Abstract
The level of thyroidectomy-related regret in patients with clinically low-risk papillary thyroid microcarcinoma (PTMC) and the determinants of decision regret are largely unknown. Here, we show that 319 (24.2%) of those who undergo thyroidectomy and 4 (3.4%) who undergo active surveillance (AS) express heightened regret based on validated decision regret scale (DRS) scores in the first online survey (P < 0.001). Multivariable analysis and the second online survey for patients with heightened regret confirm that postoperative lower thyroid cancer-specific quality of life (QoL) (scar and psychology) (75.5%) is the most common factor for heightened regret of thyroidectomy, followed by preoperative understanding of disease [not at all] (15.0%), presentation of complications (3.8%) and other factors (5.7%). These results highlight that more caution should be exercised when low-risk PTMC patients are scheduled for thyroidectomy. Information about the various treatments for clinically low-risk PTMC, the risk of thyroidectomy and postoperative QoL should be fully communicated during initial counseling.
Similar content being viewed by others
Introduction
The global incidence of thyroid cancer has increased significantly in recent decades, driven largely by the detection of papillary thyroid cancer (PTC), particularly papillary thyroid microcarcinoma (PTMC), which is defined as a PTC with a tumor size ≤10 mm1. The recommended treatments for PTMC include thyroidectomy2, radiofrequency ablation3, and active surveillance (AS)4 for selected patients. Recent studies4,5,6 have increasingly shown that patients with PTMC do not benefit from thyroidectomy and impaired physical or psychological status is observed postoperatively, especially for low-risk patients with PTMC. However, how patients with clinically low-risk PTMC are associated with the development of thyroidectomy-related regret is largely unknown.
Treatment-related regret, which is defined as remorse or distress following a treatment decision in healthcare, captures the effects of treatment-related functional impairments; oncologic anxiety and outcomes; and behavioral, emotional, and interpersonal changes within the context of patient values and expectations7. The level of treatment-related regret can be measured by the most widely validated decisional regret scale (DRS), which is the only instrument developed and tested to specifically measure experienced (and not anticipated) decision regret in healthcare settings8,9,10. Surgical resection is a more traumatic means of treatment, and surgery-related regret has received more attention. Previous studies have investigated surgery-related regret among localized prostate cancer7,11 and breast cancer patients12. Like the above cancers, PTMC is also known as an indolent cancer with controversial treatment, particularly thyroidectomy for low-risk PTMC1,5.
To understand this issue, the severity of thyroidectomy-related regret experienced by clinically low-risk PTMC patients was evaluated via a multicenter two-step online survey. In addition to the DRS, the first online survey included the validated thyroid cancer-specific quality of life (QoL) scale, which aims to evaluate thyroid-specific symptoms as well as QoL postoperation13,14. These two scales, which are highly reliable in the general population9,13,15,16, were applied to explore the level of thyroidectomy-related decision regret and determine the predictors of heightened regret in clinically low-risk PTMC patients. The second online survey comprising the above-identified predictors was subsequently conducted with patients with thyroidectomy-related heightened regret to specify what patients regret about their choice.
Here, we show that 319 (24.2%) of those who undergo thyroidectomy and 4 (3.4%) who undergo AS express heightened regret and thyroidectomy-related heightened regret is primarily due to lower postoperative QOL.
Results
Clinical characteristics
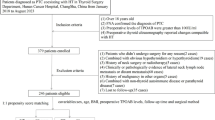
The inclusion process of the study population in our study is detailed in the Methods section and Fig. 1. Among 1805 eligible low-risk PTMC patients enrolled in the first questionnaire survey, 1432 patients completed the questionnaires (response rate: 79.3%). Among these responders, 1316 (91.9%) patients underwent thyroidectomy, and 116 (8.1%) patients underwent AS (Fig. 1). There were 1132 (86.0%) patients who received thyroid hormone replacement/suppression therapy postoperatively in the thyroidectomy group, including 438 (100%) patients who underwent total thyroidectomy and 694 (79.0%) patients who underwent lobectomy. In the AS group, 21 (18.1%) patients with high thyroid stimulating hormone (TSH) levels (higher than the normal upper limit) received thyroid hormone replacement/suppression therapy, as several studies17,18,19 revealed that thyroid hormone replacement/suppression therapy was associated with decreased tumor growth during AS of PTMC. Additionally, of the 1316 responders in the thyroidectomy group, postoperative pathological reports revealed that 85 (6.5%) patients presented with gross or microscopic extrathyroidal extension, and 399 (30.3%) patients presented with lymph node metastasis. The comparison indicated that characteristics were nearly balanced between responders and nonresponders in both the thyroidectomy group and the AS group. Additionally, in comparison with the responders in the AS group, although the responders in the thyroidectomy group tended to be older and have a larger tumor size, similar progression-free survival rates were observed between the two groups. The clinical characteristics of the study population are detailed in Table 1 and Supplementary Fig. 1.
Experiences in preoperative decision-making
As shown in Table 1, responder patients in the thyroidectomy group preferred making the final treatment decision together with their physician (708 [53.8%]), with 405 (30.8%) leaving the decision primary up to their physician and 188 (14.3%) patients making the decision themselves after their physician explained the advantages and disadvantages of treatment options. Notably, decision-making made by someone else was observed in 15 (1.1%) patients. With respect to knowledge about the disease preoperatively in the thyroidectomy group, more than half of the patients had a high degree of knowledge about the disease, including “quite a bit” (501 [38.1%]) and “very much” (346 [26.3%]). The remaining patients included “a little” (249 [18.9%]) and “not at all” (220 [16.7%]). Overall, 1262 (95.9%) patients in the thyroidectomy group reported high-quality communication with physicians. Additionally, the decision-making experiences of the AS group are presented in Table 1. Taken together, there were no significant differences in the experience of preoperative decision-making between the thyroidectomy group and the AS group (P > 0.05 across all categories, Table 1).
Distribution of DRS scores and thyroid cancer-specific QoL after surgery
The patients’ response options for postoperative DRS are detailed in Table 2. In the thyroidectomy group, the median score was 20.0, and the range was 0.0–95.0, which was significantly greater than that in the AS group (median: 7.5, range: 0.0–55.0). Among those patients, 319 patients (24.2%) who underwent thyroidectomy and 4 patients (3.4%) who underwent AS met the definition of heightened decision regret (Fig. 2A, B). The remaining patients either experienced no regret or mild regret (997 [75.8%] in the thyroidectomy group and 112 [96.6%] in the AS group). In addition, we observed that the incidence of heightened regret decreased with increasing follow-up time in the thyroidectomy group (Fig. 2C). For patients who underwent lobectomy or total thyroidectomy, there were no significant differences in terms of DRS scores (Supplementary Table 6). Four patients with heightened decision regret transitioned from AS to surgery in subsequent therapy. The DRS scores of these patients were significantly higher than those of patients who continued with AS (median: 40.0, range: 30.0–55.0 vs median: 5.0, range: 0.0–25.0, P < 0.001).
A, B Histogram of decisional regret scores in the thyroidectomy and AS groups. C The incidence of heightened regret in low-risk PTMC patients undergoing thyroidectomy or AS decreases with increasing follow-up time. D Self-reported reasons for heightened decision regret in the thyroidectomy group. AS Active surveillance, Qol quality of life.
Thyroid cancer-specific QoL scores are presented in Supplementary Table 7. The scores related to the “neuromuscular”, “concentration”, “psychological”, “sensory”, “scarring” and “tingling” scales were significantly higher in the thyroidectomy group than in the AS group (P < 0.05 across all categories). Additionally, the univariable and multivariable analyses of all patients revealed that treatment was positively associated with heightened regret (odds ratio (OR), 1.531; 95% confidence interval (CI), 1.019–2.298; Supplementary Table 8). These results highlight a greater level of regret and impaired QoL in the thyroidectomy group.
Factors associated with heightened decision regret in the thyroidectomy group
The predictors of thyroidectomy-related heightened regret were further explored. Preoperative decision-making experiences (understanding of disease [not at all]), presentation of complications and postoperative lower thyroid cancer-specific QoL (scarring and psychology) were positively associated with heightened regret, with preoperative understanding of disease [not at all] (OR, 4.216; 95% CI, 2.357–9.996), presentation of complications (OR, 3.116; 95% CI, 1.531–10.782), scarring (OR, 2.907; 95% CI, 1.527–3.920) and psychology (OR, 1.835; 95% CI, 1.248–2.988). In contrast, patients who received preoperative high-quality communication (OR, 0.451; 95% CI, 0.232–0.917) or who presented with postoperative lymph node metastasis (OR, 0.347; 95% CI, 0.104–0.864) were less likely to experience regret (Table 3). To directly verify those risk factors, the second questionnaire survey (a questionnaire that includes the above-identified risk factors) was subsequently conducted on patients with heightened regret. Patient-reported data revealed that postoperative lower thyroid cancer-specific QoL (scarring and psychology) (75.5%) was the most common factor for heightened regret, followed by preoperative understanding of disease [not at all] (15.0%), the presence of complications (3.8%) and other factors, including premature operation (2.8%), postoperative immunity decline (1.9%), and hair loss (1.0%) (Fig. 2D).
Discussion
This study highlights the prevalence and risk factors for thyroidectomy-related regret among patients with clinically low-risk PTMC. Several strengths could be observed in our study. First, to our knowledge, few studies have examined the association between thyroidectomy and decision regret in these patients. Although the proportion of low-risk PTMC patients who underwent thyroidectomy has gradually declined in recent years, the multicenter design facilitates the inclusion of a relatively large number of eligible patients for a valid comparison. We believe the results are more reliable because they are less likely to be skewed by a single institution. Second, compared with other studies20,21, the higher response rate of 79.3% and the similar basic characteristics between responder and nonresponder patients minimized the nonresponse bias as much as possible in the first questionnaire. Third, we analyzed a relatively wide range of heightened regret factors, including clinical characteristics, preoperative decision-making experiences, and postoperative thyroid cancer-specific QoL, which is likely to have reduced information bias. Finally, we conducted a targeted secondary questionnaire for low-risk PTMC patients with heightened regret in the thyroidectomy group after identifying the potential elements in the multivariable analysis, which allowed us to investigate the risk factors for heightened regret more specifically.
In this study, decisional regret may not be an experience of a minority of low-risk PTMC patients undergoing thyroidectomy in comparison with other cancer populations with relatively good prognoses7,22,23. The rate of regret for thyroidectomy in this cohort was 24.2%. Among patients with localized prostate cancer, 16.0% of patients who underwent surgery expressed surgery-related regret7. A systematic review analyzed regret in the surgical decision-making of patients and reported that the average prevalence of participants experiencing greater regret was only 14.4%24. These findings suggest that thyroidectomy for low-risk PTMC patients should be more cautious than that for patients with other malignancies. Notably, 236 patients (17.9%) had a regret score of 25 in the thyroidectomy group, suggesting that many potentially heightened regret cases might exist. If this set of patients is added, the rate of heightened regret can reach 41.2%. Additionally, thyroidectomy-related regret was more pronounced in the early stage, and the rate of regret decreased with increasing follow-up time, which may be related to patients adapting to scarring and psychological effects after thyroidectomy. Unlike our study in which a higher DRS score was identified in the thyroidectomy group, a similar mean DRS score was found in patients who underwent thyroidectomy or AS for small (<2 cm) low-risk PTC after 1 year in a recent study16. The advantages of their study include that it is a prospective study and the time for regret assessment is consistent. The strengths of our study include that it is a multicenter study with a larger sample size, as mentioned above. However, importantly, the emergence of this study revealed that thyroidectomy-related decision regret is beginning to receive attention from some clinicians. With respect to patients in the AS group, the rate of regret (3.4%) was lower than that in localized prostate cancer patients with AS7. Among the four patients with heightened regret, three patients presented primary lesion enlargement (20% increase in at least two nodule dimensions with a minimal increase of 2 mm) during follow-up, and one patient regretted due to worry and anxiety about disease progression. Additionally, previous studies25,26 investigated surgical and clinical outcomes in patients with low-risk PTMC between thyroidectomy and delayed thyroidectomy following AS and revealed that there were no differences in the incidence of unfavorable events between the two groups. This evidence suggests that AS followed by surgery for low-risk PTMC patients, even if the disease progresses, will not have a significant adverse impact on their prognosis, as discovered in our study: patients with AS subsequently transitioned from AS to surgery and eventually met the patient’s therapeutic expectations.
Among the factors associated with heightened regret in the thyroidectomy group, the importance of initial counseling was highlighted. Preoperative decision-making is limited to multiple lines. First, patients often make decisions with incomplete knowledge about treatment adverse effects (especially late effects) and prognosis, such as “a little” (249 [18.9%]) and “not at all” (220 [16.7%]) for understanding the disease in our study. Second, not all patients were involved in decision-making, with 31.9% of patients not involved in decision-making in this study. Holmes et al. 27 reported that a full discussion of all treatment options and their involvement in decision-making, whether in the outpatient ward or in the ward, may have the power to mitigate the risk of decision regret. Additionally, shared decision-making is a model that is worthy of attention28. It is a process by which physicians communicate with patients (or other decision-makers) that involves interaction and open communication to explore and contextualize treatment choices to maximize patient autonomy28. In the United States, general surgical planning involves shared decision-making, which is slightly different from management in the study population that we followed. This inconsistency may be related to cultural differences. As described in a previous study29, cultural differences are important factors that can influence the attitudes of Chinese and Westerners toward the general public and healthcare. Third, cancer treatment decision-making comes at a highly emotional time because patients are just absorbing the news of the diagnosis. Highly emotional encounters result in incomplete understanding and absorption of news. Our previous study revealed significant changes in psychological distress during the screening, diagnosis, and treatment of thyroid nodules30,31,32,33. Finally, clinicians’ knowledge regarding low-risk PTMC treatment may also be insufficient in the past1,5,34. Recent studies4,5,6 have increasingly supported the use of AS for low-risk PTMC patients, which may gradually update the perceptions of clinicians.
Patients with cancer tend to overestimate the potential benefits of surgery, often believing that surgery is very likely to cure them35,36. Lobectomy is the most common approach for patients with low-risk PTMC, and 33.4% of patients with low-risk PTMC who underwent total thyroidectomy in our study was mainly due to the presence of nodules in the contralateral thyroid gland or patients’ preference. The extent of surgery was not associated with heightened regret, but our study directly linked postoperative complications with heightened regret. Low-risk PTMC generally does not progress in the short term. However, the complications of thyroidectomy, such as recurrent laryngeal nerve injury and hypoparathyroidism, can result in changes in voice and numbness in the hands and feet. The occurrence of these complications significantly affects the QoL of patients after thyroidectomy. To attenuate complication-related regret, Cohan et al.37 indicated that the patient should be actively engaged and fully informed about complications, and a treatment decision should be made that can reflect patient values and preferences. In addition, obvious scarring after thyroidectomy may negatively affect the QoL of patients with PTMC38,39,40. As most patients with PTMC are young and the prognosis of the disease is good, a considerable number of female patients worry about the formation of a noticeable scar on the anterior neck. Problems with a noticeable scar include difficulty in choosing clothes, fear of communication with others, becoming inferior, and even affecting career development. Endoscopic surgery41 is an alternative treatment for low-risk PTMC that can effectively prevent obvious scar formation, but it is not widely used at present. Additionally, radiofrequency ablation3 has gained increasing interest as a minimally invasive procedure to treat low-risk PTMC and the long-term (58.5 months) outcomes have been verified. With the extensive application of these technologies, we believe that the impact of scarring will be significantly alleviated in the future. Additionally, according to the 2015 ATA guidelines41, the suppression of TSH is commonly used to treat patients with differentiated thyroid cancer in an effort to decrease the risk of recurrence. Hence, patients who undergo total thyroidectomy need to be orally administered the synthetic hormone L-T4, and patients who undergo lobectomy will also proceed with replacement/suppression therapy on the basis of patients’ preferences after we fully communicate with patients regarding the benefits and disadvantages. Additionally, if patients with high TSH levels (higher than the normal upper limit) or low FT4 levels (lower than the normal lower limit) during follow-up for patients undergoing lobectomy, thyroid hormone replacement is recommended. The dosage of the drug can directly affect hormone levels in the body and adversely affect psychological-related indicators42. Although similar thyroid hormone levels were observed in our study in different groups, these levels can fluctuate over time, and the potential role of thyroid hormone therapy in contributing to the DRS and QoL questionnaire could be further evaluated via a long-term multiple monitoring study.
This study also has several limitations. First, this is a domestic multicenter study in China, and the evidence from a global multicenter study is needed to further support our findings. Furthermore, importantly, survey studies may be subject to nonresponse bias. However, our response rate was 79.3% higher than that of other studies20,21, and the characteristics were nearly balanced between responders and nonresponders in our study. Additionally, recency bias, recall bias, and inconsistency in scale assessment times exist in this retrospective study. Finally, scarring is an essential factor of heightened regret. As those technologies to prevent scarring become more widely available, such as endoscopic surgery and radiofrequency ablation, whether they could improve regret remains to be further studied.
In summary, more caution should be exercised when low-risk PTMC patients are scheduled for thyroidectomy. To achieve good communication quality and reduce the risk of surgery regret, the various treatments for low-risk PTMC, the risk of treatment and the postoperative QoL should be fully communicated during initial counseling.
Methods
Cohort and study population
This multicenter online survey cohort study enrolled clinically low-risk PTMC patients who underwent thyroidectomy or AS (diagnosed with PTMC postbiopsy but not subjected to thyroidectomy) at four tertiary hospitals between June 2016 and June 2021 (n = 2441), including the West China Hospital of Sichuan University (Sichuan, China), Meishan City People’s Hospital (Sichuan, China), Sanya People’s Hospital (Hainan, China) and Chongqing University Three Gorges Hospital (Chongqing, China). The patients in the AS group underwent physical examinations, thyroid function tests, and high-resolution ultrasound examinations every 6–12 months43. Clinically low-risk PTMC is defined as PTMC with a lack of definite evidence of extrathyroidal extension, lymph node metastasis, and distant metastasis preoperatively, which is measured mainly by preoperative imaging examinations, including high-resolution ultrasound and computed tomography22,44. Individuals without complete basic information (n = 345), who suffered from uncontrolled chronic disease (n = 133), who had other tumors (n = 78), who had mental disorders (n = 48), and who could not complete the questionnaires independently or with the assistance of others (n = 32) were excluded. Among the 1805 eligible patients, 1668 underwent thyroidectomy, and 137 underwent AS. Ultimately, 1432 (79.3%) patients effectively completed the survey and were enrolled in the final analysis, including 1316 patients who underwent thyroidectomy and 116 patients who underwent AS. In addition, the second questionnaire survey (a questionnaire that includes identified risk factors in our study) was conducted on patients with heightened decision regret. The study design and inclusion/exclusion process are depicted in Fig. 1. This study was approved by the West China Hospital of Institutional Ethics Review Board (Number: 2022 (423)) and followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. The informed consent to participate was obtained by all participants and participant compensation was not implemented in this study.
Data collection
DRS score
Thyroidectomy-related regret, which was measured via the validated Chinese version of the DRS45,46 (Supplementary Tables 1, 3 and 5), was the primary outcome of this study. This series of five questions assesses the extent to which patients regret healthcare, which is scored on a scale of 1 to 5: a score of 1 indicates the least regret and a score of 5 indicates the most regret. The total score can be translated into a score ranging from 0 to 100 via a decrease of 1 point and multiplied by 25, with 100 representing maximal regret. According to the scores, the low-risk PTMC patients were categorized into two groups as previously specified: those with heightened regret (score > 25) and those with no or mild regret (score ≤ 25)47.
Additional data sources
To identify the potential factors associated with thyroidectomy-related regret, we hypothesized relationships between heightened regret and the clinical characteristics of patients, preoperative decision-making experiences, and postoperative thyroid cancer-specific QoL on the basis of prior work on cancer-related decisional involvement7,12,47.
Clinical characteristics of the patients. For the examinees enrolled in the study, information on subject age, sex, race, tumor size, marital status, employment status, comorbidities, surgical options, thyroid hormone replacement/suppression therapy, thyroid function indicators postoperation, complications, postoperative pathological features, recurrence/disease progression, and follow-up time was initially obtained. Common chronic comorbidities, including coronary artery disease, hypertension, diabetes mellitus, chronic kidney disease, liver disease, chronic lung disease such as chronic bronchitis or emphysema, and arthritis, were assessed by requesting information related to these comorbidities from the subjects. The number of self-reported comorbidities was categorized as 0, 1, or ≥230.
Preoperative decision-making experiences. To demonstrate the experience of decision-making, the final decision for patients to undergo thyroidectomy will be identified. They were offered the following options (choose one): completely my choice (with or without input from my family or friends), primarily based on my doctor’s recommendation; my doctor and I made the decision together (with or without input from my family or friends); and someone else’s choice (other than me and my doctor). In addition, how much the patient knows about the disease when making decisions preoperatively was evaluated. The response categories were “not at all”, “a little”, “quite a bit” and “very much”. Finally, the communication quality of decision-making experiences was assessed at two levels, high or low, on the basis of the patient’s subjective feelings.
Postoperative thyroid cancer-specific QoL. To assess postoperative thyroid-specific symptoms as well as QoL in low-risk PTMC patients, a Chinese version of the thyroid-specific QoL questionnaire was used48,49,50 (Supplementary Tables 2–5). This is a 24-item questionnaire that includes seven multi-item scales: neuromuscular, voice, concentration, sympathetic, throat/mouth, psychological and sensory symptoms, and six single scales. All the items were scored from 1 to 4 as follows: 1 = “not at all”, 2 = “a little”, 3 = “quite a bit”, and 4 = “very much”. A higher score indicates more complaints caused by that symptom. In our study, the patients were divided into two groups on the basis of the median thyroid cancer-specific QoL score in the multivariable model.
Reliability and validity of the Chinese version of the questionnaires used in our study
Study population
To further validate the Chinese version of the questionnaires used, 500 PTC patients who underwent thyroidectomy at West China Hospital of Sichuan University between June 2020 and December 2020 were first randomly selected via a random number table. Individuals without complete basic information (n = 36), who suffered from an uncontrolled chronic disease (n = 12), who had other tumors (n = 11), who had mental disorders, and who could not complete the questionnaires independently or who were assisted by others (n = 5) were excluded. Ultimately, 436 eligible PTC patients were enrolled in the first questionnaire survey in the validation study.
Study procedures
The questionnaires containing the Chinese versions of the DRS and the thyroid-specific QoL questionnaire were distributed and collected twice, 3 weeks apart9. The second survey was conducted for those who responded to the first survey, which aims to perform a test–retest correlation as a reliability analysis when testing the validity of the scales.
All questionnaires in this study were administered by two trained clinical research coordinators. To facilitate data collection, patients were contacted via telephone, and WeChat was added after patient consent was obtained. The questionnaires were available in electronic format and can be completed by scanning the QR code via WeChat.
Clinical characteristics of patients included in the validation of questionnaires
Among the 436 eligible PTC patients enrolled in the first questionnaire survey, 366 patients completed both the Chinese version of the DRS and the thyroid-specific QoL questionnaire (response rate: 83.9%). The second questionnaire survey, which was for test–retest correlation, was sent to the 366 people who responded to the first survey, and of those, 312 valid responses (85.2%) were received. The comparison indicated that characteristics were nearly balanced between responders and nonresponders in both the first survey and second survey groups. The clinical characteristics of the study population are detailed in Supplementary Table 3.
Reliability of the Chinese versions of the questionnaires used in our study
With respect to internal consistency reliability, Cronbach’s alpha coefficient was 0.912 for the Chinese version of the DRS. The Cronbach’s alpha coefficient for each domain of the Chinese version of the thyroid-specific QoL questionnaire ranged from 0.601 to 0.892. For the test–retest correlation, the correlation between measurement values from the first and second surveys was greater than 0.800 for all domains of the Chinese version of the DRS and the thyroid-specific QoL questionnaire, suggesting a strong correlation between them (Supplementary Table 4). Taken together, these results indicate that the Chinese version of the questionnaires used in our study has good reliability.
Validity of the Chinese version of the questionnaires
To qualitatively assess the content validity of the Chinese version of the DRS and thyroid-specific QoL questionnaire, an expert panel comprising 4 clinicians (one physician/internist, two surgeons, and one psychologist) was invited to rate the items. For the Chinese version of the DRS, the content validity index (CVI) for clarity was 0.987, and the CVI for relevance was also 0.996. For the Chinese version of the thyroid-specific QoL questionnaire, the CVIs for clarity and relevance were 0.952 and 0.964, respectively. These results demonstrated that experts believe that the items of the Chinese version of the questionnaires used in our study can be used to evaluate the decisional regret and postoperative QoL of thyroid cancer patients.
To test construct validity, exploratory factor analysis (EFA) was then performed in this study. The initial eigenvalues evolve as shown in Supplementary Table 5. One common factor was extracted via principal component analysis, and the cumulative contribution rate of variance was 87.217% in the Chinese version of the DRS. For the Chinese version of the thyroid-specific QoL questionnaire, the questions were divided into three factors, and the cumulative contribution rate for the three factors was 63.428%. Taken together, these results demonstrated that the Chinese versions of the DRS and the thyroid-specific QoL questionnaire presented good construct validity.
Taken together, the Chinese versions of the DRS and thyroid-specific QoL questionnaire used in our study have been proven to be reliable and valid.
Statistical analysis
Statistical analysis was performed via SPSS software, version 25.0 (SPSS, Chicago, IL, USA), and GraphPad Prism (version 8.0). Normally distributed quantitative variables are presented as the means ± standard deviations and were compared via Student’s t-test or one-way ANOVA. Nonnormally distributed parameters are expressed as the median, and the two groups were compared via nonparametric Mann–Whitney U tests. Comparisons of categorical variables were performed via the chi-square test or Fisher’s exact test. Univariable and multivariable logistic regression were used to evaluate factors associated with heightened regret. The OR and 95% CI reflect the independent association of each factor with treatment regret. Kaplan–Meier product-limit method was applied to assess survival in the cohorts, and the log-rank test was used to determine significant differences. Statistical significance was assessed at a two-sided level.
Reliability Testing for the Chinese version of the questionnaires. Reliability was validated by internal consistency and test–retest correlation. The test of internal consistency was evaluated via Cronbach’s alpha coefficient, and we determined that a value above 0.7 was adequate. For the test–retest correlation, reappearance was assessed by the correlation between measurement values from the first and second questionnaire surveys.
Validity Testing for the Chinese version of the questionnaires. The content validity and construct validity were used to validate the validity. The content validity (the clarity and relevance of the items) was evaluated by four specialists in this professional field. We calculated the clarity of construction and wording as well as the content relevance via a 4-point ordinal scale of 1 = item is not clear, 2 = item needs major revisions to be clear, 3 = item needs minor revisions to be clear, 4 = item is clear for clarity, and a 4-point ordinal scale of 1 = item is not relevant, 2 = item needs major revisions to be relevant, 3 = item needs minor revisions to be relevant, and 4 = item is relevant for relevance. We summed the items rated as 3 or 4 by the four specialists and divided the sum by the total number of items rated to measure the CVI. For construct validity, EFA (Varimax method) was applied to determine whether the construct idea we are trying to measure can be measured by the Chinese version of the questionnaires.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The authors declare that all relevant data used to conduct the analyses are available within the article. To protect the privacy and confidentiality of patients in this study, the detailed clinical data are not made publicly available in a repository or the supplementary material of the article but can be requested at any time from the corresponding author J.L. (leijianyong@scu.edu.cn). Any requests will be evaluated within a time frame of 4–5 weeks by the corresponding author and Institutional Ethics Review Board to verify whether the request is subject to any intellectual property or confidentiality obligations. The data will be made available for 1 month. Source data are provided with this paper.
References
Chen, D. W., Lang, B. H. H., McLeod, D. S. A., Newbold, K. & Haymart, M. R. Thyroid cancer. Lancet 401, 1531–1544 (2023).
Xu, S. et al. Comparison of lobectomy vs total thyroidectomy for intermediate-risk papillary thyroid carcinoma with lymph node metastasis. JAMA Surg. 158, 73–79 (2023).
Li, X. et al. Long-term outcomes and risk factors of radiofrequency ablation for T1N0M0 papillary thyroid carcinoma. JAMA Surg. 159, 51–58 (2023).
Lee, J. Y. et al. US predictors of papillary thyroid microcarcinoma progression at active surveillance. Radiology 309, e230006 (2023).
Ho, A. S. et al. Expanded parameters in active surveillance for low-risk papillary thyroid carcinoma: a nonrandomized controlled trial. JAMA Oncol. 8, 1588–1596 (2022).
Bach, K. et al. Health-related quality of life in patients with low-risk differentiated thyroid cancer: a systematic review examining the extent of thyroidectomy. Thyroid 34,14–25 (2024).
Wallis, C. J. D. et al. Association of treatment modality, functional outcomes, and baseline characteristics with treatment-related regret among men with localized prostate cancer. JAMA Oncol. 8, 50–59 (2022).
Brehaut, J. C. et al. Validation of a decision regret scale. Med. Decis. Mak. 23, 281–292 (2003).
Tanno, K., Bito, S., Isobe, Y. & Takagi, Y. Validation of a Japanese version of the Decision Regret Scale. J. Nurs. Meas. 24, E44–E54 (2016).
Haun, M. W., Schakowski, A., Preibsch, A., Friederich, H. C. & Hartmann, M. Assessing decision regret in caregivers of deceased German people with cancer—a psychometric validation of the Decision Regret Scale for Caregivers. Health Expect. 22, 1089–1099 (2019).
Jayadevappa, R. et al. Patient-centered preference assessment to improve satisfaction with care among patients with localized prostate cancer: a randomized controlled trial. J. Clin. Oncol. 37, 964–973 (2019).
Parker, P. A. et al. Prospective study of psychosocial outcomes of having contralateral prophylactic mastectomy among women with nonhereditary breast cancer. J. Clin. Oncol. 36, 2630–2638 (2018).
Jeon, M. J. et al. Quality of life in patients with papillary thyroid microcarcinoma managed by active surveillance or lobectomy: a cross-sectional study. Thyroid 29, 956–962 (2019).
Kong, S. H. et al. Longitudinal assessment of quality of life according to treatment options in low-risk papillary thyroid microcarcinoma patients: active surveillance or immediate surgery (interim analysis of MAeSTro). Thyroid 29, 1089–1096 (2019).
Reyes-Hadsall, S. et al. Shared decision-making, therapeutic choice, and decisional regret in patients with alopecia areata. JAMA Dermatol. 158, 1187–1191 (2022).
Sawka, A. M. et al. Decision regret following the choice of surgery or active surveillance for small, low-risk papillary thyroid cancer: a prospective cohort study. Thyroid 34, 626–634 (2024).
Kim, H. I. et al. High serum TSH level is associated with progression of papillary thyroid microcarcinoma during active surveillance. J. Clin. Endocrinol. Metab. 103, 446–451 (2018).
Sugitani, I. et al. Indications and strategy for active surveillance of adult low-risk papillary thyroid microcarcinoma: consensus statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma. Thyroid 31, 183–192 (2021).
Yamamoto, M. et al. Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status. Thyroid 33, 1182–1189 (2023).
Hoffman, R. M. et al. Treatment decision regret among long-term survivors of localized prostate cancer: results from the Prostate Cancer Outcomes study. J. Clin. Oncol. 35, 2306–2314 (2017).
Huang, K. & Mostaghimi, A. Shared decision-making, therapeutic choice and decisional regret in alopecia areata—Where narrative ethics meets the unconscious bias of clinicians—reply. JAMA Dermatol. 159, 462–463 (2023).
Jones, R. A. Decisional Regret Among Men With Prostate Cancer: What is involved? JAMA Oncol. 8, 59–60 (2022).
Diefenbach, M. A. & Mohamed, N. E. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Investig. 25, 449–457 (2007).
Wilson, A., Ronnekleiv-Kelly, S. M. & Pawlik, T. M. Regret in surgical decision making: a systematic review of patient and physician perspectives. World J. Surg. 41, 1454–1465 (2017).
Hwang, H. et al. Surgical outcomes in patients with low-risk papillary thyroid microcarcinoma from MAeSTro study: immediate operation versus delayed operation following active surveillance a multicenter prospective cohort study. Ann. Surg. 278, e1087–e1095 (2023).
Sasaki, T. et al. Comparison of postoperative unfavorable events in patients with low-risk papillary thyroid carcinoma: immediate surgery versus conversion surgery following active surveillance. Thyroid 33, 186–191 (2023).
Holmes, J. A. et al. Quality of care received and patient-reported regret in prostate cancer: analysis of a population-based prospective cohort. Cancer 123, 138–143 (2017).
Salzburg Global, S. Salzburg statement on shared decision making. BMJ 342, d1745 (2011).
Haishan, H., Hongjuan, L., Tieying, Z. & Xuemei, P. Preference of Chinese general public and healthcare providers for a good death. Nurs. Ethics 22, 217–227 (2015).
Li, R. et al. Psychological distress and sleep disturbance throughout thyroid nodule screening, diagnosis, and treatment. J. Clin. Endocrinol. Metab. 106, e4221–e4230 (2021).
Zhang, P. et al. Psychological impacts of thermal ablation and conventional thyroidectomy in BTN patients: a prospective observational study. Endocrine 85, 1310–1318 (2024).
Jiang, Y. et al. Effects of endoscopic lobectomy and conventional lobectomy on psychological and sleep quality in patients with papillary thyroid microcarcinoma—a prospective observational study. Endocrine 87, 667–674 (2024).
Ye, Z. et al. Psychological impacts of lobectomy and total thyroidectomy in PTC measuring 1 to 4 cm with low to intermediate risk of recurrence. Endocrine 86, 682–691 (2024).
Filetti, S. et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30, 1856–1883 (2019).
Binkley, C. E., Reynolds, J. M. & Shuman, A. From the eyeball test to the algorithm—quality of life, disability status, and clinical decision making in surgery. N. Engl. J. Med. 387, 1325–1328 (2022).
Church, J. Quality of life and patient-reported outcomes. Br. J. Surg. 105, 157–158 (2018).
Cohan, J. N. et al. Factors associated with decision regret among patients with diverticulitis in the elective setting. J. Surg. Res. 261, 159–166 (2021).
Kurumety, S. K. et al. Post-thyroidectomy neck appearance and impact on quality of life in thyroid cancer survivors. Surgery 165, 1217–1221 (2019).
Li, T. et al. Comparison of quality of life and cosmetic result between open and transaxillary endoscopic thyroid lobectomy for papillary thyroid microcarcinoma survivors: a single-center prospective cohort study. Cancer Med. 11, 4146–4156 (2022).
Choi, Y. et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients. Ann. Dermatol. 26, 693–699 (2014).
Dong, F., Yang, A. & Ouyang, D. Retroauricular single-site endoscopic thyroidectomy—a balanced endoscopic approach for thyroid excision. JAMA Surg. 158, 548–549 (2023).
Altuntas, S. C. & Hocaoglu, C. Effects of chronic suppression or oversuppression of thyroid-stimulating hormone on psychological symptoms and sleep quality in patients with differentiated thyroid cancer. Horm. Metab. Res. 53, 683–691 (2021).
Oh, H. S. et al. Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid 28, 1587–1594 (2018).
Haugen, B. R. et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26, 1–133 (2016).
Zhang, C. L. et al. Decision regret analysis among Chinese patients receiving penile girth enhancement with acellular dermal matrix. Beijing Da Xue Xue Bao Yi Xue Ban 52, 678–683 (2020).
Zhang Chunlong, L. H. et al. Validation analysis of Chinese version of decision regret scale in patients undergoing penile girth enhancement with acellular dermal matrix. Chin. J. Hum. Sex. 30, 11–14 (2021).
Mack, J. W., Cronin, A. M. & Kang, T. I. Decisional regret among parents of children with cancer. J. Clin. Oncol. 34, 4023–4029 (2016).
Liu, J., Gao, J., Tang, Y., Wu, C. & Yu, J. Reliability and validity of Chinese version of thyroid cancer-specific quality of life (THYCA-QOL) questionnaire. Tumor 39, 178–187 (2019).
Chen, X. L. et al. [A comparative study for the efficacies of transaxillary non-inflatable endoscopic surgery versus traditional surgery for papillary thyroid carcinoma]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 58, 351–357 (2023).
Maneesriwongul, W. & Dixon, J. K. Instrument translation process: a methods review. J. Adv. Nurs. 48, 175–186 (2004).
Author information
Authors and Affiliations
Contributions
Tang, H.R., Li. Z.H., and Lei, J.Y. were responsible for study conception, design, and supervision. Wei, T., Li, Z.H., Shuai, J.H., Chen, M.Z., and Deng, F. provided the clinical cases. Li, G.P., Li, R.C., Zhong, J.J., Chen, W.J., and Lei, J.Y. wrote and revised the manuscript. Li, G.P., Li, R.C., Zhong, J.J., and Chen, W.J. contributed equally to this article and could be co-first authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the West China Hospital of Institutional Ethics Review Board (Number: 2022 (423)).
Consent to participate
The informed consent to participate was obtained by all participants and participant compensation was not implemented in this study.
Peer review
Peer review information
Nature Communications thanks Sriram Gubbi, Joanna Klube-Gwiezdzinska, and Rebecca Williams for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, G., Li, R., Zhong, J. et al. A multicenter cohort study of thyroidectomy-related decision regret in patients with low-risk papillary thyroid microcarcinoma. Nat Commun 16, 2317 (2025). https://doi.org/10.1038/s41467-025-57627-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-57627-7