Abstract
Integrating diverse types of biological data is essential for a holistic understanding of cancer biology, yet it remains challenging due to data heterogeneity, complexity, and sparsity. Addressing this, our study introduces an unsupervised deep learning model, MOSA (Multi-Omic Synthetic Augmentation), specifically designed to integrate and augment the Cancer Dependency Map (DepMap). Harnessing orthogonal multi-omic information, this model successfully generates molecular and phenotypic profiles, resulting in an increase of 32.7% in the number of multi-omic profiles and thereby generating a complete DepMap for 1523 cancer cell lines. The synthetically enhanced data increases statistical power, uncovering less studied mechanisms associated with drug resistance, and refines the identification of genetic associations and clustering of cancer cell lines. By applying SHapley Additive exPlanations (SHAP) for model interpretation, MOSA reveals multi-omic features essential for cell clustering and biomarker identification related to drug and gene dependencies. This understanding is crucial for developing much-needed effective strategies to prioritize cancer targets.
Similar content being viewed by others
Introduction
The growing molecular and phenotypic characterization of cancer cell lines makes them one of the most studied human cell models1. This ever-growing and rich multi-omic data continues to drive the identification of cancer genes and the discovery of therapeutic targets2,3,4. Although genomics has been a primary focus in the search for predictive biomarkers in cancer, recent functional genetic screens conducted by the Cancer Dependency Map (DepMap) consortium revealed that less than 20% of RNAi cancer dependencies could be explained by mutations and copy number alterations5. This highlights the importance of developing holistic machine learning models capable of vertically integrating orthogonal datasets. In this case, vertical integration involves not only genomics but also other types of omics data6.
Despite recent successes of deep learning7 multi-omics integration faces several limitations, most importantly high heterogeneity of different data types (e.g., discrete vs. continuous distributions), intrinsic technological limitations (e.g., missing values), and limited data availability (e.g., in this study, only 25.8% of the cancer cell lines have a complete set of all seven omic datasets under consideration)8. Unsupervised machine learning has been successful in multi-omics integration capturing patterns of data variation shared across different omics9,10. This approach highlighted cancer cellular states associated with epithelial-to-mesenchymal transition (EMT), a key process in drug resistance and metastasis11. Unsupervised deep learning based models can generate improved versions of input datasets by reconstructing missing measurements and correcting experimental error, and thereby augmenting downstream analysis12,13. Although linear dimensionality reduction models10,14 have been designed for similar purposes, the application of deep generative models to large-scale multi-omic cancer cell models is lagging behind. This leaves a gap in the utilization of these non-linear approaches to augment datasets and perform statistical analysis to improve the characterization of cancer mechanisms, biomarkers and drug targets5,15,16. Deep learning models, such as variational autoencoders (VAE), provide more complex formulations of the underlying biological data. Moreover, VAEs have highly flexible designs that can handle data sparsity robustly and are easily extensible to incorporate different data types. In particular, methods based on VAE models have demonstrated significant success in the field of single-cell multi-omics integration and augmentation. However these methods often presuppose the presence of specific data types, such as count data from scRNA-seq and scATAC-seq, limiting their applicability across broader omic landscapes17,18,19,20,21.
Here, we developed a Multi-Omic Synthetic Augmentation (MOSA) VAE model that integrates and synthetically augments multi-omic datasets from >1500 cancer cell lines of the DepMap. MOSA provides a generative unsupervised deep learning model for cancer discovery that utilizes SHapley Additive exPlanations (SHAP)22 values for model explainability, facilitating the identification of underlying biological mechanisms and drug targets. In our study, we systematically evaluated and benchmarked MOSA, demonstrating its generative capacity across independent drug response and proteomic datasets and accurately recovering cancer tissue-of-origin clustering. Additionally, MOSA increased the statistical power to find genomic associations with CRISPR-Cas9 gene essentiality screens. Synthetically screened cancer cell lines revealed vulnerabilities consistent with genomic profiles, such as FLI1-EWSR1 fusion dependency. With MOSA, we generated a complete multi-omic profile across all seven different omics, increasing by 32.7% the number of available screens.
Results
Unifying deep generative model for cancer multi-omics
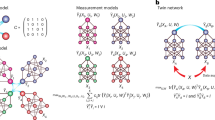
Taking advantage of the DepMap project5,6,23,24, we assembled seven different cancer cell line datasets, i.e., genomics2,3, methylomics25, transcriptomics26, proteomics11, metabolomics27, drug response2,25,28,29, and CRISPR-Cas9 gene essentiality4,30 (Fig. 1a). This comprises a total of 1523 cancer cell lines for which at least two datasets were available (Supplementary Data 1). We designed MOSA tailored to the cancer cell lines multi-omic datasets, performed robust data augmentation, and provided model explanations for biomarker discovery (Fig. 1b, see Methods).
a Cancer cell line multi-omic datasets across the 1523 cancer cell lines. Purple represents measured screens, while orange represents gaps, i.e., missing screens, which were synthetically generated with MOSA. b Schematic of the autoencoder, MOSA, where encoders are represented at the top and decoders at the bottom. For simplicity, the integration of only two datasets is represented. Highlighted designs of MOSA are illustrated on the right. Created in BioRender. Cai, Z. (2023) BioRender.com/m96b457. c Dimensionality reduction visualized using Uniform Manifold Approximation and Projection (UMAP) representation of the trained MOSA joint latent space, where each dot represents a cancer cell line colored according to its tissue of origin.
First, following a late integration31 approach, we trained a separate encoder for each dataset to derive latent embeddings specific to each omic layer. These embeddings were then concatenated and further reduced to formulate a joint multi-omic latent representation (Fig. 1c, Supplementary Data 2). Here, a latent representation is a learned, abstracted feature set (embeddings) within the hidden layers of the neural network that encapsulates the major information from the input data. Compared to a multi-omic linear dimensionality reduction method, MOFA10,14, and another VAE-based method MOVE32, our model provides better separation of cell lines by tissue in the multi-omic latent space (Fig. 1c, Supplementary Fig. 1).
Second, genomics presents a unique challenge due to the sparsity and qualitative nature of its data. To address this, we use only cancer driver events and split genomics into copy number alterations and mutations. While copy number events are integrated as ordinal data through a separate encoder/decoder akin to other omics, mutations are integrated as binary conditionals to each encoder (Fig. 1b, see Methods). The rationale is that genetic backgrounds influence cellular profiles and phenotypes, thereby conditioning other omic layers. The conditional matrix contains genetic alterations in cancer driver genes (including gene fusions), cell line tissue of origin, cell line growth rate measurements, and microsatellite instability information (MSI high), totaling 237 conditional variables (Supplementary Data 3). This conditional matrix is further concatenated to the learned multi-omic joint latent space that works as input for the decoders. Hence, the genetic background and cellular information are crucial for generating latent representations and reconstructing each omic dataset.
Third, compared with similar models for single-cell data12,21,33, the limited number of samples and heterogeneity of the omics available in the DepMap pose significant challenges to training a generalizable model for cancer cell lines. To reduce model complexity, MOSA only considers the most variable features as input for the encoders, while all features are reconstructed by the decoders for synthetic data generation, resulting in an asymmetrical design of VAE (Fig. 1b, Supplementary Fig. 2a, b, Supplementary Data 4). This unique design of MOSA allows us to discard low informative features, such as genes with constant expression and non-essential genes across all cancer cell lines. This reduces the number of trainable parameters by 39.2% while maintaining low reconstruction error.
Fourth, the diverse size of the omic multi-omic datasets may lead to some datasets dominating during training, diminishing the model’s generalizability and explainability. We develop a whole omic (view) dropout layer, which masks a complete omic layer based on a hyperparameter. This provides a significant improvement in the model’s generalization, providing better reconstructions for cancer cell lines by specific omics (see Methods, Fig. 1b). We then perform a multi-omic model explanation by calculating SHAP values22 for all omic input features to assess their importance for the latent space integration and the reconstruction of omic features (see Methods). This provides a systematic resource to explore potential nonlinear cancer genotype-phenotype associations.
Taken together, MOSA provides an unsupervised model that integrates all cancer cell line omics simultaneously. Using a 10-fold cross-validation strategy, MOSA’s reconstructed hold-out folds for CRISPR-Cas9 and drug responses were robustly correlated with the original data (mean feature Pearson’s r of 0.35 and 0.65, respectively) (Fig. 2a, Supplementary Fig. 3, Supplementary Data 5). MOSA performed better compared to a similar systematic supervised analysis designed to predict each CRISPR-Cas9 gene dependency either using core-omics (e.g., genomics, transcriptomics), only genomic, or only functionally related genes (mean feature best Pearson’s r = 0.25)34.
a MOSA reconstruction quality measured using a 10-fold cross-validation. After reconstructing all test folds, they are concatenated and the reconstruction quality score is calculated as the Pearson’s r between the reconstructed and actual measured values. Features ranked by their reconstruction quality are shown for the drug response (left) and the CRISPR-Cas9 (right) datasets. Duplicated drug names represent replicated screens for the same drug. Representative examples of strongly selective CRISPR-Cas9 and drug responses are labeled. b MOSA’s partial dataset augmentation (missing value imputation) of drug IC50s compared to recent independent drug response screens. c–e, similar to b, using MOFA, MOVE and mean imputed values, respectively.
Evaluation of multi-omics synthetic data generation
A significant advantage of multi-omic vertical integration and unsupervised deep-generative models is their ability to synthetically generate datasets that are missing in specific samples, such as reconstructing a dataset that is entirely absent for certain cell lines. This is particularly crucial given the pervasive dataset gaps, even in well-characterized models such as cancer cell lines (Fig. 1a). Multi-omic profiling is both costly and labor-intensive, thus data-driven generative models are key to prioritizing the design of the most informative experiments. However, benchmarking generative models is challenging as it requires independent, ideally large-scale, datasets to validate the model’s predictions. We initially tested 16 multi-omics integration methods (Supplementary Data 6, see Methods), but due to constraints such as the number of omics supported, type of data distribution, and limitations in design and implementation, we were narrowed to three state-of-the-art methods: MOFA10,14, MOVE32, and mixOmics35,36. These methods, encompassing linear, VAE-based, and correlation analysis approaches, were capable of integrating all seven omics datasets considered here. We have delineated a series of benchmarks over the following sections into increasing model complexity.
MOSA reconstructs the input data matrices by leveraging the multi-omic latent space learned from the original data. Data reconstruction generates complete omic matrices, thus handling both missing values (partial dataset augmentation), and more importantly, reconstructing whole-omics (full dataset augmentation) through vertical integration (at least two omics are required for a cell line to be considered in this study). For partial dataset augmentation, MOSA imputes incomplete features, e.g., measurements for certain proteins are sparse due to technical limitations commonly found in mass-spectrometry-based proteomics data11,37. A recent and independent drug response dataset, that is completely absent during model training, was accurately reconstructed (IC50s, Pearson’s r = 0.87, n = 32,659) (Fig. 2b), outperforming MOFA10,14, MOVE32 and naive mean imputation (Fig. 2c–e). Pronounced discrepancies between MOSA’s reconstruction and the original datasets revealed likely inaccurate experimental measurements. For example, the response to the MEK1/2 inhibitor trametinib was not consistent with replicate measurements and drugs with the same canonical target in the same cell line (Supplementary Fig. 4a). Such discrepancies also spotlighted drugs (e.g., venetoclax) or classes of drugs (e.g., antiapoptotic inhibitors) for which no effective molecular biomarkers are available (Supplementary Fig. 4b), underlining the challenge of devising reliable predictive models for their response. Additionally, proteomics is riddled with missing values (Supplementary Fig. 5a), affecting more predominantly lowly abundant proteins. MOSA augmented the proteomics data by filling approximately 32% of the original matrix using information from all omics, while preserving sample correlations with an independent proteomic dataset (CCLE38) (Supplementary Fig. 5b, Supplementary Data 7). Notably, MOSA effectively reconstructed the protein profiles of SMAD4 in cell lines characterized by SMAD4 gene deletions, which are typically associated with low SMAD4 gene expression and protein abundance (Supplementary Fig. 5c). The MOSA-augmented proteomic matrix preserves the ability to identify protein interactions through protein pairwise correlations39 (Supplementary Fig. 5d). In contrast to the original matrix that has missing values, MOSA’s augmented protein matrix is complete and directly usable for downstream analysis, such as generalized linear models40, which improved the recall of protein complex interactions (Supplementary Fig. 5d).
Subsequently, full dataset augmentation was assessed. Synthetic proteomic data generated by MOSA for cancer cell lines lacking proteomic measurements showed correlations with independent proteomic measurements comparable to those of cell lines that had actual proteomic data (Fig. 3a). For drug response, reconstructions of 107 overlapping drugs correlated robustly with measurements in an independent dataset (CTD241,42) (Fig. 3b). Lastly, we performed a similar analysis using independently processed transcriptomics, which included data for 272 cancer cell lines that did not have transcriptomics data during the training of MOSA26. MOSA’s transcriptomic reconstructions were strongly correlated with real data even for cell lines with no transcriptomics data for training (mean pearson’s r = 0.90) (Supplementary Fig. 5e). Crucially, this shows the capacity of MOSA as a generative model for synthetic cancer cell line multi-omic and phenotypic screening.
a Distribution of proteomics cancer cell lines correlation with an independent dataset (CCLE38) grouped by whether the cancer cell line had proteomic data for the model training (orange, n = 291) versus cell lines without any proteomics prior (light blue, n = 78). b Distribution of cancer cell line correlations (Pearson’s r) between an independent drug response dataset (CTD241,42) and the MOSA reconstructed dataset, grouped by whether the cancer cell line had prior availability of drug response in the datasets for the model training (orange, n = 571) versus cell lines without drug response data (light blue, n = 239). c One-sided log-ratio test p-value of genetic associations with CRISPR-Cas9 gene essentiality with the original dataset (x-axis) and the augmented MOSA dataset (y-axis). False discovery rate (FDR) correction is applied using the Benjamini-Hochberg method to adjust for multiple comparisons. d Fisher skew test per gene across the original CRISPR-Cas9 dataset (x-axis) and the MOSA augmented dataset (y-axis). Dot size represents the number of cell lines that have the gene as essential (scaled log2 fold-change < −0.5) in the original dataset. e Correlation between BRAF and MAPK1 CRISPR-Cas9 gene essentialities using both previous measured (Observed) and the synthetically reconstructed (Reconstructed). Gene essentiality scores are represented using copy-number corrected78 log2 fold-changes scaled by the median of common essential (score = −1) and non-essential (score = 0) genes30. Gene essentialities are also grouped according to the presence or absence of a BRAF mutation, mostly V600E gain-of-function mutations. f CRISPR-Cas9 gene essentiality association with FLI1-EWSR1 fusion. Confidence intervals of 95% are displayed for the regression lines in panels d, e, and f. Box-and-whisker plots show 1.5× interquartile ranges, centers indicate medians in panels e and f.
We evaluated downstream analysis by comparing the original data matrices with the augmented ones. MOSA increased by 34.9% the number of CRISPR-Cas9 cell line screens, and the augmented dataset improved the statistical power to find genetic associations (Fig. 3c, Supplementary Data 8). Gene essentiality specificity (Fisher’s skewness test), which can be used to identify selective cancer vulnerabilities, showed a moderate positive correlation (Pearson’s r = 0.52) between the synthetic CRISPR-Cas9 screened cell lines and the previously available screens (Fig. 3d). Nonetheless, this correlation is likely underestimated due to the presence of potential outlier non-essential genes. MOSA accurately reconstructed gene dependencies, for example, BRAF dependency in BRAF gain-of-function mutant cancer cell lines (Fig. 3e), and FLI1 dependency in cell lines harboring an FLI1-EWSR1 fusion gene (Fig. 3f).
Lastly, we aimed to assess the advantages of developing a method capable of natively integrating more than two omics. Specifically, we focused on transcriptomics and drug response datasets, which represent molecular and phenotypic datasets, respectively. These are also commonly utilized in multi-omics integration and are among the most informative omic types for our benchmarks. From the list of methods we evaluated, we considered iClusterPlus43, JAMIE18, scVAEIT44, and moCluster45 (Supplementary Data 6, see Methods). MOSA provided a better reconstruction of transcriptomics and drug response data (Supplementary Fig. 6a, b). Particularly, adding more omics to MOSA provided a significant improvement over existing methods, supporting the utility of using holistic multi-omics models. Furthermore, MOSA consistently outperformed the other methods in tissue of origin clustering (Supplementary Fig. 6c). Considering only transcriptomics and drug response resulted in the best tissue of origin clustering, reflecting the strong structuring of these omics by tissue of origin46. In contrast, other omics such as proteomics and metabolomics are more loosely structured by tissue11,47. Consequently, including omics that are less strongly structured by tissue will naturally result in looser tissue clustering.
Taken together, these diverse examples demonstrate MOSA’s ability to perform both partial and full dataset augmentation validated using various independent datasets and from different laboratories. The generation of large-scale multi-omic datasets is both time and resource-intensive, thereby positioning MOSA as a valuable tool for in silico testing and prioritization of drug targets for experimental validation.
Model interpretation reveals cancer cell states
To prioritize the most promising targets, a model needs to be explainable beyond producing reliable predictions. Hence, we used the SHAP22 algorithm to calculate the feature importance, defined as the amount of contribution of each feature to the latent space (Fig. 1b, Supplementary Data 9, see Methods). When grouping features by their corresponding omic datasets, we observed that metabolomics, drug response, and copy number alterations exhibited the highest average feature importance (Supplementary Fig. 7a). Regarding conditional features, although their average feature importance was modest, certain key features, such as TP53 mutation, growth rate, and tissue of hematopoietic and lymphoid origin emerged as highly significant, even when compared with other omic datasets (Fig. 4a, Supplementary Data 9). This underscores the importance of incorporating conditional variables into the model. Features ranked in the top five from each omic dataset also validated the capacity of our approach to recover well-established molecular processes associated with cancer (Fig. 4a), for example, CDKN2A copy number alterations, as well as sensitivity to the SRC family inhibitor, dasatinib. Interestingly, other less obvious features that were highly ranked shed light on previously less explored biological mechanisms. One specific example is the metabolite, 1-methylnicotinamide involved in the nicotinate and nicotinamide metabolism, which was calculated to be the most important feature in the metabolomics towards the multi-omics latent representation (Fig. 4a). We observed a strong relation between increased 1-methylnicotinamide intracellular abundance and the overexpression of Nicotinamide N-Methyltransferase (NNMT) enzyme, which catalyzes the production of this metabolite (Supplementary Fig. 7b). We also observed an association between 1-methylnicotinamide and the EMT state of cancer cell lines, as corroborated by the expression of VIM and CDH111 (Supplementary Fig. 7c, d). This confirms a recent single-cell study’s finding that the PC-9 non-small cell lung carcinoma line, which harbors an activating EGFR mutation, develops a cellular state resistant to EGFR inhibitors through expression of EMT markers as well as accumulation of 1-methylnicotinamide48. Additionally, 1-methylnicotinamide was observed with a significant increase during the early stages of EMT in the A549 cell line, and this increase was associated with changes in glycolytic metabolites and histone post-translational modifications, indicating a link between 1-methylnicotinamide and epigenetic modifications during EMT49. While further experimental validation is necessary, this could pave the way for the identification of cancer cellular states underlying drug resistance.
To delve deeper, we subsequently used the SHAP algorithm to calculate the feature importance specifically for the reconstruction of drug response, thereby facilitating the discovery the most promising biomarkers (see Methods). As expected, the drug response features themselves were the most important features on average (Supplementary Fig. 8a, Supplementary Data 10). Notably, the conditionals emerged as the second most important omics, reflecting the critical role of tissue of origins, mutations, and growth rate in influencing drug responses (Supplementary Fig. 8a). Centering on the metabolite 1-methylnicotinamide, drugs known to be EMT-related were ranked as the top drugs showing high feature importance from 1-methylnicotinamide (Fig. 4b). All the top five drugs, except Daraprim (Pyrimethamine) which was not included in the dataset as an anti-cancer drug, were found to be related to EMT in recent studies. Specifically, UNC063850, Entinostat51, and BIX0218952 suppress EMT, while methotrexate53 shows the ability to induce EMT. This finding suggests that the top-ranked drug Daraprim may also harbor a close relation to EMT, presenting a potential avenue for repurposing in cancer treatment. Other EMT-related features such as GPX1 protein intensity54 also ranked as top features for Daraprim, indicating the potential to utilize other features in the list for the discovery of the most promising biomarkers for drug response (Fig. 4c). Among the other top features for the top drugs, KRAS and KMT2D were consistently identified as being of high importance, and both of these genes have been implicated in EMT55,56 (Supplementary Fig. 8b–f). Lastly, we utilized an external metabolomic dataset47 to validate the drugs associated with 1-methylnicotinamide by SHAP values. Although the abundance of 1-methylnicotinamide was not directly measured in their study, we analyzed the drugs linked to nicotinate and nicotinamide metabolism, where 1-methylnicotinamide is a direct product of nicotinamide methylation. Several highlighted drugs identified by SHAP values, including Daraprim, UNC0638, Entinostat (MS-275), and PAC-1, were also ranked highly as either resistant or sensitive drugs (Supplementary Fig. 9).
Taken together, our findings suggest a broad association of 1-methylnicotinamide and EMT across hundreds of cancer cell lines with a potential role in drug resistance. While further assessment is needed to substantiate this, more generally, it unveils the possibility of using MOSA as a holistic model that integrates molecular and phenotypic data of cancer cells to investigate cancer cell states, drug resistance and their underlying mechanisms.
Discussion
The application of deep generative models, including MOSA, in cancer research is promising but comes with limitations, mainly related to the restricted sample size which impaired exploring more complex VAE designs, and more complex designs led to worse dataset reconstructions. While the overall reconstruction of the datasets was robust, there are examples where it could be improved, particularly for proteomics where intrinsic data sparseness makes it more challenging for the model to train successfully. Thus, the addition of more characterized cancer models will likely allow us to train better models and reduce reconstruction error. Future efforts should leverage multi-omic resources from cancer patients and derived models, such as organoids and patient derived xenografts (PDXs), to enhance training and explore transfer learning opportunities. In addition to tabular omic data, VAEs have demonstrated great success integrating image and text-based data57,58, and MOSA can be further enhanced to integrate these types of data and enable multi-modal data augmentation. We also aim to address the complex challenge of data missing not at random (MNAR), a scenario commonly encountered in omics datasets, by adapting VAE architectures to more accurately identify and handle MNAR scenarios59,60,61. SHAP analysis offers an explanation for deep learning models, however, there are still some obstacles in verifying the biological significance of certain highlighted features. These challenges could be associated with the inherent limitations of SHAP and Shapley values62, thus additional research is required to ascertain the importance of these emphasized features. Furthermore, while this has provided strong initial support for the EMT-related associations, further experimental work is necessary to validate and confirm these findings across different cancer cell models.
In summary, MOSA augmented the multi-omic profiles of 1523 cancer cell lines by robustly filling in gaps in the existing experimental screens. Deep learning-based synthetic data generation can augment experimental screens by facilitating the creation of realistic datasets to guide experimental design and accelerate the validation of the most promising targets. Looking ahead, this model is readily adaptable to integrate other types of data modalities, such as imaging, further enabling the discovery of molecular/phenotype associations.
Methods
Cancer cell line multi-omic data collection
The aim was to assemble the most up-to-date and comprehensive molecular, phenotypic and cancer cell line sample information. All datasets were downloaded from the DepMap (https://depmap.org/), and the CellModelPassports (https://cellmodelpassports.sanger.ac.uk/)23 portals, with the exception of the metabolomics data which were taken directly from the original publication supplementary materials27. For reproducibility, all data used in this study are provided in a figshare repository (see Code and data availability).
We integrated genomics2,63, transcriptomics26, methylomics25, proteomics11, metabolomics27, drug response25,28,29, and CRISPR-Cas9 gene essentiality4,64. This comprised a total of 1523 cancer cell lines with at least two datasets available for each cell line. All datasets have been previously processed, normalized/scaled, and batch corrected in each of their individual publications addressing technical and design aspects important to each dataset (e.g., integration of CRISPR-Cas9 screens across different laboratories65, driver mutations and copy number alterations, and gene expression samples from different datasets26).
Cancer cell line validation datasets
Three independent datasets were used in this study for validation, i.e. they were not used for model training. The first dataset presents the CCLE proteomic characterization of 375 cancer lines38, of which 291 comprise the proteomic dataset11 used for training. The second dataset represents recent drug response screens with the same platform as the drug screens used for training25,28,29 that were obtained from the Genomics of Drug Sensitivity in Cancer (GDSC) portal (https://www.cancerrxgene.org/)66 comprising a total of 32,659 IC50s measured across 313 unique drugs and 781 overlapping cancer cell lines. The third dataset is an independent drug response dataset (CTD2)41,42, comprising a total of 545 drugs and 887 cancer cell lines, for which 106 and 575, respectively, overlap with the drug response data used for training25,28,29.
Data preprocessing
A total of seven datasets were considered: copy number (n = 777 features); methylome (n = 14,608); transcriptome (n = 15,278); proteome (n = 4922); metabolome (n = 225); drug response (n = 810); and CRISPR-Cas9 gene essentiality (n = 17,931). A total of 1523 cancer cell lines were profiled with each cell line having at least two of these datasets.
For CRISPR-Cas9 gene essentiality, transcriptomic and methylomic feature reduction was performed to exclude lowly variable features. For gene essentiality, samples were scaled using essential and non-essential genes making their median per sample -1 and 0, respectively. Never essential genes were discarded, i.e., genes that do not have an essentiality profile lower than 50% of the median log2 fold-change of essential genes in at least one cell line were removed. For transcriptomics and methylomics, a standard deviation filter was applied. By taking the standard deviation of all genes across samples, a Gaussian mixture model (k = 2) was fitted, identifying lowly variable genes and the rest. A standard deviation threshold was defined as the rightmost intercept of the two Gaussian distributions (Supplementary Fig. 2a), and any gene with a standard deviation lower than that was discarded. Moreover, for the proteomic, drug response, metabolomic and CRISPR-Cas9 datasets, any feature with a missing rate higher than 85% was discarded. All datasets were standardized by z-score, except copy number. Missing values were replaced with 0 and their position in the original dataset was stored for use in the model (e.g., to exclude them from the loss functions). In addition to these seven datasets, driver gene mutations, fusion genes, microsatellite instability, growth rate, cancer and tissue type information were concatenated into a single matrix to be used as labels of the cancer cell lines.
Multi-omics synthetic augmentation (MOSA)
MOSA is a conditional multi-view variational autoencoder implemented using PyTorch (v2.0)67. In the next section, we describe MOSA’s architecture, use of conditionals, dropout layer and SHAP explainability analysis.
Architecture
MOSA follows a traditional design of conditional VAEs (Fig. 1b). For each of the seven datasets (views), an encoder is trained with multiple fully connected layers, which are all proportional to the number of input features of the dataset plus the number of labels (concatenated conditionals). First, joint fully connected layers take as input each dataset and reduce them to a fixed number of joint latent dimensions. Different techniques were tested to integrate the omic-specific latent dimensions (e.g., product of experts), but concatenation obtained the smallest reconstruction loss. The multi-omics joint latent dimensions are further reduced to a specified number of latent dimensions (hyperparameter). Then, the joint layer outputs two layers representing Gaussian distribution mean and variance. These are important for the regularization of the latent space and are used to sample the latent dimensions. Finally, the latent dimensions (z) are concatenated with the conditionals and provided to the decoders of each dataset. The decoders have a similar but inverse architecture to the encoders.
Conditionals
We introduced a conditional architecture to enhance the model’s reconstruction performance and biological relevance. Conditionals (n = 237) include key biological features, such as cancer driver mutations, tissue types, gene fusions, MSI status, and cell line growth rate. These were used in two stages in model architecture: 1) concatenated to each omic layer prior to encoding; 2) concatenated to the multi-omic joint latent representation before decoding. The conditional concatenation serves two crucial purposes: it contextualizes the input data within specific cellular or genetic backgrounds, and it allows the decoder to generate condition-specific reconstructions of the data. The inclusion of conditionals offered several advantages. First, it ensured that the model was not merely capturing patterns within individual omic layers in isolation. Instead, complex interactions among multi-omic data and genomic and physiological variables were accounted for, facilitating a more holistic understanding of the underlying biological processes and phenomena. Second, by embedding these conditionals into the decoder, the model can generate data reconstructions contextualized to specific cell line conditions.
View dropout layer
A special dropout strategy, namely the view dropout layer, was included in MOSA to both improve the model’s predictive power and interpretability. Unlike traditional dropout layers, which randomly set individual features to zero, the view dropout layer zeroes out all the input features of a single omic layer. This approach encouraged the model to reconstruct the data by learning the relationships among multiple omic layers, rather than relying on one specific omic layer. For example, in generating drug response predictions, the MOSA model could disproportionately emphasize the input drug response data, neglecting the potential contributions from other omic layers, such as transcriptomic and proteomic data. By using the view dropout layer, we significantly improved the latent space cell line separation (Fig. 1c, Supplementary Figs. 1b, 10a, b) and reconstruction for both the proteomic (Fig. 3a, Supplementary Fig. 10c) and drug response data (Supplementary Fig. 10d). The dropout rate for this layer is controlled by the hyperparameter view_dropout, which was optimally set as 0.5 for the final model.
Model explanation via SHapley Additive exPlanations (SHAP)
For model explanation, we used the Python package SHAP22 (v0.42.1) with technical modifications to support the multi-omic data as the input to MOSA. Specifically, the GradientExplainer, which combines IntegratedGradient68 and SmoothGrad69, was used to calculate the changes of the gradients on the model’s output regarding its input to attribute an importance value to each feature. The SHAP calculation was performed in two ways.
First, SHAP was run to explain the encoder part of MOSA, treating the integrated latent dimensions as the output. The result contains SHAP values in a multidimensional array with shapes of \(({N}_{{latent\_}\dim },\,{N}_{{samples}},\,{{N}}_{{features}})\), where each \(N\) represents the number of latent dimensions, samples and features, respectively. To achieve the global level feature importance for analysis, the multidimensional array was first taken as the absolute value to account for both positive and negative impact, and then summed across latent dimensions, followed by averaging by samples. This then resulted in a list of length \({N}_{{features}}\), representing the overall feature importance contributing to the latent space (Fig. 4a).
Second, SHAP was run to explain MOSA’s reconstruction of each omic dataset. Taking drug response as an example, similarly to explaining the latent space, the shape of the SHAP values is \(({N}_{{drugs}},\,{N}_{{samples}},\,{{N}}_{{features}})\), where \({N}_{{drugs}}\) represents the number of drugs, and \({N}_{{samples}},\,{N}_{{features}}\) are described as above. In this analysis, the array was only averaged across samples, resulting in a 2D array of \(({N}_{{drugs}},\,{N}_{{features}})\), which measures the feature importance for each drug. The feature 1-methylnicotinamide metabolite was first selected and the drugs that had the highest SHAP values were analyzed to identify EMT-related drugs (Fig. 4b). Other important features for the drugs of interest were then ranked by selecting the row of the drug and then ranking the features in the descending order (Fig. 4c). Due to the limitation of the computational resource, 20% of the samples were randomly selected to compute the feature importance for reconstructing drug response and copy number datasets, while 20 samples were randomly selected for other omic datasets which have much larger number of dimensions.
Overall, the SHAP analysis allowed us to identify features that are important for the multi-omic latent dimension and for explaining the reconstruction of features, such as drug response. Feature importance aggregated across all the samples and output dimensions can be found in Supplementary Data 9 and 10. More granular feature importances for each output dimension can be downloaded from the figshare repository provided in the code and data availability section.
Loss function
The loss function is the summation of three components: 1) Reconstruction error across all input datasets; 2) weighted variational Kullback–Leibler (KL) regularization term of the multi-omic joint latent dimensions70; and 3) a contrastive loss using tissue types as labels:
The reconstruction loss\(\,{L}_{{reconstruction}}\) is defined as:
Where \({l}_{d}\) represents the reconstruction loss for dataset d, calculated using the mean squared error (MSE)71,72.
In Eq. (1) the λ and α are optimized hyperparameters to weight the KL divergence and contrastive loss terms, respectively. \({L}_{{KL}}\) calculates the KL divergence between the learned gaussian distribution with mean (\(\mu\)) and variance (\({\sigma }^{2}\)) of the VAE and a standard normal prior distribution70.
The last part of the loss function is a contrastive loss defined as:
where \({s}_{p}\) and \({s}_{n}\) represents the cosine similarity between positive pairs and negative pairs, which are defined by whether two samples have the same tissue type. \({m}_{{pos}}\) and \({m}_{{neg}}\) are positive and negative margins, which are hyperparameters tuned as described in the section below.
Asymmetrical VAE
MOSA was also engineered with an asymmetrical structure to optimize model efficiency by reducing the number of parameters. Specifically, feature selection was conducted in a data-type-specific manner before the encoding process. For transcriptomic and methylation data, only features that exhibited high variability were selected as input to the model. Highly variable features were defined using a gaussian mixture model with two components fitted to the standard deviation of all features, thus capturing two distributions of lowly and highly variable features. The standard deviation threshold is defined as the biggest value at which the densities of the two distributions are equal, hence features with a standard deviation greater than 1.122 for transcriptomic data and 0.064 for methylation data are considered highly variable and selected as input for the encoder. For CRISPR-Cas9 data, gene knock-outs that did not significantly impact any cell line, as indicated by a gene fitness score higher than −0.5 in every cell line, were excluded from the input layer. This targeted feature selection effectively reduced the model’s computational burden. Despite this reduction in input complexity, all available features were included during the decoding process to reconstruct the data. This asymmetrical design was chosen for its ability to maintain the model’s predictive and reconstructive capacities while streamlining its architecture.
Hyperparameters
The choice of hyperparameters (Table 1) was guided by an automatic optimization framework based on parallel trials (Optuna73) and then manually adjusted. For each run a stratified shuffle split is performed, stratifying by hematopoietic and lymphoid cell lines, leaving 20% of the samples for testing. A total of 600 trials were performed, where each trial was capped to 150 epochs.
Benchmark state-of-the-art methods
For comparison with the unsupervised multi-omics approach taken by MOSA, 16 multi-omics integration methods were tested. However, as listed in Supplementary Data 6, for most of the models, we encountered issues related to intrinsic design and implementation choices. These included, for example, limitations on the number of supported omic modalities and specific designs tailored only for count data processing since many of the models are designed for single-cell data. Therefore, we have managed to run and systematically benchmark our results for all seven omics datasets considered against three other state-of-the-art methods for multi-omics data integration, including MOFA10,14 as a linear multi-omics dimensionality reduction approach, MOVE32 as a VAE-based approach, and mixOmics35,36, which is based on generalized canonical correlation analysis. To make comparisons as close as possible and focus solely on methodological differences, the same data preprocessing was used for MOSA, MOFA, MOVE and mixOmics. Similarly, the number of factors for MOFA was initially set to the same optimal number of joint latent dimensions, i.e., 200 (Table 1). However, this generated poorly performant results, i.e., poorly reconstructed datasets. Through manual exploration, the optimal number of factors was set to 100, which was automatically reduced during training to 97 by discarding factors with variance explained lower than 0.0001. Each view was scaled independently, and the model was run until it converged (convergence_mode = slow). The number of dimensions was successfully set as 200 in MOVE. Since mixOmics requires the number of dimensions separately associated with each omic dataset, 210 dimensions were used in mixOmics to achieve the closest comparison. The conditionals layer in MOSA contains both binary, e.g., mutations and tissue of origin, and continuous, e.g., cancer cell line growth rates and doubling times from independent studies, features. These data were included as a separate layer in MOVE, however, MOFA does not support a mixed distributed view, e.g., Gaussian and Bernoulli. Thus we could not integrate the growth rate and doubling time in the conditional view, which apart from these two have only binary features, and therefore the prior likelihood distribution was set to Bernoulli. These configurations produced the best multi-omic dimensionality reduction and view reconstruction using MOFA. The optimized model was saved as an HDF5 file and is also provided in the figshare repository. Similarly, the tissue-of-origin data was used as the target variable in mixOmics following the documentation of the package. Specifically, the DIABLO mode36 (N-integration) in the mixOmics suite, which was an extension to the original mixOmics toolset35, was used for the multi-omics data integration task in this study.
In order to evaluate MOSA more comprehensively and to address the limitations of many state-of-the-art methods that support only a limited number of omic modalities, we conducted a separate benchmarking analysis considering only two omic modalities as input. This approach allowed us to include four additional methods: JAMIE18, scVAEIT44, iClusterPlus74 and moCluster45. Transcriptomic and drug response data were used to train and benchmark MOSA against seven other methods, as these omic types are the focus of our benchmarks. Since only two omics were included, we removed the requirement for a sample to have data from at least two omics. JAMIE, iClusterPlus and moCluster were successfully run using 200 dimensions for the integrated latent space, which was the same as MOSA. However, scVAEIT with 200 latent dimensions generated poor results, especially for the latent space clustering comparison. Similar to MOFA, we manually searched for the optimal setting and decided on using 100 latent dimensions for scVAEIT. Additionally, Gaussian distribution was set for the dist_block hyperparameter for both the transcriptomic and drug response data. MOSA, MOFA, MOVE, JAMIE and scVAEIT were evaluated for both synthetic data reconstruction and clustering performance, while mixOmics, iClusterPlus, and moCluster were only included in the latent space clustering comparison as they are not generative models. To ensure fair comparisons, conditionals were not incorporated into any of the selected methods during training.
Protein-protein interaction co-abundance analysis
Protein-protein interactions (PPIs) were estimated using two methods to compare the ability of MOSA augmented proteomics matrix and the original proteomic matrix to recapitulate PPIs present in specific protein interaction resources datasets: CORUM75, BioGRID76 and STRING77. The first method, Pearson’s r, has been previously used for this task39. Due to its inherent limitations, e.g., its inability to account for confounding effects and data structure, a new method, similar to that described by Wainberg et al.40 based on a generalized linear model (GLM) was tested. This method applies Cholesky’s Whitening transformation to proteomics data by using the inverse of its covariance matrix, which decorrelates samples and pushes data towards normality. This transformed data is then used in an ordinary least squares (OLS), whose calculated weights are a correlative metric between two proteins. Each method was calculated for every protein pair, with all pairs being ordered for each method by ascending p-value. Afterwards, a curve was drawn based on the cumulative sum of presence of that pair on a PPI set, either \(\frac{1}{k}\) (presence) or 0 (absence), where \(k\) is the total number of present pairs. Thus, the better the method, the greater the AUC of the recall curve.
Statistics & reproducibility
Sample sizes were determined by the availability of cancer cell lines and the associated multi-omic datasets from the Cancer Dependency Map (DepMap). A total of 1523 cancer cell lines were included, for which at least two datasets were available. No statistical method was used to predetermine sample size. Data exclusion details can be found under the Data preprocessing section in Methods. Data were randomly split for cross-validation purposes. The randomization was stratified by hematopoietic and lymphoid cell lines to ensure balanced representation across cell line types and distinct culture conditions, i.e. suspension vs adherent. Blinding was not applicable to this study, as all analyses were conducted using publicly available in vitro data from cancer cell lines. The findings were validated using independent datasets for proteomics (CCLE), drug response (GDSC and CTD2), and transcriptomics (DepMap). A 10-fold cross-validation strategy was applied to assess the reproducibility of the MOSA model across multiple omics layers.
Inclusion and ethics
All authors have committed to upholding the principles of research ethics and inclusion as advocated by the Nature Portfolio journals.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data were assembled from the Cancer DepMap and synthetic datasets generated have been deposited in figshare under the following URLS: DepMap datasets: https://doi.org/10.6084/m9.figshare.24420580. https://doi.org/10.6084/m9.figshare.24420598. MOSA augmented datasets and latent representation: https://doi.org/10.6084/m9.figshare.24562765. MOSA feature importance: https://doi.org/10.6084/m9.figshare.24473005. MOFA multi-omics reconstruction and latent representation: https://doi.org/10.6084/m9.figshare.24420631. MixOmics multi-omics latent representation: https://doi.org/10.6084/m9.figshare.25764408. MOVE diabetes multi-omics reconstruction and latent representation: https://doi.org/10.6084/m9.figshare.25764438.
Code availability
All code is available at https://github.com/QuantitativeBiology/PhenPred (https://doi.org/10.5281/zenodo.13945138). The pretrained weights of MOSA are available at https://huggingface.co/QuantitativeBiology/MOSA_pretrained (https://doi.org/10.57967/hf/3634).
Change history
04 February 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41467-025-56686-0
References
Trastulla, L., Noorbakhsh, J., Vazquez, F., McFarland, J. & Iorio, F. Computational estimation of quality and clinical relevance of cancer cell lines. Mol. Syst. Biol. 18, e11017 (2022).
Garnett, M. J. et al. Systematic identification of genomic markers of drug sensitivity in cancer cells. Nature 483, 570–575 (2012).
Barretina, J. et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 483, 603–607 (2012).
Behan, F. M. et al. Prioritization of cancer therapeutic targets using CRISPR–Cas9 screens. Nature 568, 511–516 (2019).
Tsherniak, A. et al. Defining a Cancer Dependency Map. Cell 170, 564–576.e16 (2017).
Pacini, C. et al. A comprehensive clinically informed map of dependencies in cancer cells and framework for target prioritization. Cancer Cell 42, 301–316.e9 (2024).
Wekesa, J. S. & Kimwele, M. A review of multi-omics data integration through deep learning approaches for disease diagnosis, prognosis, and treatment. Front. Genet. 14, 1199087 (2023).
Cai, Z., Poulos, R. C., Liu, J. & Zhong, Q. Machine learning for multi-omics data integration in cancer. iScience 25, 103798 (2022).
Argelaguet, R. et al. Multi-omics profiling of mouse gastrulation at single-cell resolution. Nature 576, 487–491 (2019).
Argelaguet, R. et al. MOFA+: a statistical framework for comprehensive integration of multi-modal single-cell data. Genome Biol. 21, 111 (2020).
Gonçalves, E. et al. Pan-cancer proteomic map of 949 human cell lines. Cancer Cell 40, 835–849.e8 (2022).
Eraslan, G., Simon, L. M., Mircea, M., Mueller, N. S. & Theis, F. J. Single-cell RNA-seq denoising using a deep count autoencoder. Nat. Commun. 10, 390 (2019).
Freeman, B. A. et al. MIRTH: Metabolite Imputation via Rank-Transformation and Harmonization. Genome Biol. 23, 184 (2022).
Argelaguet, R. et al. Multi-Omics Factor Analysis-a framework for unsupervised integration of multi-omics data sets. Mol. Syst. Biol. 14, e8124 (2018).
Boehm, J. S. et al. Cancer research needs a better map. Nature 589, 514–516 (2021).
Poulos, R. C., Cai, Z., Robinson, P. J., Reddel, R. R. & Zhong, Q. Opportunities for pharmacoproteomics in biomarker discovery. Proteomics 23, e2200031 (2023).
Minoura, K., Abe, K., Nam, H., Nishikawa, H. & Shimamura, T. A mixture-of-experts deep generative model for integrated analysis of single-cell multiomics data. Cell Rep. Methods 1, 100071 (2021).
Cohen Kalafut, N., Huang, X. & Wang, D. Joint variational autoencoders for multimodal imputation and embedding. Nat. Mach. Intell. 5, 631–642 (2023).
He, Z. et al. Mosaic integration and knowledge transfer of single-cell multimodal data with MIDAS. Nat. Biotechnol. 42, 1594–1605 (2024).
Ghazanfar, S., Guibentif, C. & Marioni, J. C. Stabilized mosaic single-cell data integration using unshared features. Nat. Biotechnol. 42, 284–292 (2024).
Ashuach, T. et al. MultiVI: deep generative model for the integration of multimodal data. Nat. Methods 20, 1222–1231 (2023).
Lundberg, S. M. & Lee, S.-I. A Unified Approach to Interpreting Model Predictions. In Advances in Neural Information Processing Systems (eds. Guyon, I. et al.) vol. 30 (Curran Associates, Inc., 2017).
van der Meer, D. et al. Cell Model Passports-a hub for clinical, genetic and functional datasets of preclinical cancer models. Nucleic Acids Res. 47, D923–D929 (2019).
Dwane, L. et al. Project Score database: a resource for investigating cancer cell dependencies and prioritizing therapeutic targets. Nucleic Acids Res. 49, D1365–D1372 (2021).
Iorio, F. et al. A Landscape of Pharmacogenomic Interactions in Cancer. Cell 166, 740–754 (2016).
Garcia-Alonso, L. et al. Transcription Factor Activities Enhance Markers of Drug Sensitivity in Cancer. Cancer Res. 78, 769–780 (2018).
Li, H. et al. The landscape of cancer cell line metabolism. Nat. Med. 25, 850–860 (2019).
Picco, G. et al. Functional linkage of gene fusions to cancer cell fitness assessed by pharmacological and CRISPR-Cas9 screening. Nat. Commun. 10, 2198 (2019).
Gonçalves, E. et al. Drug mechanism-of-action discovery through the integration of pharmacological and CRISPR screens. bioRxiv, https://doi.org/10.1101/2020.01.14.905729 (2020).
Meyers, R. M. et al. Computational correction of copy number effect improves specificity of CRISPR-Cas9 essentiality screens in cancer cells. Nat. Genet. 49, 1779–1784 (2017).
Zampieri, G., Vijayakumar, S., Yaneske, E. & Angione, C. Machine and deep learning meet genome-scale metabolic modeling. PLoS Comput. Biol. 15, e1007084 (2019).
Allesøe, R. L. et al. Discovery of drug-omics associations in type 2 diabetes with generative deep-learning models. Nat. Biotechnol. 41, 399–408 (2023).
Lotfollahi, M., Wolf, F. A. & Theis, F. J. scGen predicts single-cell perturbation responses. Nat. Methods 16, 715–721 (2019).
Dempster, J. M., Krill-Burger, J., Warren, A. & McFarland, J. Gene expression has more power for predicting in vitro cancer cell vulnerabilities than genomics. bioRxiv, https://doi.org/10.1101/2020.02.21.959627 (2020).
Rohart, F., Gautier, B., Singh, A. & Lê Cao, K.-A. mixOmics: An R package for’omics feature selection and multiple data integration. PLoS Comput. Biol. 13, e1005752 (2017).
Singh, A. et al. DIABLO: an integrative approach for identifying key molecular drivers from multi-omics assays. Bioinformatics 35, 3055–3062 (2019).
Poulos, R. C. et al. Strategies to enable large-scale proteomics for reproducible research. Nat. Commun. 11, 3793 (2020).
Nusinow, D. P. et al. Quantitative Proteomics of the Cancer Cell Line Encyclopedia. Cell 180, 387–402.e16 (2020).
Gonçalves, E. et al. Widespread Post-transcriptional Attenuation of Genomic Copy-Number Variation in Cancer. Cell Syst. 5, 386–398.e4 (2017).
Wainberg, M. et al. A genome-wide atlas of co-essential modules assigns function to uncharacterized genes. Nat. Genet. 53, 638–649 (2021).
Seashore-Ludlow, B. et al. Harnessing Connectivity in a Large-Scale Small-Molecule Sensitivity Dataset. Cancer Discov. 5, 1210–1223 (2015).
Rees, M. G. et al. Correlating chemical sensitivity and basal gene expression reveals mechanism of action. Nat. Chem. Biol. 12, 109–116 (2016).
Mo, Q. et al. Pattern discovery and cancer gene identification in integrated cancer genomic data. Proc. Natl Acad. Sci. USA 110, 4245–4250 (2013).
Du, J.-H., Cai, Z. & Roeder, K. Robust probabilistic modeling for single-cell multimodal mosaic integration and imputation via scVAEIT. Proc. Natl Acad. Sci. USA 119, e2214414119 (2022).
Meng, C., Helm, D., Frejno, M. & Kuster, B. MoCluster: Identifying joint patterns across multiple omics data sets. J. Proteome Res. 15, 755–765 (2016).
Menden, M. P. et al. Machine learning prediction of cancer cell sensitivity to drugs based on genomic and chemical properties. PLoS One 8, e61318 (2013).
Shorthouse, D., Bradley, J., Critchlow, S. E., Bendtsen, C. & Hall, B. A. Heterogeneity of the cancer cell line metabolic landscape. Mol. Syst. Biol. 18, e11006 (2022).
Oren, Y. et al. Cycling cancer persister cells arise from lineages with distinct programs. Nature 596, 576–582 (2021).
Campit, S. E. et al. An Ensemble Metabolome-Epigenome Interaction Network Identifies Metabolite Modulators of Epigenetic Drugs. bioRxiv, https://doi.org/10.1101/2023.02.27.530260 (2024).
Liu, X.-R. et al. UNC0638, a G9a inhibitor, suppresses epithelial‑mesenchymal transition‑mediated cellular migration and invasion in triple negative breast cancer. Mol. Med. Rep. 17, 2239–2244 (2018).
Du, L., Xie, F., Han, H. & Zhang, L. Targeting SALL4 by Entinostat Inhibits the Malignant Phenotype of Gastric Cancer Cells by Reducing EMT Signaling. Anticancer Res. 43, 4389–4401 (2023).
Park, S. J. et al. BIX02189 inhibits TGF-β1-induced lung cancer cell metastasis by directly targeting TGF-β type I receptor. Cancer Lett. 381, 314–322 (2016).
Ojima, T., Kawami, M., Yumoto, R. & Takano, M. Differential mechanisms underlying methotrexate-induced cell death and epithelial-mesenchymal transition in A549 cells. Toxicol. Res. 37, 293–300 (2021).
Meng, Q. et al. Abrogation of glutathione peroxidase−1 drives EMT and chemoresistance in pancreatic cancer by activating ROS-mediated Akt/GSK3β/Snail signaling. Oncogene 37, 5843–5857 (2018).
Pan, L.-N., Ma, Y.-F., Li, Z., Hu, J.-A. & Xu, Z.-H. KRAS G12V mutation upregulates PD-L1 expression via TGF-β/EMT signaling pathway in human non-small-cell lung cancer. Cell Biol. Int. 45, 795–803 (2021).
Zhang, Y. et al. Genome-wide CRISPR screen identifies PRC2 and KMT2D-COMPASS as regulators of distinct EMT trajectories that contribute differentially to metastasis. Nat. Cell Biol. 24, 554–564 (2022).
Hao, X. et al. MixGen: A New Multi-Modal Data Augmentation. arXiv https://doi.org/10.48550/arXiv.2206.08358 (2022).
Liu, Z. et al. Learning multimodal data augmentation in feature space. arXiv, https://doi.org/10.48550/arXiv.2212.14453 (2022).
Pereira, R. C., Santos, M. S., Rodrigues, P. P. & Abreu, P. H. Reviewing Autoencoders for Missing Data Imputation: Technical Trends, Applications and Outcomes. JAIR 69, 1255–1285 (2020).
Ipsen, N. B., Mattei, P.-A. & Frellsen, J. not-MIWAE: Deep Generative Modelling with Missing not at Random Data. arXiv, https://doi.org/10.48550/arXiv.2006.12871 (2020).
Chen, J., Xu, Y., Wang, P. & Yang, Y. Deep Generative Imputation Model for Missing Not At Random Data. In Proceedings of the 32nd ACM International Conference on Information and Knowledge Management 316–325 (Association for Computing Machinery, New York, NY, USA, 2023). https://doi.org/10.1145/3583780.3614835.
Marques-Silva, J. & Huang, X. Explainability is NOT a Game. arXiv, https://doi.org/10.48550/arXiv.2307.07514 (2023).
Ghandi, M. et al. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature 569, 503–508 (2019).
Pacini, C. et al. Integrated cross-study datasets of genetic dependencies in cancer. Nat. Commun. 12, 1661 (2021).
Dempster, J. M. et al. Agreement between two large pan-cancer CRISPR-Cas9 gene dependency data sets. Nat. Commun. 10, 5817 (2019).
Yang, W. et al. Genomics of Drug Sensitivity in Cancer (GDSC): a resource for therapeutic biomarker discovery in cancer cells. Nucleic Acids Res. 41, D955–D961 (2013).
Paszke, A. et al. Pytorch: An imperative style, high-performance deep learning library. Adv. Neural Inf. Process. Syst. 32, 8026–8037 (2019).
Sundararajan, M., Taly, A. & Yan, Q. Axiomatic Attribution for Deep Networks. In Proceedings of the 34th International Conference on Machine Learning (eds. Precup, D. & Teh, Y. W.) vol. 70 3319–3328 (PMLR, 2017).
Smilkov, D., Thorat, N., Kim, B., Viégas, F. & Wattenberg, M. SmoothGrad: removing noise by adding noise. arXiv, https://doi.org/10.48550/arXiv.1706.03825 (2017).
Asperti, A. & Trentin, M. Balancing Reconstruction Error and Kullback-Leibler Divergence in Variational Autoencoders. IEEE Access 8, 199440–199448 (2020).
Kingma, D. P. & Welling, M. Auto-Encoding Variational Bayes. arXiv, https://doi.org/10.48550/arXiv.1312.6114 (2013).
Kingma, D. P. & Welling, M. An Introduction to Variational Autoencoders. arXiv, https://doi.org/10.48550/arXiv.1906.02691 (2019).
Akiba, T., Sano, S., Yanase, T., Ohta, T. & Koyama, M. Optuna: A Next-generation Hyperparameter Optimization Framework. In Proceedings of the 25th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining 2623–2631 (Association for Computing Machinery, 2019). https://doi.org/10.1145/3292500.3330701.
Mo, Q. et al. A fully Bayesian latent variable model for integrative clustering analysis of multi-type omics data. Biostatistics 19, 71–86 (2018).
Ruepp, A. et al. CORUM: the comprehensive resource of mammalian protein complexes. Nucleic Acids Res. 36, D646–D650 (2008).
Chatr-Aryamontri, A. et al. The BioGRID interaction database: 2015 update. Nucleic Acids Res. 43, D470–D478 (2015).
Szklarczyk, D. et al. The STRING database in 2017: quality-controlled protein-protein association networks, made broadly accessible. Nucleic Acids Res. 45, D362–D368 (2017).
Iorio, F. et al. Unsupervised correction of gene-independent cell responses to CRISPR-Cas9 targeting. BMC Genomics 19, 604 (2018).
Acknowledgements
We thank the Broad Institute and the Wellcome Sanger Institute for, through the Cancer Dependency Map consortium, making their data freely available and readily accessible to the scientific community and thereby enabling this work. This research was funded in part by the Wellcome Trust Grant 206194. ProCan® is supported by the Australian Cancer Research Foundation, Cancer Institute New South Wales (NSW) (2017/TPG001,REG171150), NSW Ministry of Health (CMP-01), The University of Sydney, Cancer Council NSW (IG 18-01), Ian Potter Foundation, the Medical Research Futures Fund (MRFF-PD), National Health and Medical Research Council (NHMRC) of Australia European Union grant (GNT1170739, a companion grant to support the European Commission’s Horizon 2020 Program, H2020-SC1-DTH-2018-1,’iPC- individualized Paediatric Cure’ [ref. 826121]), and National Breast Cancer Foundation (IIRS-18-164). Work at ProCan® is done under the auspices of a Memorandum of Understanding between Children’s Medical Research Institute and the U.S. National Cancer Institute’s International Cancer Proteogenome Consortium (ICPC), that encourages cooperation among institutions and nations in proteogenomic cancer research in which datasets are made available to the public. Z.C. is the recipient of a PhD Scholarship from Sydney Cancer Partners with funding from Cancer Institute NSW (2021/CBG0002). A.R.B. is funded by the Portuguese national agency Fundação para a Ciência e a Tecnologia (FCT) through the research grant UI/BD/154599/2022. This work has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement no. 951970 (OLISSIPO project). For open access, the authors have applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. This work was supported by national funds through FCT, under project UIDB/50021/2020 (https://doi.org/10.54499/UIDB/50021/2020). The authors acknowledge the OSCARS project, funded by the European Commission’s Horizon Europe Research and Innovation Programme under grant agreement No. 101129751.
Author information
Authors and Affiliations
Contributions
Z.C., S.A., A.R.B., M.D.S., C.P. and E.G. implemented analyses. Z.C., S.A. and E.G. wrote the software. E.G. supervised and conceptualized the study. S.V., P.J.R., R.R.R., M.J.G, Q.Z. and E.G. acquired funding and contributed to methodology. Z.C, S.A., A.R.B., Q.Z. and E.G. wrote the manuscript. All authors have revised and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
AstraZeneca, GlaxoSmithKline, and Astex Pharmaceuticals have awarded M.J.G. research grants and M.J.G. is founder and advisor at Mosaic Therapeutics. All other authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Yejin Kim, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cai, Z., Apolinário, S., Baião, A.R. et al. Synthetic augmentation of cancer cell line multi-omic datasets using unsupervised deep learning. Nat Commun 15, 10390 (2024). https://doi.org/10.1038/s41467-024-54771-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-024-54771-4
This article is cited by
-
Synthetic lethality in cancer drug discovery: challenges and opportunities
Nature Reviews Drug Discovery (2026)
-
Integrative single-cell and spatial transcriptomics with explainable AI reveal lethal prognostic axis in prostate cancer
npj Digital Medicine (2026)
-
Applications of artificial intelligence in non–small cell lung cancer: from precision diagnosis to personalized prognosis and therapy
Journal of Translational Medicine (2025)
-
Drug resistance in cancer: molecular mechanisms and emerging treatment strategies
Molecular Biomedicine (2025)
-
The clinical application of artificial intelligence in cancer precision treatment
Journal of Translational Medicine (2025)