/FAM/CCTCCTGAC/ZEN/CGTCATCAGCAAAGG/3IABkFQ.
Manufacturing and characteristics of CAR T cell products
Following confirmation of enrollment, 52 patients underwent apheresis. Apheresis products were shipped to a cleanroom facility (Nebraska Medical Center’s Biologics Production Facility, Resilience Texas, or Bellicum’s in-house facility) where manufacturing was performed according to Phase 1 IND current Good Manufacturing Practice guidelines and FACT Common Standards for Cellular Therapies. Incoming apheresis products were processed using either CD4/CD8-positive selection to enrich for T lymphocytes followed by immediate cell culture, or Ficoll density-gradient enrichment of mononuclear cell content, followed by cryopreservation and subsequent thaw of aliquoted material to initiate cell culture. The cell culture was then activated using soluble anti-CD3 and anti-CD28 antibodies in the presence of IL-7 and IL-15. Based on the target final cell dose, a portion of the cultured cells was transduced on process day 4 with the CAR/iMC gamma retrovirus construct in adherent bags (St. Gobain) using RetroNectin as a transduction enhancer. Culture continued after transduction until the target dose of CAR-positive cells was met, with a target overall process length of 8 days and the possible extension to 11 days if the target dose was not met on day 8. Over 95% of batches initiated reached the target cell dose by day 8, and one or two final product doses were formulated and cryopreserved in each case. The total manufacturing cycle time generally ranged from 24 to 30 days without interruption. Manufacturing was initiated (defined as initiation of cell culture) for a total of 51 subjects; manufacturing of 1 of the 52 aphereses performed was not initiated as it occurred just prior to study termination. BPX-601 cells were successfully manufactured for 50 of 51 of these subjects (manufacturing success rate 98%). The one manufacturing failure (1/51 or 2%) was contaminated in the cell culture process before transduction with no additional aliquot of processed apheresis material available; a second apheresis was not performed due to program discontinuation. Thirty-three manufactured products were infused to patients in this study; other manufactured products were not infused due to duration and success of bridging therapy, disease progression, and/or termination of the program.
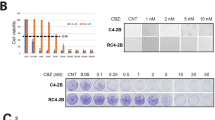
Cell product release assays
Release testing of BPX-601 cell product measured the quantity and activity of the BPX-601 GoCAR-T® cells and included cell count, viability, percent positive CAR T cells, cytotoxicity, and IL-2 production in co-cultures with PSCA-positive human pancreatic adenocarcinoma cell line (HPAC). PCR assays were performed to ensure the lack of replication-competent retrovirus, and to quantitate the vector copy number (VCN) of the integrated transgenes in the BPX-601 cell product. To ensure microbial safety, mycoplasma by PCR, endotoxin, and rapid sterility testing were performed.
Characteristics of cell products
In the infused mPDAC products, the mean frequency of CAR-expressing T cells in infusion products was 45.2% (range 25.0%–67.0%), with a mean VCN per transduced cell of 2.0 (range 1.2–2.6). Evaluation of cytotoxicity and IL-2 production of the BPX-601 cells in mixed-cell assays showed 91.6% mean cytotoxicity (range 84.7%–95.5%) and 5997 pg/mL IL-2 production (range 1642–13,372 pg/mL). In the infused mCRPC products, the mean frequency of CAR-expressing T cells in infusion products was 50.8% (range 30.0%–68.0%), with a mean VCN per transduced cell of 1.5 (range 0.9–2.6). Evaluation of cytotoxicity and IL-2 production of the BPX-601 cells in mixed-cell assays showed a mean cytotoxicity of 91.5% (range 80.9%–99.6%) and 6870 pg/mL (2850–12,200 pg/mL) IL-2 production.
Bridging therapy and toxicity management
For patients whose tumor burden was heavy or whose disease had the potential to rapidly progress, according to the investigators’ discretion, during the period of BPX-601 manufacturing, bridging chemotherapy was permitted. Investigators were allowed to individualize the regimen according to the patient’s previous antitumor therapy and the patient’s clinical condition.
Tocilizumab, corticosteroids, or other immunosuppressive measures were administered according to the investigator’s discretion for toxicity management.
Rimiducid pharmacokinetics
Whole blood samples for the determination of plasma levels of rimiducid (AP1903) were collected at pre-dose, 1, 2, 4, 8, and 24 h after the start of rimiducid infusion.
Rimiducid PK analyses were performed at KCAS Bioanalytical & Biomarker Services (Olathe, KS). Rimiducid and internal standard were released from the human plasma by protein precipitation using a 1:1 methanol/acetonitrile solution. Supernatant was chromatographed using reversed-phase HPLC with a Zorbax SB-C8 analytical column. Rimiducid and internal standard AP23510 were detected by monitoring the precursor and product ions using an Applied Biosystems Sciex API 6500 LC–MS/MS. The lower limit of quantitation was 1.00 ng/mL.
Sampling for rimiducid pharmacokinetics was required only in cohorts 5B and 5C; measurement of rimiducid concentration in plasma after the first rimiducid dose was performed using all available samples, obtained from 19 patients (11 patients with mPDAC and 8 with mCRPC).
Quantitative PCR analyses of BPX-601 expansion and persistence (VCN)
Whole blood samples were collected and stored as is at −70 °C, or peripheral blood mononuclear cells (PBMCs) were prepared using the Ficoll method and cryopreserved. VCN analyses were performed in Bellicum Laboratories (Houston, TX) or at LabCorp (Greenfield, IN). Genomic DNA (gDNA) was extracted from frozen whole blood or PBMCs using the QIAamp DNA Blood Kit or DNA Blood and Tissue Kit (Qiagen).
The standard curve for the transcript copy number was established by the amplification of a 9–10 point standard curve consisting of between 10 and 5 × 107 copies of pBP0189 plasmid. The number of transgene copies per microgram of gDNA was determined on a Step One Plus Real-Time PCR system (Applied Biosystems) or a Quant Studio Flex Real-Time PCR system (Thermo Fisher Scientific). BPX-601 forward primer: GGCATCACCACACTTGATGAC; BPX-601 reverse primer: GCCTTATTGGTTGGCTTCTTG; BPX-601 probe: 5′-6-FAM/ATATGCCTG/ZEN/AGCGTTTCGATGCCT/IABkFQ-3′. Each data point (sample, standard curve, positive and negative controls, quality controls) was evaluated in triplicate. The limit of detection of this assay was 10 copies/microgram of gDNA.
VCN was expressed per microgram of PBMC gDNA. To normalize the transcript copy number obtained from whole blood samples to the value from PBMC, VCN was measured from whole blood and PBMC obtained from 12 blood collections from three patients, and a correlation equation was derived with an R2 of 0.9117. Copies of transgene per μg gDNA in PBMCs were calculated according to the formula: Copies of transgene per μg gDNA in PBMC = (copies of transgene per μg gDNA in whole blood)/0.2824.
Serum cytokine profiling
Multiplex Luminex cytokines testing was performed in the Bellicum Lab and KCAS Bioanalytical & Biomarker Services (Olathe, KS). Whole blood samples were collected before and after BPX-601 or rimiducid infusions, serum was prepared and samples were cryopreserved at −70 °C until analysis. For cytokine/chemokine measurements, the serum samples were thawed and tested using 29-plex MILLIPLEX MAP Human Cytokines/Chemokines MAG panel (Millipore) following the manufacturer’s instructions. Data were collected with a Luminex 200 controlled by xPONENT version 4.2 or later and imported into MILLIPLEX Analyst version 5.1.1.0 or later for calculation of concentrations and statistical analyses. The calibration curves were regressed using 5 parameter logistic curve fit.
Detection of BPX-601 CAR T cells and PSCA mRNA expression in tissue by chromogenic in situ hybridization
RNAscope chromogenic in situ hybridization (CISH) and dual CISH/IHC assays were performed at Advanced Cell Diagnostics (ACD; Newark, CA). Five-micron FFPE sections were evaluated by RNAscope CISH for the expression of the following RNAs using ACD probes as follows: specific for BPX-601 retroviral GoCAR-T® cell vector construct (mPDAC: single probe: 549188, mCRPC: pooled probes: 564508 and 1141668-C1), PSCA (820628), positive control PPIB (313908), and negative control bacterial dapB (312038). CD3 was detected by IHC (anti-CD3 rabbit antibody [Roche 790-4341] per manufacturer recommendation (neat) or mouse antibody [LN-10, Leica CD3-565-L-CE]). The RNAscope CISH assays were performed using the RNAscope 2.5 LSx (ACD: 322750) Red Reagent Kit, and IHC was performed using Leica BOND Refine Detection Kit and RNAscope 2.5 LS Green Accessory Pack (Cat. No. 322550). Staining was performed on the Leica Biosystems BOND RX platform according to the automated RNAscope and dual RNAscope/IHC protocols optimized for use on the instrument. Stained slides were reviewed by a pathologist, and percent positive and signal intensity scores in the tumor were provided.
Statistical analysis
The sample size was based on clinical considerations and a modified 3 + 3 dose-escalation/de-escalation design. Descriptive statistics include the number of cases, mean, median, standard deviation, minimum and maximum values for continuous variables, and frequency distributions for categorical variables. All TEAEs were categorized according to the ICH MedDRA codes version 25.1, graded according to CTCAE version 4.1, and analyzed via frequency distributions, tables, or other descriptive indicators. The number and percentage of patients experiencing TEAEs were calculated based on system organ classification, preferred term, and different groups. Exact methods contain the Clopper–Pearson method with 95% CIs for ORR and DCR.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The study protocol is available in the Supplementary Information file. All data reported in Article, Supplementary Information, and Source data files are anonymized to respect the privacy of patients who participated in the study, consistent with applicable laws and regulations. Additional individual de-identified participant data and other datasets generated and/or analyzed during the current study beyond the data that was disclosed in the manuscript cannot be shared since they were collected as part of a clinical trial and subject to patient confidentiality as well as proprietary considerations. Source data are provided with this paper.
References
Chen, Y. J., Abila, B. & Mostafa Kamel, Y. CAR-T: what is next? Cancers 15, 663 (2023).
Hines, M. R. et al. Immune effector cell-associated hemophagocytic lymphohistiocytosis-like syndrome. Transplant. Cell. Ther. 29, 438.e431–438.e416 (2023).
Guzman, G., Reed, M. R., Bielamowicz, K., Koss, B. & Rodriguez, A. CAR-T therapies in solid tumors: opportunities and challenges. Curr. Oncol. Rep. 25, 479–489 (2023).
Sterner, R. C. & Sterner, R. M. CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J. 11, 69 (2021).
Narayanan, P. et al. A composite MyD88/CD40 switch synergistically activates mouse and human dendritic cells for enhanced antitumor efficacy. J. Clin. Investig. 121, 1524–1534 (2011).
Clackson, T. et al. Redesigning an FKBP-ligand interface to generate chemical dimerizers with novel specificity. Proc. Natl. Acad. Sci. USA 95, 10437–10442 (1998).
Foster, A. E. et al. Regulated expansion and survival of chimeric antigen receptor-modified T cells using small molecule-dependent inducible MyD88/CD40. Mol. Ther. 25, 2176–2188 (2017).
Mata, M. et al. Inducible activation of MyD88 and CD40 in CAR T cells results in controllable and potent antitumor activity in preclinical solid tumor models. Cancer Discov. 7, 1306–1319 (2017).
Duong, M. T. et al. Two-dimensional regulation of CAR-T cell therapy with orthogonal switches. Mol. Ther. Oncolytics 12, 124–137 (2019).
Reiter, R. E. et al. Prostate stem cell antigen: a cell surface marker overexpressed in prostate cancer. Proc. Natl. Acad. Sci. USA 95, 1735–1740 (1998).
Bahrenberg, G., Brauers, A., Joost, H. G. & Jakse, G. Reduced expression of PSCA, a member of the LY-6 family of cell surface antigens, in bladder, esophagus, and stomach tumors. Biochem. Biophys. Res. Commun. 275, 783–788 (2000).
de Nooij-van Dalen, A. G. et al. Characterization of the human Ly-6 antigens, the newly annotated member Ly-6K included, as molecular markers for head-and-neck squamous cell carcinoma. Int. J. Cancer 103, 768–774 (2003).
Ruan, Y., Yu, W., Cheng, F., Zhang, X. & Larré, S. Detection of prostate stem cell antigen expression in human prostate cancer using quantum-dot-based technology. Sensors 12, 5461–5470 (2012).
Zhigang, Z. & Wenlv, S. Prostate stem cell antigen (PSCA) expression in human prostate cancer tissues: implications for prostate carcinogenesis and progression of prostate cancer. Jpn. J. Clin. Oncol. 36, 121 (2006).
Saeki, N., Gu, J., Yoshida, T. & Wu, X. Prostate stem cell antigen: a Jekyll and Hyde molecule? Clin. Cancer Res. 16, 3533–3538 (2010).
Antonarakis, E. S. et al. Phase I rapid dose-escalation study of AGS-1C4D4, a human anti-PSCA (prostate stem cell antigen) monoclonal antibody, in patients with castration-resistant prostate cancer: a PCCTC trial. Cancer Chemother. Pharmacol. 69, 763–771 (2012).
Morris, M. J. et al. A phase I/IIA study of AGS-PSCA for castration-resistant prostate cancer. Ann. Oncol. 23, 2714–2719 (2012).
Abate-Daga, D. et al. A novel chimeric antigen receptor against prostate stem cell antigen mediates tumor destruction in a humanized mouse model of pancreatic cancer. Hum. Gene Ther. 25, 1003–1012 (2014).
Dorff, T. et al. PSCA-CAR T cell therapy in metastatic castration-resistant prostate cancer: a phase 1 trial. Nat. Med. 30, 1636–1644 (2024).
Gu, Z. et al. Prostate stem cell antigen (PSCA) expression increases with high Gleason score, advanced stage and bone metastasis in prostate cancer. Oncogene 19, 1288–1296 (2000).
Neelapu, S. S. CAR-T efficacy: is conditioning the key? Blood 133, 1799–1800 (2019).
Iuliucci, J. D. et al. Intravenous safety and pharmacokinetics of a novel dimerizer drug, AP1903, in healthy volunteers. J. Clin. Pharmacol. 41, 870–879 (2001).
Kershaw, M. H. et al. A phase I study on adoptive immunotherapy using gene-modified T cells for ovarian cancer. Clin. Cancer Res. 12, 6106–6115 (2006).
Hines, M. R. et al. Hemophagocytic lymphohistiocytosis-like toxicity (carHLH) after CD19-specific CAR T-cell therapy. Br. J. Haematol. 194, 701–707 (2021).
Narayan, V. et al. PSMA-targeting TGFβ-insensitive armored CAR T cells in metastatic castration-resistant prostate cancer: a phase 1 trial. Nat. Med. 28, 724–734 (2022).
Maude, S. L. et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N. Engl. J. Med. 378, 439–448 (2018).
Qi, C. et al. Claudin18.2-specific CAR T cells in gastrointestinal cancers: phase 1 trial interim results. Nat. Med. 28, 1189–1198 (2022).
van de Donk, N. W. C. J., Themeli, M. & Usmani, S. Z. Determinants of response and mechanisms of resistance of CAR T-cell therapy in multiple myeloma. Blood Cancer Discov. 2, 302–318 (2021).
Junghans, R. P. et al. Phase I trial of anti-PSMA designer CAR-T cells in prostate cancer: possible role for interacting interleukin 2-T cell pharmacodynamics as a determinant of clinical response. Prostate 76, 1257–1270 (2016).
Slovin, S. F. et al. A phase I dose escalation trial of vaccine replicon particles (VRP) expressing prostate-specific membrane antigen (PSMA) in subjects with prostate cancer. Vaccine 31, 943–949 (2013).
Hay, K. A. et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor-modified T-cell therapy. Blood 130, 2295–2306 (2017).
Hay, K. A. Cytokine release syndrome and neurotoxicity after CD19 chimeric antigen receptor-modified (CAR-) T cell therapy. Br. J. Haematol. 183, 364–374 (2018).
Neelapu, S. S. et al. Outcomes of older patients in ZUMA-1, a pivotal study of axicabtagene ciloleucel in refractory large B-cell lymphoma. Blood 135, 2106–2109 (2020).
Zettler, M. E. et al. Real-world adverse events associated with CAR T-cell therapy among adults age ≥ 65 years. J. Geriatr. Oncol. 12, 239–242 (2021).
Fabrizio, V. A. et al. Optimal fludarabine lymphodepletion is associated with improved outcomes after CAR T-cell therapy. Blood Adv. 6, 1961–1968 (2022).
Hirayama, A. V. et al. The response to lymphodepletion impacts PFS in patients with aggressive non-Hodgkin lymphoma treated with CD19 CAR T cells. Blood 133, 1876–1887 (2019).
Butler, M. O. et al. The addition of fludarabine to cyclophosphamide for lymphodepleting chemotherapy enhances the persistence of infused NY-ESO-1 TCR anticancer therapy TBI-1301. J. Clin. Oncol. 40, 2539–2539 (2022).
Santomasso, B. D. et al. Management of immune-related adverse events in patients treated with chimeric antigen receptor T-cell therapy: ASCO guideline. J. Clin. Oncol. 39, 3978–3992 (2021).
Sachdeva, M., Duchateau, P., Depil, S., Poirot, L. & Valton, J. Granulocyte-macrophage colony-stimulating factor inactivation in CAR T-cells prevents monocyte-dependent release of key cytokine release syndrome mediators. J. Biol. Chem. 294, 5430–5437 (2019).
Mehta, H. M., Malandra, M. & Corey, S. J. G-CSF and GM-CSF in neutropenia. J. Immunol. 195, 1341–1349 (2015).
Greenbaum, U. et al. CRP and ferritin in addition to the EASIX score predict CAR-T-related toxicity. Blood Adv. 5, 2799–2806 (2021).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Scher, H. I. et al. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J. Clin. Oncol. 34, 1402–1418 (2016).
Lee, D. W. et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol. Blood Marrow Transplant. 25, 625–638 (2019).
Acknowledgements
We thank the patients and their families for participation in this Bellicum Pharmaceuticals-sponsored clinical trial, the study teams at the clinical sites, and the many company employees and consultants who contributed to the study over the years. As study sponsor, Bellicum was involved in the study design, oversaw the data collection, performed the data analysis, and authored the manuscript with all authors providing feedback. We appreciate the team at Emanate Biostats for their biostatistical support which enabled this manuscript. Editorial support was provided by Bryan Tutt, Scientific Editor, Research Medical Library, The University of Texas MD Anderson Cancer Center.
Author information
Authors and Affiliations
Contributions
All investigator co-authors, M.S., E.D., B.T., U.G., M.G., R.R., S.S., M.C., M.B., W.S., and C.B. contributed to the enrollment of study participants. C.B. conceived of the study. C.J., C.S., J.S., and J.H.B. participated in the acquisition and analysis of data in their roles at Bellicum and authored the first draft of the manuscript with all authors providing feedback.
Corresponding author
Ethics declarations
Competing interests
C.J., J.S., J.H.B., and C.S. were employees of Bellicum Pharmaceuticals at the time of the study conduct and manuscript preparation. M.S. consulting or advisory role: Merck Sharp & Dohme, Exelixis, Xencor Research, Janssen Oncology, Vaccitech, Bristol-Myers Squibb/Medarex; research funding: Bellicum Pharmaceuticals, Oncoceutics, Merck Sharp & Dohme, Janseen Oncology, Medivation/Astellas, Advaxis, Suzhou Kintor Pharmaceuticals, Harpoon, Bristol-Myers Squibb, Genocea Biosciences, Lilly, Nektar, Seattle Genetics, Xencor, Tmunity, Exelixis, Regeneron, Bicycle Therapeutics, AstraZeneca. E.D. research or grant funding: Bayer HealthCare Pharmaceuticals Inc., Immunocore LTD., Amgen, Aileron Therapeutics, Compugen Ltd., TRACON Pharmaceuticals Inc., Unum Therapeutics, Gilead Immunomedics, BOLT Therapeutics, Aprea Therapeutics, Bellicum Pharmaceuticals, PMV Pharma, Triumvira Immunologics, Seagen Inc., Mereo BioPharma 5 Inc., Sanofi, Rain Oncology, Astex Therapeutics, Sotio, Poseida, Mersana Therapeutics, Genentech, Boehringer Ingelheim, Dragonfly Therapeutics. Advisory board: BOLT Therapeutics, Mersana Therapeutics, Orum Therapeutics, Summit Therapeutics, PMV Pharma. Speaker: PMV Pharma; travel, accommodations, expenses: ASCO, LFSA Association, Rain Oncology, Banner MD Anderson Cancer Center, Triumvira Immunologics. W.S. has served as a paid consultant (DSMB) for AstraZeneca, Merck, Pfizer, Treadwell Therapeutics; consultant (other): AstraZeneca, Caremark/CVS, EMA Wellness, Fortress Biotech; Speakers Bureau: CME providers (sponsorship unknown): Dava Oncology, Global Academy for Medical Education, OncLive, PeerView, Research to Practice, Vindico; Grant/research support (to institution): Abbvie, Amgen, AstraZeneca, Astellas (Medivation), Bayer, Bristol-Myers-Squibb, Boehringer Ingelheim, Calithera, Clovis, Corvus, Eisai, Exilixis, Genentech (Roche), Johnson & Johnson (Janssen), Merck, Novartis, Pfizer, Seattle Genetics, X4Pharmaceuticals, Xencor; Stockholder: Fortress Biotech; Expert Witness: Apotex, DRL, Mylan, Sandoz; Miscellaneous/Editorial: Cancer (ACS), Up-To-Date, Kidney Cancer Journal. B.A.T. has served as a paid consultant/advisor to Seagen, Exelixis, Lilly, and Sanofi; grant reviewer for Pfizer; and has received research funding (to his institution) from Bristol-Myers Squibb and Bellicum Pharmaceuticals. R.R. has acted as a consultant for Atara Biotherapeutics, Capstan Therapeutics, Gilead Sciences, Incyte Corporation, Instil Bio, Jasper Therapeutics, Midatech Pharma US Inc., Regeneron Pharmaceuticals, Synthekine, Takeda Oncology, TScan. He has served as an expert witness for Bayer CropScience; Travel has been provided by Gilead and Incyte; Additionally, he serves on the End Point Review Committee for OrcaBio and Data and Safety Monitoring for Perelman School of Medicine, University of Pennsylvania. He holds two US patents for methods for treating graft-versus-host disease (US 83/139,490 and US 81/731, 943). M.G.: Speakers’ Bureau—BMS, Lilly, Merck; Advisory board: Sanofi; Consultant: Merck, Celularity, Guardant. He has received research funding from: Acerta Pharma; Adlai Nortye; Arcus Biosciences; Array BioPharma; Bayer; Bellicum Pharmaceuticals; BMS; Boehringer Ingelheim; Celgene; Checkpoint Therapeutics; Compass Therapeutics; Constellation Pharmaceuticals; Cullinan Oncology; Cyteir; Daiichi Sankyo Company; Eisai; EMD Serono; EMD Serono; Erasca, Inc; Fate Therapeutics; Georgetown Univ.; GlaxoSmithKline; GSB Pharma; Hackensack Meridian Health; Imugene; Incyte; Infinity Pharmaceuticals; ITeos Therapeutics; Janssen; Johnson & Johnson; KSQ Therapeutics; MedImmune; Memorial Sloan-Kettering Cancer Center; Merck; Millennium; Mirati Therapeutics; Moderna Therapeutics; NextCure; Nimbus Therapeutics; Pfizer; Pharmacyclics; Rapa Therapeutics; Regeneron; Roche/Genentech; Sanofi; Seagen; Silenseed; Synlogic; Tesaro; Turning Point Therapeutics; Vedanta Biosciences; VelosBio; Verastem; Vincerx Pharma, Amgen, Agenus, AstraZeneca, Beigene, Zailab. U.G. has participated in Speaker Bureau for Incyte. M.A.B. has acted as a paid consultant for and/or as a member of the advisory boards of Exelixis, Bayer, BMS, Eisai, Pfizer, AstraZeneca, Janssen, Calithera Biosciences, Genomic Health, Nektar, EMD Serono, SeaGen, and Sanofi and has received grants to his institution from Merck, Xencor, Bayer, Bristol-Myers Squibb, Genentech/Roche, SeaGen, Incyte, Nektar, AstraZeneca, Tricon Pharmaceuticals, Genome & Company, AAA, Peloton Therapeutics, Bellicum and Pfizer for work performed as outside of the current study. C.B., M.C., and S.S. declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Stein, M.N., Dumbrava, E.E., Teply, B.A. et al. PSCA-targeted BPX-601 CAR T cells with pharmacological activation by rimiducid in metastatic pancreatic and prostate cancer: a phase 1 dose escalation trial. Nat Commun 15, 10743 (2024). https://doi.org/10.1038/s41467-024-53220-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-024-53220-6
This article is cited by
-
Targeting urological cancers with CAR-T cell therapy: current landscape and future directions
Journal of Translational Medicine (2026)
-
Recent advances and future prospects of immunotherapeutic approaches in prostate cancer
Journal of Translational Medicine (2026)
-
T cells in cancer: mechanistic insights and therapeutic advances
Biomarker Research (2025)
-
Small-molecule control of CAR T cells
Nature Reviews Chemistry (2025)
-
Targeting the tumour cell surface in advanced prostate cancer
Nature Reviews Urology (2025)