Abstract
In recent decades, Acinetobacter baumannii has become a major global nosocomial pathogen, with bloodstream infections (BSIs) exhibiting mortality rates exceeding 60% and imposing substantial economic burdens. However, limited large-scale genomic epidemiology has hindered understanding of its population dynamics. Here, we analyzed 1506 non-repetitive BSI-causing A. baumannii isolates from 76 Chinese hospitals over a decade (2011–2021). We identified 149 sequence types (STs) and 101 K-locus types (KLs), revealing increased population diversity. International clone (IC) 2 accounted for 81.74% of isolates, with a notable shift in prevalent STs: ST208 increased while ST191 and ST195 declined, aligning with global trends. ST208 exhibited higher virulence, greater antibiotic resistance, enhanced desiccation tolerance, and more complex transmission patterns compared to ST191 and ST195. Its genomic plasticity drives its adaptation and spread. Using the high-resolution Oxford MLST scheme, this study uncovered greater diversity and genetic factors behind ST208’s rise. A. baumannii is evolving from a low-virulence, multidrug-resistant pathogen to a more virulent one, highlighting the urgent need to address its growing threat. These findings have critical implications for infection control and public health policies.
Similar content being viewed by others
Introduction
Acinetobacter baumannii is an opportunistic human pathogen that predominantly causes healthcare-associated infections, such as ventilator-associated pneumonia and bloodstream infections (BSIs), particularly in critically ill patients1,2,3. Approximately 1,000,000 people worldwide are estimated to be infected with A. baumannii each year1. Infections caused by A. baumannii account for 6–7% of all healthcare-associated infections in China; this figure is twice as high as those reported in the United States and Europe2,4. A. baumannii has been identified as the cause of approximately 1.6% of all healthcare-associated BSIs in the United States, similar to findings in Europe. In China, approximately 2.8% of all healthcare-associated BSIs are caused by A. baumannii2. Despite a low isolation rate, BSIs caused A. baumannii have an alarmingly high mortality rate that exceeds 60%, leading to higher total hospitalisation costs and significantly impacting the clinical and economic burden1,5,6.
A. baumannii is now considered a global healthcare setting threat, mainly due to its propensity to acquire multidrug resistance phenotypes and to thrive in the healthcare environment at previously unforeseen rates7,8. Globally, A. baumannii has a high multidrug resistance (MDR) rate, reaching ~45%9,10,11. Carbapenem-resistant A. baumannii (CRAB) is considered “critical” among the WHO priority pathogens12. In China, CRAB has an isolation rate of ~70% and is susceptible consistently to treatment only with polymyxins and tigecycline3. In addition to antibiotic resistance, its environmental persistence, such as disinfection and desiccation tolerance, biofilm formation, and motility, is another attribute that enables A. baumannii to thrive in the nosocomial environment13,14,15,16,17. Compared with its antibiotic resistance and environmental persistence, little attention is given to its virulence. A. baumannii is often viewed as an environment-originating, low-virulence opportunistic pathogen7. The current understanding of A. baumannii virulence primarily focuses on essential factors such as capsular polysaccharides, secretion systems, and micronutrient acquisition systems, which collectively enable successful host infection7. Recently, more studies have focused on the impact of virulence on the prognosis of A. baumannii infections. However, these studies are relatively fragmented and lack comprehensive, overarching analysis, especially concerning BSIs caused by A. baumannii18,19,20,21.
The genomic plasticity of A. baumannii has led to a wide range of strain variations22,23. These variations contribute to diverse phenotypes associated with pathogenesis and population diversity7,22,23. Significant variation in capsular polysaccharide structures has been identified between A. baumannii isolates, with over 100 distinct capsule types recognised24. Among the A. baumannii genomes available in GenBank, 59% belong to the international clone (IC)225. The dissemination of IC2 has been well documented. Oxford sequence type (ST) 195, ST191 and ST208 are most prevalent lineages of A. baumannii IC2. Within IC2, there is significant variation, encompassing over 500 Oxford STs. All these variations suggest that the epidemiological characteristics and trends of A. baumannii may undergo constantly change18,21,26.
In this study, we investigated the genomic epidemiology of 1506 BSI-causing A. baumannii strains isolated over an 11-year period between 2011 and 2021 across China and collected in the framework of the national surveillance Blood Bacterial Resistant Investigation Collaborative System (BRICS) to elucidate the spatial and temporal population structure of BSI-causing A. baumannii strains and dissect the genetic and phenotypic drivers of intraclonal diversification. We revealed heightened diversity of these isolates and investigated the factors driving the increased prevalence of ST208.
Results
Population structure and spatiotemporal distribution of BSI-causing A. baumannii isolates in China
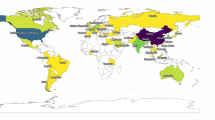
Between 2011 and 2021, a total of 1506 non-repetitive A. baumannii isolates involved in BSIs were collected from 76 sentinel hospitals distributed across 25 provinces covering 83.87% of the population of China (ca. 1.18 billion) (Fig. 1a, Fig. S1a). The genomes were analysed via average nucleotide identity (ANI) and ribosomal multilocus sequence typing (rMLST), which excluded other bacterial species within the Acinetobacter calcoaceticus-Acinetobacter baumannii (Acb) complex. The three provinces with the most strains were Zhejiang Province (ZJ) (40.2%), Anhui Province (AH) (20.0%), and Shandong Province (SD) (7.7%) (Fig. S1a). The collection of strains was limited from 2011 to 2013, with a more even distribution observed from 2014 to 2021 (Fig. S1b). A total of 149 STs were identified via the Oxford scheme, including 47 new STs that we submitted to PubMLST database (ST3225 to ST3271), with the top 3 being ST195 (n = 334), ST208 (n = 234), and ST191 (n = 148) (Figure 1ab, Supplementary Fig. S1c, Supplementary Data 1). Twenty-nine of the 149 identified STs (1,227 strains), including two new STs (ST3243 and ST3247, belonged to the IC2 lineage (1231/1506, 81.74%), which significantly dominates BSI-causing A. baumannii strains nationwide. ST208 was the hub node of IC2 (Fig. S2).
a Clonal distribution of the 1,506 nonrepetitive A. baumannii isolates in 76 sentinel hospitals distributed across 25 provinces from 2011 to 2021. The map shows the prevalence of various STs in different regions, as represented by pie charts located at corresponding geographic locations. Each pie chart illustrates the proportion of specific STs in that region. The number next to each region’s name represents the total number of isolates analysed from that region. b Distribution of the top ten STs of A. baumannii from 2011 to 2021. The bar chart illustrates the yearly prevalence of various STs. The y-axis represents the percentage of each ST. The total number of isolates (n) for each year is indicated below the x-axis. Different colours represent different STs, as indicated in the legend on the right. c The number and proportion of IC2 and non-IC2 strains changed over time. d Increase in the population diversity of IC2 and non-IC2 A. baumannii-related BSI isolates in China between 2011 and 2021. The axes indicate the Shannon diversity index (Y-axis) and the year of isolation (X-axis). Dots represent the shannon diversity index of this type of A. baumannii ST type in this year. The shaded area surrounding the fitted linear regression line represent the 95% confidence interval based on the standard error of the mean slope of the regression line. The ST diversity of IC2 was significantly positively correlated with time (r = 0.4, p = 0.036). Non-IC2 ST diversity also showed a significant positive correlation with time (r = 0.8, p < 0.001), with a higher correlation coefficient than IC2. Source data are provided as a Source Data file.
Capsular genotyping revealed 101 K-locus types (KLs) among the 1,506 isolates, with the top three being KL3 (22.2%), KL2 (11.6%), and KL9 (9.6%), indicating a highly diverse distribution of KL types across BSI-causing A. baumannii isolates in China. In this study, different KLs corresponded to different STs. For example, 81.08% (120/148) of the ST191 strains were KL72, and 18.92% (28/148) were KL9. A total of 99.4% (332/334) of the ST195 strains were KL3. A total of 73.93% (173/234) of the ST208 strains were KL2, and 25.64% (60/234) of the ST208 strains were KL7. The KL9 isolates corresponded mainly to ST369 (97/145, 66.90%) and ST191 (Fig. S3, Supplementary Data 1). The distributions of the KL types did not show significant regional differences, but the frequencies of some KL types varied with time (Fig. S1d). Changes in some KL types over time reflect corresponding changes in STs over time. For example, the decreasing isolation rates of KL3 and KL72 over time mirror the decreasing isolation rates of ST195 and ST191 (Fig. 1b, Fig. S1d). Moreover, we observed a significant volatility increase in KL7 from 1.36% in 2014 to 9.32% in 2021, amid the years in which the isolates were evenly distributed (Fig. S1f), and 90.91% of the KL7 strains were found within the ST208 strains (Supplementary Data 1). Additionally, there were 16 locus types for the lipooligosaccharide outer core biosynthesis locus (OCL), with the top three being OCL1 (83.1%), OCL6 (7.2%), and OCL2 (3.9%). The exclusive OCL type found across the three most prevalent STs was OCL1 (Fig. S3).
The population dynamics and phylogenetic relationships of BSI-causing A. baumannii
A notable shift in the proportion of dominant STs in IC2 occurred during the study period. The proportion of ST195 sharply declined from 42.18% in 2014 to 8.5% in 2021, and that of ST191 declined from 18.37% in 2014 to 0.9% in 2021. Conversely, the proportion of ST208 increased from 12.93% in 2014 to 21.19% in 2021, whereas those of ST540 and ST369 rose from 2.7% and 2.04% in 2014 to 11.44% and 12.3% in 2021, respectively (Fig. 1b). The proportion of unknown STs progressively increased each year, increasing from 2.04% (3/147) in 2014 to 4.66% (11/236) in 2021 (Fig. 1b). The isolation rate of non-IC2 strains has shown a fluctuating increasing trend over time, starting at 13.56% in 2011 and remaining above 22.22% since 2018 (Fig. 1c). The ST diversity of IC2 was significantly positively correlated with time (r = 0.4, p < 0.036). Non-IC2 ST diversity also showed a significant positive correlation with time (r = 0.8, p < 0.001), with a higher correlation coefficient than IC2. Linear regression confirms these findings. The steeper slope for the time association of non-IC2 suggested that its diversity changed more significantly over time (Fig. 1d, Fig. S1e).
To compare the global prevalence trends of BSI-causing A. baumannii to those specific to China, we collected data from the National Center for Biotechnology Information (NCBI) Pathogen Detection database, which comprises a total of 1978 BSI-causing A. baumannii genomes with identified isolation times and locations, including 246 isolates from mainland China (as of September 7, 2023; Supplementary data 2). The temporal span of the data ranged from 1995 to 2023. We annotated and sequenced typing the above isolates and included them in epidemiological analysis. The dataset included a total of 207 STs (Oxford scheme). There were only 30 shared STs between mainland China and other countries/regions, indicating substantial differences in the ST distribution of BSI-causing A. baumannii between mainland China and other regions worldwide. According to the global data, the top three STs were the same as those in China, namely, ST195 (n = 281), ST208 (n = 261), and ST191 (n = 92). The rest of the top 10 STs showed complete divergence between the rest of the world and China (Fig. S4a, b).
After excluding strain data from mainland China, ST191, ST195, and ST208 presented similar trends in isolation rates on a global scale, with an increase in the proportion of ST208 and a decrease in that of ST191 and ST195 compared with the findings in this study (Fig. S4c, d). ST540, which ranked fourth (9.03%, n = 136) among the isolates from this study, was not found in the global BSI-causing A. baumannii genomes except for isolates from China, which suggests that ST540 is associated with local evolution and prevalence in China (Fig. S4b). In addition to ST540, ST1791, ST1968, ST373, and ST381 have been isolated only from mainland China. ST369 ranked fifth (6.64%, n = 100) among the strains isolated in this study, but, excluding those from mainland China, only 1% (18/1732) of the isolated strains globally belonged to ST369.
A maximum-likelihood phylogeny reflecting the relationships among the 1506 BSI-causing A. baumannii isolates was constructed via core-genome MLST (cgMLST) in this study. The analysis revealed the division of these isolates into two distinct clusters on the basis of IC2 and non-IC2. The IC2 strains exhibited relatively close evolutionary distances, whereas the non-IC2 strains were dispersed (Fig. S5).
To achieve greater resolution in analysing the phylogenetic relationships among IC2 strains, a maximum-likelihood tree was derived from recombination-free Single Nucleotide Polymorphisms (SNPs) (Fig. 2). The IC2 strains can be divided into four major lineages: ST191, ST208, ST195, and other STs (Fig. 2). Through further detailed analysis, we determined that ST208 can be divided into three lineages, and lineage L3 can be further subdivided into eleven sub-lineages (Fig. 3). From a temporal perspective, the ST208 cluster was interleaved with isolation times, suggesting that ST208 strains with close evolutionary distances have coexisted over time, implying a survival advantage for ST208. Different KLs of ST208 (ST208-KL2 and ST208-KL7) were cross-distributed on the tree (Figs. 3 and 4), indicating that distinct KLs may have been acquired through recombination. A total of 81.82% (36/44) of L1 isolated in 2016 or earlier, 97.72% (43/44) L1 isolates were KL2. All L2 isolates (n = 22) were isolated in 2017 or later, along with KL7 and KL2. A total of 64.15% (102/159) of the L3 isolates were isolated in 2017 or later, with L3.1 (n = 13), L3.8 (n = 6), L3.10 (n = 4), L3.11 (n = 4) isolates being KL7 and having been isolated in 2018 or later (Fig. 3). These results indicate that ST208-KL7 has evolved into a distinct cluster, which may further expand and gradually replace ST208-KL2 or coexist alongside it.
The phylogenetic tree is rooted according to the A. baumannii XH857 (accession number: NZ_CP014540.1) outgroup. Branch lengths represent the number of nucleotide substitutions per site, as indicated by the scale bar. Branch colours represent the bootstrap support values. Orange or blue dots indicate that the gene exists in the corresponding strain, while blank indicate that it does not exist. Source data are provided as a Source Data file.
We collapsed the branches corresponding to ST191, ST195, and other ST types, and focused on enlarging the internal lineage structure of the ST208 branch. ST208 could be divided into three lineages (L1-L3), with L3 further subdivided into 11 sub-lineages (L3.1-L3.11). ST208 lineages are labelled and are painted with different colours. The tree is surrounded by colour strips, indicating the lineages, KL locus, provinces and year, respectively. Source data are provided as a Source Data file.
Five isolates were randomly selected for each ST-KL combination to conduct experiments (Supplementary table 1). A. baumannii LAC-4, AB5075, and ATCC17978 were used as control strains. The results of the complement killing assay for different ST (a) and ST-KL (b) strains. The assay was triplicated, and the error bars represent standard deviations. Student’s t tests were used for pairwise group comparisons. The anti-complement killing ability of ST208 is greater than that of ST191 or ST195, but not significant (a, p > 0.05), and ST208-KL2 exhibits the strongest anti-complementary killing ability, but also not significant (b, p > 0.05). In vivo mouse infection model showing 72-h survival rates (c) and survival rates every 12 h (d) for different ST-KL combination strains. Five mice were injected with each strain. The error bars represent standard deviations (c). Student’s t-tests were used for pairwise group comparisons (c). The average survival rates of the mice infected with ST208-KL2, ST208-KL7, or ST191-KL9 were significantly lower than those infected with ST191-KL72 or ST195-KL3 (c, p < 0.05). Survival rates of different ST (e) and ST-KL (f) strains under 20% humidity. The assay was triplicated, and the error bars represent standard deviations. Student’s t tests were used for pairwise group comparisons. The desiccation tolerance of ST208 was significantly greater than that of ST191 or ST195 (e, p < 0.05), with ST208-KL2 exhibiting even greater desiccation tolerance (f). Source data are provided as a Source Data file. Notes: * indicates P < 0.05, ** indicates P < 0.01, *** indicates P < 0.001, **** indicates P < 0.0001.
ST208 exhibited increased virulence
To evaluate the potential pathogenesis of ST208 compared with that of ST191 and ST195, which contributes to its prevalence, we focused on capsules. Considering the need to diversify according to region and isolation time, we randomly selected five isolates for each ST-KL combination to conduct experiments (Supplementary Table 1). The results of the antiserum complement killing assay indicate that the complement resistance of ST208 is greater than that of ST191 or ST195. This was mainly reflected in the fact that ST208-KL2 has the strongest anti-complement killing ability but not significant (Fig. 4a, b). Virulence and pathogenicity are multifaceted, and the relative virulence and pathogenicity of strains ultimately need to be evaluated via in vivo models. To further investigate virulence, a mouse model of abdominal infection was employed. The average survival rates of the mice infected with ST208-KL2, ST208-KL7, or ST191-KL9 were significantly lower than those infected with ST191-KL72 or ST195-KL3 (Fig. 4c, d). The average virulence of a strain from each of the three STs was weaker than that of LAC-4 and AB5075, the two classic highly virulent strains of A. baumannii. Although the ST191-KL9 strains accounted for a relatively small proportion of the ST191 strains and exhibited a clonal spread phenomenon in ZJ, the significantly increased virulence of ST191-KL9 in the mouse infection model compared with that of the ST191-KL72 strain highlighted the potential for transmission and infection by ST191-KL9 (Fig. 4c). The survival rates of mice infected with the ST208-KL2 isolates varied, whereas those of the mice infected with the ST208-KL7 isolates remained consistent (Fig. 4c, d). All mice (5 per strain) infected with two ST208-KL2 strains died, whereas for one ST208-KL2 strain, all infected mice survived until after the seventh day of infection. These findings indicate that, in addition to KL type, other factors influenced the virulence of the ST208-KL2 strains. Overall, compared with those of the other two prevalent STs, the ST208 strains presented significantly greater virulence.
Furthermore, the virulence factors of A. baumannii ST208, ST191 and ST195 were analysed using VFDB database. The average number of virulence-related genes in the ST208 isolates was greater than that in the ST191 or ST195 isolates, indicating a larger virulence-related gene repertoire (133.90 ± 4.72 vs 126.44 ± 6.86 vs 131.79 ± 1.61, p < 0.05 according to the Wilcoxon rank-sum test, Fig. 5a), which may partially explain its success. Principal component analysis (PCA) revealed that there are significant differences among the virulence genomes of ST191, ST195, and ST208, the virulence-related gene profile of ST195 showed greater disparity from that of either ST208 or ST191 (R = 0.907, p = 0.001; Fig. 5b). A set of key virulence factors (VFs) associated with hypervirulence and typically located on chromosomes, such as immune modulation-related VFs, contributed to the differences in the virulence of ST208 compared to that of other STs (Fig. 5c, Supplementary Data 1).
a Number of virulence-related genes in ST208 compared with those in ST191 and ST195. The average number of virulence-related genes in the ST208 isolates was greater than that in the ST191 or ST195 isolates (133.90 ± 4.72 vs 126.44 ± 6.86 vs 131.79 ± 1.61, p < 1.6 × 10−11, Wilcoxon rank-sum test). b Principal component analysis (PCA) of virulence-related genes profile in strains ST208, ST195 and ST191. There are significant differences among the virulence genomes of ST191, ST195, and ST208, the virulence-related gene profile of ST195 showed greater disparity from that of either ST208 or ST191 (R = 0.907, p = 0.001, ANOSIM). c Comparison of the number of virulence-related genes in different functional categories in ST208, ST195 and ST191, the results showed significant differences in five virulence-related functions (p < 1 × 10−5, Wilcoxon rank-sum test). For (a, c), boxes show the median and interquartile range (IQR) while whiskers extend to a maximum of 1.5× IQR. Dots indicate outliers beyond whiskers. The statistical significance is shown by the number of asterisks as follows: ****p < 0.0001, NS. indicates no statistical significance. Source data are provided as a Source Data file.
Through correlation analysis, we found that the significant factor influencing the distribution of virulence-related genes in all strains was sequence types (Fig. S6a, adjusted R2 = 0.72, p.adj < 0.001). We clustered virulence-related genes according to STs and discovered that the overall carriage rate of virulence-related genes in non-IC2 strains was not lower than that in IC2 strains. However, the carriage rates of some important virulence-related genes, such as those in the Type VI secretion system (T6SS) cluster (14.06% vs. 65.89%) and the hemO cluster (28.48% vs. 87.12%), were significantly lower in non-IC2 strains than in IC2 strains (Fig. S6b). Different isolation times (year) and provinces (temperature and humidity) also influenced the isolation rates of virulence-related genes (Fig. S6a). The carriage rates of 15 virulence-related genes were significantly correlated with changes over time (Spearman r > | ± 0.80 | , FDR < 0.05). The functions of these virulence-related genes include capsule (n = 14) and type IV pili (n = 1). The occurrence of ten capsule-related genes increased over time, whereas that of 4 capsule-related genes and one type IV pili-related gene decreased over time (Supplementary Data 3). These results were consistent with the changes in KLs over time, indicating that the KLs (capsule-related genes) of A. baumannii are continuously evolving and changing.
Increased desiccation tolerance and the propensity to acquire ARGs drove the thrive of ST208
To evaluate the environmental persistence (which contributes to its ability to survive in the healthcare environment), disinfectant tolerance and desiccation tolerance of ST208 compared with that of ST191 or ST195 were analysed. The distribution analysis of disinfectant tolerance-related genes in the top 3 STs revealed a total of 25 disinfectant tolerance-related genes among them (Fig. S7a). Overall, the average number of disinfectant tolerance-related genes in the ST191 isolates was significantly greater than that in the ST195 or ST208 isolates (Fig. 6a, 24 vs 23 vs 23.79, p < 0.01). Among these, qacE was the most unevenly distributed, with that of ST208 and ST191 both significantly greater than that of ST195 (Kruskal‒Wallis, Dunn’s test for multiple comparisons, p.adj < 0.05) (Fig. S7a). Disinfectant tolerance experiments revealed that the disinfectant tolerance phenotype of ST208 was not significantly different from that of ST191 or ST195 (Fig. S7b). The desiccation tolerance of ST208 was significantly greater than that of ST191 or ST195, with ST208-KL2 exhibiting even greater desiccation tolerance (Fig. 4e, f). This may be because capsules belonging to KL2 strains are hydrophilic, providing an important advantage for survival on abiotic surfaces such as those found in hospital environments27, which could explain the greater desiccation tolerance observed in ST208 than in ST191 or ST195 (Fig. 4e, f).
a The number of disinfectant tolerance-related genes in ST208 (n = 234) compared with those in ST191 (n = 148) and ST195 (n = 334). The average number of disinfectant tolerance-related genes in the ST191 isolates was significantly greater than that in the ST195 or ST208 isolates (24 vs 23 vs 23.79, p < 0.0078, Wilcoxon rank-sum test). b Number of antibiotic resistance-related genes (ARGs) in ST208 compared with those in ST191 and ST195. Compared with ST191 and ST195, ST208 presented significantly more ARGs (31.97 ± 3.23 vs 29.83 ± 1.67 vs 29.40 ± 3.65, p < 2.2 × 10−16, Wilcoxon rank-sum test). For (a, b), boxes show the median and interquartile range (IQR) while whiskers extend to a maximum of 1.5× IQR. Dots indicate outliers beyond whiskers. The statistical significance is shown by the number of asterisks as follows: *p < 0.05, **p < 0.01, ****p < 0.0001. c Heatmap of antimicrobial resistance rates among the main STs to 14 antibiotics (POL polymyxin B, TGC tigecycline, AMK amikacin, CRO ceftriaxone, GEN gentamicin, CIP ciprofloxacin, LVX levofloxacin, CSL cefperazone-Sulbactam, CAZ ceftazidime, IPM imipenem, MEM meropenem, FEP, cefepime, SXT sulfamethoxazole, TZP piperacillin-tazobactam). Source data are provided as a Source Data file.
To understand how resistance profile shapes the population structure of A. baumannii clinical isolates, we analysed their antibiotic-resistance genes (ARGs) and the minimum inhibitory concentrations (MICs) of 14 antibiotics in the isolates. The average number of ARGs in non-IC2 isolates was significantly lower than that in IC2 isolates (19.59\(\,\pm \,\)3.32 vs 30. 8\(1\pm\)3.06, p < 0.001, Fig. S8). The carrying rate of some ARGs in non-IC2 strains, such as blaOXA-23 was 11.64%, which was lower than the 97.64% in IC2 strains (Fig. S8). Among these, 96.93% (1196/1234) blaOXA-23 positive isolates carried blaOXA-23 within a Tn2007 transposon, while the other 38 isolates carried it within Tn2008. We did not detect Tn2006 or Tn2009, which are known to occur in other regions globally. The blaNDM-1-like, blaOXA-24-like, blaOXA-270-like, and blaOXA-58-like genes were detected in 6, 6, 1, and 3 isolates, respectively, across all strains. The carrying rates of some ARGs, such as sul2, blaTEM-1, and tet(B), differed across the different ST-KL combinations (Fig. S9a). 81.80% of the IC2 isolates were CRAB, whereas 60.36% of the non-IC2 isolates were CRAB. The resistance rate of A. baumannii to ceftriaxone (a third-generation cephalosporin) increased significantly with time (Fig. S9b). Compared with ST191 and ST195, ST208 presented significantly more ARGs (31.97 ± 3.23 vs 29.83 ± 1.67 vs 29.40 ± 3.65, p < 2.2 × 10−16, Wilcoxon rank-sum test, Fig. 6b). However, blaOXA-23 carriage rates did not significantly differ among ST208, ST191, and ST195 (95.73%, 97.3%, 99.7%, respectively. Fig. S8). Compared with ST191 and ST195, ST208 had a significantly greater presence of APH(3’)-Ia and other aminoglycoside resistance genes (50% vs 64.37% vs 88.03%, Fig. S8). The imipenem resistance rates for ST208, ST191, and ST195 were 78.21%, 85.14%, and 85.33%, respectively, and there were no significant differences. The drug resistance rates of ST208 to aminoglycosides (amikacin, gentamicin) and quinolones (ciprofloxacin, levofloxacin) were at least 10% higher than those of ST191 or ST195 (Fig. 6c, Fig. S10). In addition to the increase in the rate of ceftriaxone drug resistance annually, the drug resistance rate of ST208 to the other 13 antibacterial drugs showed a stable and fluctuating trend (Fig. S9c). These findings suggest that ST208 harbours more ARGs and has higher resistance rates to commonly used quinolones in China, contributing to its prevalence.
Enhanced genomic plasticity underlain the adaptation of ST208
The previous results indicate that, compared with ST191 and ST195, ST208 is more virulent, has greater desiccation tolerance, and has a greater abundance of ARGs. To determine the underlying reasons behind these characteristics, we conducted a genome-based analysis. No significant changes were detected in the total number of genes or the number of ARGs or VFs in the genomes from 2011 to 2021 (Fig. S11ab). Overall, the number of genes in the ST208 genome and its total genomic length were significantly greater than those of ST191 and ST195 (3920.41 ± 149.48 vs 3834.25 ± 110.21 vs 3788.18 ± 58.49, p < 2.5 × 10−9, Wilcoxon rank-sum test and 4.14 + e06 ± 2.96E + 05 vs 4.06 + e06 ± 1.56E + 05 vs 4.00 + e06 ± 2.96E + 05, p < 4 × 10−7, Wilcoxon rank-sum test), indicating that, compared with ST191 and ST195, ST208 possesses a significantly larger genome (Fig. 7a, b). Recombination and horizontal gene transfer play crucial roles in shaping bacterial genome structures by influencing the exchange of genetic materials, such as mobile genetic elements (MGEs). We conducted an analysis of recombination and MGEs, including integrons, insertion sequences (ISs), prophages, and plasmids (approximated by replicons), in the three predominant STs, in an aim to identify additional mechanisms contributing to the adaptation of these strains.
a Gene number distributions of the ST191, ST195 and ST208 isolates, ST208 presented significantly more gene number (p < 2.5 × 10−9, Wilcoxon rank-sum test). b Genome length distributions of the ST191, ST195 and ST208 isolates, ST208 presented significantly expanded genome (p < 4 × 10−7, Wilcoxon rank-sum test). For (a, b), boxes show the median and interquartile range (IQR) while whiskers extend to a maximum of 1.5× IQR. Dots indicate outliers beyond whiskers. Wilcoxon rank-sum test was used for statistical test between two groups. The statistical significance is shown by the number of asterisks as follows: ****p < 0.0001. c ST208 phylogenetic tree based on Bayesian Binary Markov Chain Monte Carlo (BMM) model. Each small coloured circle at the tips of the phylogenetic tree represents an isolate, with different colours indicating different KLs, as shown in the legend on the right. The pie chart of internal nodes represents the KL state of ancestral nodes inferred by BMM method. Hidden probabilities less than 5% are lumped together and reposted as * (white). Source data are provided as a Source Data file.
We identified 2058, 891 and 1284 core SNPs after the removal of the recombination regions of the genomes of ST208, ST191 and ST195, respectively. The nonrecombinant region of the ST208 genome presented more SNPs, especially in genes related to cell wall/membrane/envelope biogenesis, extracellular structures, and carbohydrate transport and metabolism (Figs. S11c, S12). Recombination hotspots, particularly in the genomes of the ST208 and ST191 strains, were concentrated in regions associated with CPS, and type IV secretion systems (Fig. S12). Recombination of the CPS region occurred in the ST208-KL7 strain and the ST208-KL2 strain, which evolved similarly to ST208-KL7, suggesting that the CPS region of the ST208-KL7 genome may be derived from the CPS region of the ST208-KL2 genome (Fig. S13). Further evolutionary analysis revealed that the ST208-KL2 strain is indeed the most recent common ancestor (MRCA) of all the ST208 strains (Fig. 7c). Nucleotide divergence analysis within the same ST revealed less divergence in ST195 than in ST191 and ST208, before and after removing recombinant sequence regions (mean pairwise divergence: 25.94435, 59.73938 and 59.74454, respectively; p < 0.001 according to the Wilcoxon rank-sum test, Fig. S11d). The r/m values for ST208, ST191, and ST195 were 32.436, 30.657, and 20.526, respectively, indicating significantly higher recombination rates in the genomes of ST208 and ST191 than in that of ST195. These findings suggest that the ability of ST208 to acquire exogenous recombinant genes is greater than that of the other strains, highlighting its enhanced genomic plasticity, which could contribute to its adaptation.
The number and proportion of MGEs in the genome of ST208 were significantly greater than those in the genomes of ST191 and ST195 (p < 0.001, Wilcoxon rank-sum test, Fig. 8a, b). The total number of transposons (Tn), integrative conjugative elements (ICEs), phages, and genomic islands in the genome of ST208 was significantly greater than that in the genomes of ST191 and ST195 (3.62\(\,\pm \,\)1.14 vs 2.24\(\,\pm \,\)0.97 vs 3.43\(\,\pm\) 0.67; 11.39\(\,\pm \,\)2.04 vs 8.56\(\pm\)1.83 vs 8.97\(\pm\)1.70; 45.59\(\pm\)6.82 vs 42.55\(\pm\)6.60 vs 44.10\(\pm\)4.02; 19.75\(\,\pm \,\)5.93 vs 17.62\(\,\pm \,\)2.65 vs 17.49\(\,\pm \,\)1.96, respectively; Wilcoxon rank-sum test, p < 0.05) (Fig. 8c–f). In the MGE category with the greatest difference, nine ICEs exhibited significant differences among the three STs (Kruskal‒Wallis, p < 0.05), with six ICEs being most prevalent in the genome of ST208. ICEs with relatively high carriage rates in the genome of ST208 carried the aminoglycoside resistance-related genes AAC(6’)-Ib7, APH(3’)-Ia, and aadA; the disinfectant tolerance-related gene qacE; and the sulfonamide resistance-related gene sul1 (Fig. S14a). These genes were more prevalent in the genome of ST208 than in that of ST191 or ST195 (Fig. 6, Fig. S8). The six Tns that had the highest carriage rate in the genome of ST208 were associated with mainly aminoglycoside resistance- and macrolide resistance-related genes (Fig. S14b). No drug resistance-related genes were found among the phage-related proteins that presented the highest carrying rates in ST208 (Fig. S14c). This suggests that the genome of ST208 acquires more resistance genes through ICEs and Tns.
a Violin plots displayed MGEs number distribution of the ST191, ST195 and ST208 isolates, ST208 presented a significantly higher abundance of MGEs (p < 3.9 × 10−10). b MGEs distribution of the ST191, ST195 and ST208 isolates, ST208 exhibited a significantly higher proportion of MGEs (p < 3.5 × 10−10). The quantity distribution of transposons (Tn, c, p < 3.9 × 10−10), integrative conjugative elements (ICEs, d, p < 0.0009), phages (e, p < 0.0074), and islands (f, p < 4.6 × 10−8) in each isolate of ST191, ST195 and ST208. Statistical tests used Wilcoxon rank-sum test. For (a), violin plots show MGEs number distribution combined with boxes show the median and interquartile range (IQR) while whiskers extend to a maximum of 1.5× IQR. Dots indicate outliers beyond whiskers. For (b, f), boxes show the median and interquartile range (IQR) while whiskers extend to a maximum of 1.5× IQR. Dots indicate outliers beyond whiskers. The statistical significance is shown by the number of asterisks as follows: *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, NS. indicates no statistical significance. Source data are provided as a Source Data file.
To better understand whether the differences in prophages, plasmids, and ISs between the STs were due to vertical or horizontal transfer, we reconstructed the ancestral states of these MGEs. Our results indicated that the large-scale expansion of Tns, ICEs, phages and islands within ST208 was likely caused by multiple acquisition and loss events within ST208 (Fig. 9), suggesting a complex pattern of horizontal transfer. These findings support the critical roles of MGEs in shaping the population structure of prevalent STs. ST208 exhibits an evolutionary strategy in which its accessory gene pools are reshaped and genetic diversity is accumulated at the population level.
MGEs were mapped as continuous characters onto the phylogenetic tree of the genomes. Evolution was reconstructed via the R package phytools, including the number of Tns (a), ICEs (b), phages (c), and islands (d) identified per genome. The colours represent the number of MGEs detected per genome, as indicated by the colour bars. Source data are provided as a Source Data file.
ST208 was disseminated through multiple interprovincial transmission events
To explore whether the dissemination ability of ST208 is superior to that of ST191 or ST195, we conducted discrete trait phylogeographic inference for them (Fig. 10). Using a constant population approach with the GTR substitution model and strict clock model (MCMC chain length: 1 × 108), we investigated clonal replacement and its correlation with modified transmission patterns. Using phylogeographic analysis, we aimed to reconstruct the evolutionary histories and transmission dynamics of these prevalent STs.
National distributions and major transmission of ST191 (a), ST195 (b) and ST208 (c). The background colour of the map represents the proportion of isolates in each province. The dotted line represents one-way transmission, and the solid line represents two-way transmission. The thickness of the arrow represents the number of major transmission events. Lines of different colours represent the sources of transmission in different provinces, and the red asterisk indicates the central province of transmission. d The number of observed all transmissions originating from each region. The predominant sources (e.g. Zhejiang, Anhui and Yunnan) are highlighted in orange. The provinces represented on the x-axis are abbreviated using the first letters of their two-syllable names, such as ZJ for Zhejiang and AH for Anhui. Source data are provided as a Source Data file.
The common ancestor of ST191 dates to approximately 1995 [95% Highest Posterior Density (HPD), 1991–1999) and originated in ZJ. All the ST191-KL9 strains were grouped within the same clade, which emerged in approximately 2010, which is consistent with the cgSNP-based clustering results. ST191 isolates clustered based on their isolation locations, indicating nosocomial clonal transmission (Fig. S15). We identified a total of 26 cross-regional transmissions along the ST191 phylogeny, approximately 53.85% (14/26) of these transmissions were major transmission event. The earliest occurring between ZJ and AH in 1995 and 2001, and after that, it spread in both directions between ZJ Province and AH Province. ZJ Province and AH Province are important hubs in the spread of ST191 in the country (Fig. 10a, d). The common ancestor of ST195 dates to 1996 (95% HPD 1992-2000), when it originated from ZJ. ST195 initially emerged in ZJ and subsequently diverged into two major clades. One clade predominantly comprised strains isolated in ZJ, with a few from AH, indicating a prevalent distribution in ZJ and limited spread to AH. The other clade included strains from various regions nationwide, with recent ancestors originating from AH, suggesting the dissemination of AH-originating strains across the country (Fig. S16). Among the 56 predicting cross-regional transmissions in ST195, 40 transmissions were major transmission event. AH Province is the province with the most ST195 transmissions in and out, with 40 transmission events originating from AH Province, highlighting AH as a transmission hub for ST195 (Fig. 10b, d). The initial introduction of ST208 occurred in AH in 1987 (95% HPD 1982-1992), followed by its spread to Yunnan (Fig.S17). As a result, varying degrees of ST208 epidemics were observed in most regions of China (Fig. 10c, Fig. S17). BEAST analysis predicted a total of 69 transmission events between provinces, including 36 major transmission events. These transmission events involved 21 provinces, with AH being the most frequent origin and destination for transmission (Fig. 10c, d).
Overall, compared with ST191 and ST195, ST208 has undergone more complex transmission events and a greater number of transmission nodes. In contrast to ST191 and ST195, ST208 demonstrates denser nationwide transmission, broader dissemination, and earlier initiation of interprovincial spread (Fig. 10, Figs. S15–17). Interprovincial transmission events have resulted in the current distributions of these prevalent STs in China, and these events are likely facilitated by the movement of the population. AH, the second largest province in China in terms of population outflow, produced the second largest number of isolates involved in this study, thereby serving as a crucial hub for the transmission of A. baumannii.
Discussion
Although A. baumannii has a severe impact on clinical treatment, there are very few long-term and comprehensive epidemiological studies on BSI-causing A. baumannii isolates worldwide13. To our knowledge, this study is the largest BSI-causing A. baumannii isolates genomic epidemiology study ever conducted, and conducted over the longest period. The global spread of A. baumannii has been driven by that of several major lineages, including IC1 and IC2. IC2, also known as global clone (GC)2, has been observed to be the predominant clinically isolated A. baumannii lineage3,14,28. In this study, we also found that the IC2 strains were dominant. We observed an increasing diversity of all isolates over time and a shift in the prevalent STs among BSI-causing A. baumannii isolates in China, characterised by an increase in the proportion of ST208 and a decrease in that of ST191 and ST195, reflecting similar trends observed in global datasets. Moreover, other STs isolated from BSIs in China but rare in other countries deserve further genomic epidemiology study, such as the fourth- and fifth-ranked STs, ST540 and ST369. It is still unknown how they evolved and became prevalent, whether they will spread from China to other countries, and what their virulence levels are.
A. baumannii ST208 was first detected in Australia in 1999, with isolates subsequently found in the United States and various European and Asian countries29,30,31,32. As one of the most prevalent lineages, ST208 has caused numerous difficult-to-treat infections and outbreaks worldwide33,34. In recent years, several outbreaks of CRAB ST208 have occurred in China, posing a serious public health threat34,35,36. Gao et al. reported that ST208 might have originated from North America and subsequently evolved into two clades37. In this study, we demonstrated that ST208 has become a complete epidemic. We discovered that increased virulence drove ST208 infection, increased desiccation tolerance and the propensity to acquire ARGs, thereby driving its survival. A significant factor contributing to the success of A. baumannii ST208 is its enhanced genomic plasticity. The adaptable genome undergoes rapid mutations, including recombination and point mutations, in response to challenges and stressors22. These results are important for understanding the dynamic changes and evolutionary trends of epidemic clones of A. baumannii. The genome of A. baumannii is an open pangenomic bacterial pathogen that is highly plastic, making it highly adaptable to different environments38,39,40. However, the fundamental reasons behind this genomic plasticity remain unclear41,42. It is unknown whether the variation in genomic plasticity among different STs is determined by specific genetic factors or is a result of random horizontal gene transfer events. Further, whether STs with greater plasticity have an absolute advantage in evolution, or there is still a possibility of them being replaced, is not clear. These questions warrant further research in the future.
Notably, A. baumannii has become increasingly virulent in recent years7,19,20,27. An increasing number of VFs have been described that may contribute to the pathogenicity of A. baumannii18,43,44. Among the major virulence determinants, surface polysaccharides, especially capsules, are crucial for protecting bacteria from phagocytosis and the bactericidal effects of serum or the host immune response7. Considering the capsule’s exposure to selective pressures, a certain level of capsular diversity can be anticipated19. Although capsular variation in A. baumannii has been documented, there is a lack of information regarding whether specific capsule types are associated with epidemic clones23. Among the two main KLs of ST208 isolates, legionaminic acid (KL7) and pseudaminic acid (KL2) belong to the nonulosonic acid superfamily, which shares structural similarities with eukaryotic sialic acid19,45,46,47. Notably, legionaminic acid facilitates the ability of a pathogen to mimic the host cell surface, thus allowing it to evade the host immune response19,47. Furthermore, the presence of capsule derivatives enriched in nonulosonic acid sugars, which enhance adaptation to host‒pathogen interactions by masking bacterial cells from the host immune system, appears to contribute to the success and predominance of A. baumannii ST208.
Our study emphasises the importance of assessing the evolutionary and functional properties of A. baumannii KLs at the population level to better monitor and predict the emergence of prevalent and virulent clones. Therefore, there is a need for updated epidemiological insights into the most prevalent and clinically relevant KLs. The ability to acquire different KLs through recombination is a crucial factor in the prevalence of STs, suggesting potential turnover of STs in the future. The success of STs is, to some extent, linked with the success of KLs. In summary, the continued long-term dominance of ST208 may not be guaranteed, as other STs or KLs, which are more virulent and environmentally adaptable, could replace ST208-KL2 and ST208-KL7.
Current epidemiological studies regarding A. baumannii have used the Pasteur scheme or Oxford scheme for MLST analysis14,18,23,37,48. At the outset, we explored both schemes, recording the assigned types and the prevalent clone IC2 (Supplementary Data 1). While the Pasteur scheme mostly grouped strains as ST2, the Oxford scheme revealed greater diversity. To study the evolution and internal variation of prevalent clones, we aimed to strike a balance between the conservativeness and resolution of typing methods. Ultimately, we selected the Oxford scheme for its higher resolution. Further, this scheme also reflects important evolutionary features of A. baumannii, making it relevant to our study.
This study has several limitations. Although we observed a fluctuating increasing trend in the isolation rate of non-IC2 strains over time, which is consistent with the phenomenon reported by Wang et al. in the United States3, further in-depth analysis was not conducted because factors such as dispersed clustering and high diversity still merit attention. Whether these non-IC2 clones exhibit increased virulence and enhanced environmental adaptability and whether they will gradually become predominant in future BSI-causing A. baumannii isolates require further research and continuous monitoring. Furthermore, why ST208 has undergone more extensive transmission events, in addition to population mobility, is unclear and requires further experimental investigation to identify other contributing factors. Additionally, we did not perform statistical analysis to determine whether infections with ST208 compared with those with ST191, ST195, or other STs affect treatment outcomes.
Methods
Strain collection and whole-genome sequencing
This study involved 1,506 unique A. baumannii isolates from more than 54 thousand BSI patients whose data were collected via the National Surveillance for Blood Bacterial Resistant Investigation Collaborative System (BRICS) between January 2011 and December 2021 from 76 secondary and tertiary hospitals distributed across 25 provinces in China. The isolates were submitted quarterly to the central laboratory of the First Affiliated Hospital of Zhejiang University by all the hospitals and then subjected to species identification via Matrix-assisted laser desorption ionisation time-of-flight mass spectrometry (MALDI-TOF/MS, Bruker Daltonik GmbH, Bremen, Germany). This study complies with all relevant ethical regulations and was approved by the Ethics Committee of Zhejiang University First Affiliated Hospital (Ethics approval number: IIT202103IIB).
The genomic DNA of 1506 A. baumannii isolates was extracted via Gentra Puregene Yeast/Bact. Kit (Qiagen, San Francisco, CA, USA). Whole-genome sequencing was performed on an Illumina NovaSeq 6000 PE150 platform (Illumina, San Diego, CA, United States).
Genome assembly and sequence typing
After trimming and filtering the low-quality bases with PRINSEQ-lite (version 0.19.3)49, we assembled the pair-end reads de novo via SPAdes (version 3.11.1)50 and evaluated the assemblies via QUAST (version 5.02)51. The ribosomal multilocus sequence typing (https://pubmlst.org/species-id) method was used as a supplement for species identification. In silico multilocus sequence typing (MLST) was performed via mlst (version 2.19.0) (https://github.com/tseemann/mlst). New STs identified in this study have been submitted to the pubMLST database (ST3225 to 3271). International Clone (ICs) were identified via the goeBURST52 algorithm. The capsular polysaccharide (KL) and lipooligosaccharide outer core (OCL) loci were identified via Kaptive (version 2.0.7)53. Diversity indices of STs were calculated via a custom script available on GitHub (https://github.com/ahmedmagds/rarefaction-curves).
Genome annotation
We detected the coding sequences (CDSs) from assemblies via Prokka (version 1.13.0)54, annotated their functions, and identified the antimicrobial (antibiotics or biocides) resistance genes (ARGs), virulence factors (VFs), and disinfectant-related genes via DIAMOND (version v2.0.14)55 against the Clusters of Orthologous Groups of Proteins (COG), Comprehensive Antibiotic Resistance Database (CARD), virulence factors database (VFDB, http://www.mgc.ac.cn/VFs/main.htm. version 2022, set B) and BacMet datasets, respectively.
Additionally, various types of mobile genetic elements (MGEs) were annotated. Transposons (Tns) were identified in our curated database, encompassing 357 unique transposons from TnCentral, TRANSPOSON REGISTRY, and many other studies. For plasmid typing, we also integrated a database containing 902 unique plasmids from the PlasmidFinder and Acinetobacter PlasmidTyping databases. Moreover, insertion sequences (ISs), Integrative and conjugative elements (ICEs), phages, and genomic islands were identified via ISfinder, ICEberg, Islandviewer4 (https://www.pathogenomics.sfu.ca/islandviewer), and PHASTER, respectively. The ancestral IS/Tn/phage state was reconstructed with maximum likelihood via the fastAnc function in the R package phytools (Version 2.1-1)56.
Variation analysis and recombination detection
We identified variants by aligning the assemblies to the reference genome, A. baumannii BJAB07104 (accession number: NC_021726.1), via Minimap2 (version 2.26-r1175)57 with the parameter “asm20.” After short alignments (<200 bp) were filtered, we used nucleotide sequences aligned at each site against the reference genome to generate the “pseudogenome” for each isolate. These consensus sequences were subjected to Gubbins (version 2.4.1)58 for recombination identification with default parameters. Moreover, the Gubbins output files were used to calculate the ratio of the number of SNPs inside the recombinations to the number of SNPs outside the recombinations (r/m).
We additionally applied read mapping-based analysis to call more accurate IC2 variants via Snippy (version 4.6.0)59. The variants include single nucleotide variants (SNVs) and short-indels where the alternative bases are called by ≥5 mapped reads. Variants supported by ≥95% of the reads were considered homozygous mutations; otherwise, they were considered heterozygous mutations. The homozygous SNVs in nonrecombinant regions called by both the mapping- and assembly based analyses above were selected for phylogenetic analysis.
Phylogenetic analysis
After annotating the assembled genomes via Prokka (Version 1.13.0)54, we analysed the core and pan genes via Roary (Version 3.12.0)60, in which the homologous genes were clustered via the Markov Cluster Algorithm (MCL) algorithms in CD-HIT (Version 4.7.0)61 with the following settings: thresholds of 90% Basic Local Alignment Search Tool Protein (BLASTP) identity and 100% presence in all the isolates and filtering of paralogues. To construct the core genome alignment, the alignments of each gene were concatenated according to the gene coordinates in the reference genome. RaxML (version 8.2.12)62 was then used to construct the maximum likelihood (ML) phylogeny with a GTR model and 500 rapid bootstrap replications, midpoint rooting method is used to root the tree.
Notably, this is the first study to elucidate the phylogenetic structure of a large population containing thousands of A. baumannii strains. To address this issue, we removed the duplicated core genome sequences to reduce redundant information in the large population and used the outgroup A. baumannii XH857 (accession number: NZ_CP014540.1, Oxford ST806) to root the tree. RaxML (version 8.2.12) was then used to construct the maximum likelihood (ML) phylogeny with a General Time Reversible (GTR) model and 100 rapid bootstrap replications. The phylogenetic lineages were subsequently inferred via a hierarchical Bayesian analysis of population structure (hierBAPS) model in R (rHierBAPs) with a maximum depth of five and an initial population size of 5063. iTOL (version 6.9)64 was used for visualising and annotating the phylogenetic trees.
We constructed a maximum likelihood phylogenetic tree using non-recombinant SNP sequences of 234 strains of ST208, and the Bayesian binary Markov chain Monte Carlo (BMM) method in RASP (Version 4.0)65 was used to analyze the status of KL in the ST208 phylogenetic tree. According to the KL type of ST208, the strains were divided into two states, KL2 and KL7. The analysis used a fixed JC model with the following parameters: 5,000,000 cycles, 10 chains, 0.1 temperature, sampling every 100 iterations.
Phylogeographic analysis
We next conducted discrete trait phylogeographic inference for the ST195, ST208, and ST191 isolates via their nonrecombinant core SNP alignment via BEAST (version 2.7.4)66. BEAST priors were introduced with BEAUti (version 2.7.5)66, including a strict molecular clock model with a lognormal distribution of the evolutionary rate, an Hasegawa-Kishino-Yano (HKY) nucleotide substitution model with invariant sites and a coalescence constant population to model the changes in population size over time. The analyses were performed via Markov chain Monte Carlo (MCMC) with at least 50,000,000 states, a 10% burn-in, and sampling of parameters every 3000 steps. We monitored the convergence of the MCMC chains via Tracer (version 1.7.2)67, ensuring that each estimated parameter had an effective sample size (ESS) > 200. The maximum clade credibility (MCC) tree under each model was generated in TreeAnnotator (version 2.7.5) and plotted in FigTree (version 1.4.4) (https://github.com/rambaut/figtree).
We visualised the nationwide spatial transmission of A. baumannii output by SpreaD3 (version 0.9.6)68, with ggplot2 labelling the transmission events as either “major transmission” or “tip transmission“68. The former is characterised by the different geographical states (referred to as provinces in this study) of the common ancestor between two nodes, and the latter is defined as where the tip isolate originated from a province rather than its most recent common ancestor.
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was initially conducted via a VITEK-2 system (bioMérieux, Lyon, France) in the participating hospitals and was further confirmed via the agar and/or broth dilution method in the central laboratory. The results were interpreted according to the Clinical and Laboratory Standards Institute and European Committee (CLSI, 2023) or Antimicrobial Susceptibility Testing v.13.0 (http://www.eucast.org/clinical_breakpoints/). Carbapenem resistance was defined as a minimum inhibitory concentration (MIC) of ≥8 mg/L for imipenem or meropenem. Tigecycline resistance was defined as a MIC of ≥8 mg/L. Polymyxin resistance was defined as a MIC of >2 mg/L.
Disinfectant tolerance assay
Bacterial isolates are grown overnight in Luria-Bertani Broth (LB) broth at 37 °C and adjusted to a turbidity of 0.5 McFarland. Disinfectants are serially diluted to various concentrations (e.g., 0.5×, 1×, 2×, and 4× the Minimum Inhibitory Concentration (MIC)) and incorporated into molten agar medium. The medium is poured into Petri dishes and allowed to solidify. Subsequently, bacterial suspensions are inoculated onto the surface of the agar medium using a bacterial multipoint inoculator, followed by incubation at 37 °C. The MIC is determined as the lowest disinfectant concentration that inhibits visible bacterial growth. All experiments are performed in triplicate, and statistical analysis is conducted to evaluate bacterial tolerance.
Antiserum complement killing assay
Blood collected from healthy volunteers was centrifuged and filtered through a 0.22 mm pore size syringe filter to obtain sterilised serum. Half of the serum was inactivated by heating in a 56 °C water bath for 30 min. A. baumannii in the logarithmic growth phase was adjusted to a concentration of 2 × 106 colony-forming units (CFU)/ml and mixed with normal or inactivated serum at a ratio of 1:9. After being incubated for 1 h at 37 °C, the samples were serially diluted and spread on Mueller-Hinton (MH) agar plates. Following overnight incubation at 37 °C, bacterial colonies were counted, and the bacterial survival rate was calculated via the following formula: bacterial survival rate = (number of colonies in normal serum/number of colonies in inactivated serum) × 100%. We did three biological replications of these experiments.
Desiccation tolerance assay
Bacterial cultures were grown overnight in LB broth at 37 °C. The bacterial suspension was adjusted to an optical density equivalent to a 0.5 McFarland standard. A 10 µL volume of the adjusted suspension was inoculated onto a 96-well plate and air-dried under ambient conditions. Then, the plate was transferred to a controlled environmental chamber (DHTHM-27, DHT, Shanghai) maintained at 25 °C with 20% relative humidity (RH). To establish the baseline bacterial load (D0), serial dilutions of the suspension were plated on LB agar and incubated for 16 h to determine colony-forming units (CFU). After 48 h of desiccation, each well was rehydrated with 200 µL of phosphate-buffered saline (PBS, pH 7.2), followed by serial dilution and plating for CFU enumeration. Post-desiccation bacterial survival (D2) was determined, and survival rates were calculated accordingly.
Mouse infection model
Eight-week-old female BALB/c mice (to reduce variability caused by sex-related physiological and hormonal differences) were injected with 100 μL of sterile NaCl solution containing 1 × 106 CFU of each strain through the intraperitoneal injection (five mice were injected with each strain). The physical condition of each mouse was monitored every 12 h. All surviving mice were euthanized after 7 days of injection. All animal experiments were conducted following the guidelines of the Institutional Animal Care and Ethics Committee at The First Affiliated Hospital of Zhejiang University, School of Medicine (number: 2022-835).
Statistical analysis
PERMANOVA (Permutational multivariate analysis of variance) analyze the explanatory power of different factors on the differences in the distribution of VFs. Continuous variables, represented by the means ± SDs, were statistically tested by the Wilcoxon rank-sum test and the Kruskal‒Wallis test or Dunn’s test for multiple comparisons. P values or FDR-adjusted P values (Padj) ≤ 0.05 were assumed to be statistically significant.
Data visualisation
The histograms, alluvial diagrams, Sankey diagrams, boxplots, violin plots, and heatmaps used in this study were drawn in R (version 4.2.2). Principal component analysis (PCA) of VFs between ST195, ST208, and ST191 was performed via anosim functions in the R package vegan (version 2.6.4). The R package ggplot2 (version 3.4.0) was used for map generation.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Processed data are available in Supplementary data 1. The sequencing datasets generated in this study were publicly available in the NCBI database (BioProject: PRJNA1120174). Source data are provided as a Source Data file. Source data are provided with this paper.
Code availability
The custom code used in this study is freely available at the link (https://doi.org/10.5281/zenodo.14875779).
References
Antimicrobial Resistance, C. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399, 629–655 (2022).
Luo, Q. et al. ESKAPE in China: epidemiology and characteristics of antibiotic resistance. Emerg. Microbes Infect. 2317915, https://doi.org/10.1080/22221751.2024.2317915 (2024).
Wang, M. et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant acinetobacter baumannii among patients from different global regions. Clin. Infect. Dis. 78, 248–258 (2024).
Organization, W. H. Antimicrobial resistance surveillance in Europe 2022–2020 data. (World Health Organization. Regional Office for Europe, 2022).
Collaborators, G. B. D. A. R. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 400, 2221–2248 (2022).
Musicha, P. et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998-2016): a surveillance study. Lancet Infect. Dis. 17, 1042–1052 (2017).
Harding, C. M., Hennon, S. W. & Feldman, M. F. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat. Rev. Microbiol. 16, 91–102 (2018).
Peleg, A. Y., Seifert, H. & Paterson, D. L. Acinetobacter baumannii: emergence of a successful pathogen. Clin. Microbiol. Rev. 21, 538–582 (2008).
Giammanco, A., Cala, C., Fasciana, T. & Dowzicky, M. J. Global assessment of the activity of tigecycline against multidrug-resistant gram-negative pathogens between 2004 and 2014 as Part of the tigecycline evaluation and surveillance trial. mSphere 2, https://doi.org/10.1128/mSphere.00310-16 (2017).
Mohd Sazlly Lim, S., Zainal Abidin, A., Liew, S. M., Roberts, J. A. & Sime, F. B. The global prevalence of multidrug-resistance among Acinetobacter baumannii causing hospital-acquired and ventilator-associated pneumonia and its associated mortality: a systematic review and meta-analysis. J. Infect. 79, 593–600 (2019).
Russo, A. et al. Bloodstream infections caused by carbapenem-resistant Acinetobacter baumannii: Clinical features, therapy and outcome from a multicenter study. J. Infect. 79, 130–138 (2019).
WHO Bacterial Priority Pathogens List, 2024: bacterial pathogens of public health importance to guide research, development and strategies to prevent and control antimicrobial resistance. Geneva: World Health Organization; 2024. Licence: CC BY-NC-SA 3.0 IGO.
Whiteway, C., Breine, A., Philippe, C. & Van der Henst, C. Acinetobacter baumannii. Trends Microbiol. 30, 199–200 (2022).
Doughty, E. L. et al. Endemicity and diversification of carbapenem-resistant Acinetobacter baumannii in an intensive care unit. Lancet Reg. Health West Pac. 37, 100780 (2023).
Migliaccio, A. et al. Inhibition of AdeB, AceI, and AmvA efflux pumps restores chlorhexidine and benzalkonium susceptibility in Acinetobacter baumannii ATCC 19606. Front. Microbiol. 12, 790263 (2022).
Li, L. et al. Systematic analyses identify modes of action of ten clinically relevant biocides and antibiotic antagonism in Acinetobacter baumannii. Nat. Microbiol. 8, 1995–2005 (2023).
Lucidi, M. et al. Pathogenicity and virulence of Acinetobacter baumannii: factors contributing to the fitness in healthcare settings and the infected host. Virulence 15, 2289769 (2024).
Hua, M. et al. The novel outer membrane protein from OprD/Occ family is associated with hypervirulence of carbapenem resistant Acinetobacter baumannii ST2/KL22. Virulence 12, 1–11 (2021).
Weiss, D. S. et al. Capsule carbohydrate structure determines virulence in Acinetobacter baumannii. PLOS Pathog. 17, https://doi.org/10.1371/journal.ppat.1009291 (2021).
Yu, K. et al. Bloodstream infections caused by ST2 Acinetobacter baumannii: risk factors, antibiotic regimens, and virulence over 6 years period in China. Antimicrob. Resist. Infect. Control 10, 16 (2021).
Bai, B. et al. Clinical and genomic analysis of virulence-related genes in bloodstream infections caused by Acinetobacter baumannii. Virulence 13, 1920–1927 (2022).
Imperi, F. et al. The genomics of Acinetobacter baumannii: insights into genome plasticity, antimicrobial resistance and pathogenicity. IUBMB Life 63, 1068–1074 (2011).
Muller, C. et al. A global view on carbapenem-resistant Acinetobacter baumannii. mBio 14, e0226023 (2023).
Hsieh, Y. C. et al. Association of capsular types with carbapenem resistance, disease severity, and mortality in Acinetobacter baumannii. Emerg. Microbes Infect. 9, 2094–2104 (2020).
Hamidian, M. & Nigro, S. J. Emergence, molecular mechanisms and global spread of carbapenem-resistant Acinetobacter baumannii. Microb. Genom. 5, https://doi.org/10.1099/mgen.0.000306 (2019).
Hu, F. et al. Carbapenem-resistant Klebsiella pneumoniae capsular types, antibiotic resistance and virulence factors in China: a longitudinal, multi-centre study. Nat. Microbiol. 9, 814–829 (2024).
Silva, L. et al. The success of particular Acinetobacter baumannii clones: accumulating resistance and virulence inside a sugary shield. J. Antimicrob. Chemother. 76, 305–311 (2021).
Kang, H. M., Yun, K. W. & Choi, E. H. Molecular epidemiology of Acinetobacter baumannii complex causing invasive infections in Korean children during 2001-2020. Ann. Clin. Microbiol Antimicrob. 22, 32 (2023).
Adams-Haduch, J. M. et al. Molecular Epidemiology of Carbapenem-Nonsusceptible Acinetobacter baumannii in the United States. J. Clin. Microbiol. 49, 3849–3854 (2011).
Tada, T., Miyoshi-Akiyama, T., Shimada, K., Shimojima, M. & Kirikae, T. Dissemination of 16S rRNA Methylase ArmA-Producing Acinetobacter baumannii and Emergence of OXA-72 Carbapenemase Coproducers in Japan. Antimicrob. Agents Chemother. 58, 2916–2920 (2014).
Jeon, H. et al. Molecular epidemiology of carbapenem-resistant Acinetobacter baumannii isolates from a Korean hospital that carry blaOXA-23. Infect. Genet. Evol. 58, 232–236 (2018).
Chen, Y., Wu, L., Chen, Y., Xu, Z. & Xu, L. Draft genome sequence of a multidrug-resistant bla OXA-23 -producing Acinetobacter baumannii ST208 isolate from China. J. Glob. Antimicrob. Resist. 4, 42–43 (2016).
Giannella, M. & Viale, P. Treating carbapenem-resistant Acinetobacter baumannii infections. Lancet Infect. Dis. 23, 994–995 (2023).
Yang, J. L. et al. Association of capsular polysaccharide locus 2 with prognosis of Acinetobacter baumannii bacteraemia. Emerg. Microbes Infect. 11, 83–90 (2022).
Wang, X., Du, Z., Huang, W., Zhang, X. & Zhou, Y. Outbreak of multidrug-resistant Acinetobacter baumannii ST208 producing OXA-23-like carbapenemase in a children’s hospital in Shanghai, China. Microb. Drug Resist. 27, 816–822 (2021).
Jiang, M. et al. Epidemiological analysis of multidrug-resistant acinetobacter baumannii isolates in a tertiary hospital over a 12-Year period in China. Front. Public Health 9, https://doi.org/10.3389/fpubh.2021.707435 (2021).
Gao, Y. et al. Origin, phylogeny, and transmission of the epidemic clone ST208 of carbapenem-resistant acinetobacter baumannii on a global scale. Microbiol. Spectr. 10, e0260421 (2022).
Wright, M. S., Mountain, S., Beeri, K. & Adams, M. D. Assessment of insertion sequence mobilization as an adaptive response to oxidative stress in Acinetobacter baumannii using IS-seq. J. Bacteriol. 199, https://doi.org/10.1128/jb.00833-00816 (2017).
Baumgart, L. A. et al. Persistence and plasticity in bacterial gene regulation. Nat. Methods 18, 1499–1505 (2021).
Dobrindt, U. & Hacker, J. Whole genome plasticity in pathogenic bacteria. Curr. Opin. Microbiol. 4, 550–557 (2001).
Wang, P. et al. Mobile genetic elements used by competing coral microbial populations increase genomic plasticity. ISME J. 16, 2220–2229 (2022).
Verma, J. et al. Genomic plasticity associated with antimicrobial resistance in Vibrio cholerae. Proc. Natl Acad. Sci. USA 116, 6226–6231 (2019).
Pérez-Varela, M. et al. Evidence for Rho-dependent control of a virulence switch in Acinetobacter baumannii. Mbio 15, e02708–e02723 (2024).
Li, P. et al. The role of type VI secretion system genes in antibiotic resistance and virulence in Acinetobacter baumannii clinical isolates. Front. Cell. Infect. Microbiol. 14, 1297818 (2024).
Singh, J. K., Adams, F. G. & Brown, M. H. Diversity and function of capsular polysaccharide in acinetobacter baumannii. Front. Microbiol. 9, 3301 (2018).
Wyres, K. L., Cahill, S. M., Holt, K. E., Hall, R. M. & Kenyon, J. J. Identification of Acinetobacter baumannii loci for capsular polysaccharide (KL) and lipooligosaccharide outer core (OCL) synthesis in genome assemblies using curated reference databases compatible with Kaptive. Microb. Genom. 6, https://doi.org/10.1099/mgen.0.000339 (2020).
Knirel, Y. A. et al. 5,7-Diamino-3,5,7,9-tetradeoxynon-2-ulosonic Acids in the Capsular Polysaccharides of Acinetobacter baumannii.Biochemistry 88, 202–210 (2023).
Liu, C. et al. Epidemiological and genetic characteristics of clinical carbapenem-resistant Acinetobacter baumannii strains collected countrywide from hospital intensive care units (ICUs) in China. Emerg. Microbes Infect. 11, 1730–1741 (2022).
Cantu, V. A., Sadural, J. & Edwards, R. PRINSEQ++, a multi-threaded tool for fast and efficient quality control and preprocessing of sequencing datasets. Preprint at https://doi.org/10.7287/peerj.preprints.27553v1 (2019).
Bankevich, A. et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29, 1072–1075 (2013).
Francisco, A. P., Bugalho, M., Ramirez, M. & Carriço, J. A. Global optimal eBURST analysis of multilocus typing data using a graphic matroid approach. BMC Bioinforma. 10, 1–15 (2009).
Lam, M. M., Wick, R. R., Judd, L. M., Holt, K. E. & Wyres, K. L. Kaptive 2.0: updated capsule and lipopolysaccharide locus typing for the Klebsiella pneumoniae species complex. Microb. Genom. 8, 000800 (2022).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Buchfink, B., Xie, C. & Huson, D. H. Fast and sensitive protein alignment using DIAMOND. Nat. Methods 12, 59–60 (2015).
Revell, L. J. phytools: an R package for phylogenetic comparative biology (and other things). Methods Ecol. Evol. 2, 217–223 (2012).
Li, H. Minimap2: pairwise alignment for nucleotide sequences. Bioinformatics 34, 3094–3100 (2018).
Croucher, N. J. et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 43, e15–e15 (2015).
Seemann, T. Snippy: rapid haploid variant calling and core SNP phylogeny. GitHub. Available at: github. com/tseemann/snippy (2015).
Page, A. J. et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31, 3691–3693 (2015).
Fu, L., Niu, B., Zhu, Z., Wu, S. & Li, W. CD-HIT: accelerated for clustering the next-generation sequencing data. Bioinformatics 28, 3150–3152 (2012).
Stamatakis, A. RAxML version 8: a tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 30, 1312–1313 (2014).
Tonkin-Hill, G., Lees, J. A., Bentley, S. D., Frost, S. D. & Corander, J. RhierBAPS: an R implementation of the population clustering algorithm hierBAPS. Wellcome open research 3, 93 (2018).
Letunic, I. & Bork, P. Interactive Tree of Life (iTOL) v6: recent updates to the phylogenetic tree display and annotation tool. Nucleic Acids Res. 52, W78–W82 (2024).
Yu, Y., Blair, C. & He, X. RASP 4: ancestral state reconstruction tool for multiple genes and characters. Mol. Biol. Evol. 37, 604–606 (2020).
Bouckaert, R. et al. BEAST 2: a software platform for Bayesian evolutionary analysis. PLoS Comput. Biol. 10, e1003537 (2014).
Rambaut, A., Drummond, A. J., Xie, D., Baele, G. & Suchard, M. A. Posterior summarization in Bayesian phylogenetics using Tracer 1.7. Syst. Biol. 67, 901–904 (2018).
Bielejec, F. et al. SpreaD3: interactive visualization of spatiotemporal history and trait evolutionary processes. Mol. Biol. Evol.33, 2167–2169 (2016).
Acknowledgements
This work was supported by the National Key Research and Development Program of China (2021YFC2300300 to Y.X.). This work was partially supported by grants from the Key Research and Development Program of Zhejiang Province (No. 2021C03068 to Y.X.), the Natural Science Foundation of Zhejiang Province, China (No. LY24H190002 to Q.L.), and the National Natural Science Foundation of China (No. 32070667, No. 81971984 to H.Z.).
Author information
Authors and Affiliations
Consortia
Contributions
Y.X., H.Z., and Q.L. conceived the project and revised the manuscript. The BRICS Working Group collected the bacterial isolates and epidemiological data. Y.C., P.S., J.J., C.Y., and Z.L. performed the preliminary laboratory analyses. P.L., T.X., P.S., W.Y. Y.M., and E.Z. performed the experiments. M.C., Q.G., X.J., and Y.Z. performed the data analysis. Q.L. and M.C. wrote the manuscript, Q.L., M.C., and Q.G. revised the manuscript. Y.X. and H.Z. are the guarantors of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Benjamin Evans, Branko Jovcic and Raffaele Zarrilli for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Luo, Q., Chang, M., Lu, P. et al. Genomic epidemiology and phylodynamics of Acinetobacter baumannii bloodstream isolates in China. Nat Commun 16, 3536 (2025). https://doi.org/10.1038/s41467-025-58772-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-58772-9