Abstract
SARS-CoV-2 variants present diverse clinical manifestations, necessitating deeper insights into their pathogenic effects. This study employs multi-omics approaches to investigate the molecular mechanisms underlying SARS-CoV-2 infection, focusing on vascular damage. Plasma proteomic analysis of unvaccinated participants infected with Omicron BA.2.76 or ancestral variants identifies key signaling pathways associated with endothelial dysfunction, with the vinculin (VCL) pathway emerging as a hallmark of Omicron infections, contributing to lung exudation. Metabolomic analysis of plasma samples from the same cohort reveals disruptions in immune function, cell membrane integrity, and metabolic processes, including altered tricarboxylic acid cycle and glycolysis pathways. An integrated analysis of proteomic and metabolomic data underscores the role of VCL in inflammation and extravasation, highlighting its interactions with adhesion molecules and inflammatory metabolites. A validation cohort of plasma samples from Omicron-infected participants confirms this association by replicating proteomic analysis, showing elevated VCL levels correlated with inflammatory markers. Functional studies in a male rat model of lung injury demonstrate that anti-VCL intervention reduces plasma VCL levels, mitigates alveolar edema, and restores alveolar-capillary barrier integrity, as assessed by histological staining and electron microscopy, thereby illustrating VCL modulation’s impact on vascular leakage and extravasation. These findings establish VCL as a potential therapeutic target for mitigating vascular complications in SARS-CoV-2 infections.
Similar content being viewed by others
Introduction
Five years have passed since the initial report of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection caused by the ancestral variant, the earliest strain identified from samples collected from December 2019 to May 20201,2,3. During this time, the virus has mutated extensively, with the Omicron variant becoming the most dominant globally at one point4. Research shows that various SARS-CoV-2 variants, though primarily affecting the respiratory system, also affect different extrapulmonary systems5. Employing multi-omics studies grounded in the hematological ecosystem, combined with a collaborative multi-method validation approach, allows for precisely capturing the comprehensive pathological landscape of SARS-CoV-25.
The damage mechanism of SARS-CoV-2 is primarily attributed to the host immune system dysfunction resulting in uncontrolled inflammation, rather than the direct toxicity of the virus. However, viral load is directly correlated with the severity clinical outcomes6. Once immune dysfunction takes place within the lungs, uncontrolled inflammatory chemotaxis leads to the secretion of numerous cytokines, causing damage to alveolar epithelium and vascular endothelium. The damage can even progress to the development of deep vein micro thrombosis or bleeding, disruption of the gas-blood barrier, and potential complications like multiple organ failure7,8. The likelihood of severe cases with the Omicron variant is lower, and these cases are characterized by mild inflammation. Research has found that changes in the condition of mild to moderate symptoms do not necessarily parallel changes in infection indicators such as C-reactive protein (CRP), procalcitonin (PCT), and inflammatory cells. These indicators may even remain at clinically normal levels9,10. According to the most recent research, although Omicron exhibits lower infection indicators and decreased risk when contrasted with the ancestral and Delta variants, it should not be classified as a “mild” variant of Coronavirus Disease 2019 (COVID-19)4,11. Previous studies by our team have identified that coagulation-related pathways play a critical role in symptomatic Omicron infections, though the key pathways and proteins involved remain unknown12. At the same time, compared with original variant, what unique symptoms, disease progression, and diagnostic indicators Omicron has remained to be explored. Understanding the unique impacts of the Omicron variant on the human body is crucial for shaping public health strategies and therapeutic approaches that address not only the current but also emerging viral variants, thereby enhancing our capacity to manage COVID-19 effectively.
Compared to the ancestral variant, the Omicron variant has approximately twice the affinity for ACE2, making it more transmissible. In terms of respiratory symptoms, Omicron is almost indistinguishable from earlier variants and generally causes milder symptoms4. However, Omicron infections exhibit highly heterogeneous characteristics, with symptoms ranging from asymptomatic to severe pneumonia, respiratory distress, organ dysfunction, and even death in participants across all age groups13. This diversity in infection outcomes highlights the importance of further research into Omicron’s pathogenic mechanisms. A study has shown that the damaging effect on the blood-gas barrier during persistent lung functional impairment during and post-hospitalization is the main cause of refractory hypoxemia14, but the mechanism remains unclear. Furthermore, the ambiguous disease characteristics in low-risk populations pose challenges for assessing Omicron’s progression. There has been debate over the definition of asymptomatic Omicron, with arguments suggesting that Omicron infections, whether asymptomatic or symptomatic, can initiate humoral immune responses14. Currently, the chemotaxis mechanisms guiding inflammatory cells remain unclear6. Despite Omicron variants generally being considered less severe in symptoms, revealing potential damage pathways in Omicron’s hematological ecosystem and identifying key targets to effectively block blood-gas barrier exudation pathways can enhance oxygenation and reduce clinical mortality.
In this work, we recruited distinct cohorts of unvaccinated participants infected with Omicron BA.2.76 or ancestral variants, alongside healthy controls, to uncover reproducible proteins and pathways, extending our prior study12. Employing multi-omics approaches, proteomic and metabolomic profiling of plasma, we compared Omicron and ancestral variant infections, pinpointing the VCL/ICAM-1 pathway as a key driver of blood-gas barrier damage and inflammatory exudation in Omicron, distinct from ancestral variant’s broader inflammatory profile. Integrated omics revealed disrupted immune and metabolic cascades, with rat models of Omicron-like lung injury validating VCL/ICAM-1’s role in vascular leakage, mitigated by targeted intervention. By incorporating validation cohorts and diverse analytical methods, we ensured robust findings, delineating molecular mechanisms underlying Omicron’s unique pathogenesis and its impact on gas exchange.
Results
Clinical information profile of participants
In this study, participants were sampled immediately upon hospital admission after disease onset and confirmation by etiological testing. This ensures that the samples reflect the early response to infection. Additionally, all participants included in the Omicron-infected cohort had no prior vaccination history and no known previous SARS-CoV-2 infection. Although up to 87% of the Chinese population was vaccinated during the Omicron wave, a subset of participants remained unvaccinated due to personal concerns, medical contraindications, or other reasons. By including only unvaccinated and previously uninfected participants, we aimed to isolate the specific effects of the Omicron variant on the blood proteome without the confounding influence of prior immune exposure. As detailed in Supplementary Table 1, we investigated the clinical features of COVID-19 across different patient groups, with a specific emphasis on laboratory biomarkers. In participants infected with Omicron, we observed higher Actual Forced Vital Capacity (FVC.A), Actual Forced Vital Capacity to Predicted Ratio (FVC.A/Pd), Actual Forced Expiratory Volume in 1 Second (FEV1.A), and Actual Forced Expiratory Volume in 1 Second to Predicted Ratio (FEV1.A/Pd), as well as low HRCT Score, as detailed in Supplementary Table 2. Notably, neutrophil counts were significantly elevated in severe participants with ancestral variant COVID-19 compared to those infected with the non-severe Omicron variant and healthy controls. This observation underscores the role of SARS-CoV-2 in stimulating an aggressive neutrophilic response, which may contribute to tissue invasion and subsequent damage as the disease progresses. Furthermore, our study documented a decrease in lymphocyte populations, potentially attributable to viral mechanisms that either directly engage these cells or induce collateral damage through inflammatory mediators. Interestingly, monocyte levels remained consistent in severe participants infected with ancestral variant when compared to HC, yet were significantly elevated in those infected with the Omicron variant. This variation highlights different immunological responses elicited by distinct viral variants.
Our analysis also revealed reductions in eosinophils and basophils in participants infected with ancestral variant, cells known for their capacity to produce IL-4 and enhance the proliferation of activated B cells and T cells. The decline in these cell types may contribute to the observed decrease in lymphocyte counts, further complicating the immune response in participants infected with COVID-19. We found that the number and proportion of monocytes were significantly increased in the Omicron variant compared to HC and ancestral variant. Additionally, we observed marked increases in the inflammatory marker CRP, indicating a pronounced inflammatory state within these participants (Fig. 1a). Plasma markers of extrapulmonary organ dysfunction, such as lactate dehydrogenase (LDH), aspartate aminotransferase (AST), and alanine aminotransferase (ALT), were also elevated in both Omicron-infected and ancestral variant-infected groups, suggesting widespread organ impact beyond the respiratory system. Elevated plasma glucose (GLU) levels were noted alongside a decreasing trend in Creatinine (Cr), adding complexity to the metabolic disruptions observed in participants infected with SARS-CoV-2 (Fig. 1b). Additional plasma markers, including prothrombin time, international normalized ratio, fibrinogen, and activated partial thromboplastin time, while within normal ranges, were significantly elevated in both patient groups, pointing to subtle yet significant differences in their coagulative responses. Elevated D-dimer levels aligned with findings of microvascular inflammation and an increased thrombosis risk in COVID-19 cases. Additionally, we found that myoglobin (MYO) levels were significantly higher in participants infected with Omicron compared to both HC and participants infected with ancestral variant (Fig. 1c). Blood gas analysis revealed varying degrees of respiratory failure predominantly in hospitalized participants infected with ancestral variant (Fig. 1d), in contrast to participants infected with Omicron who exhibited no such complications upon admission. A notable decrease in CD3 + T lymphocytes, CD4 + T lymphocytes, CD8 + T lymphocytes, CD16 + CD56 + NK cells, and CD19 + B lymphocytes was observed across both symptomatic groups (Fig. 1e).
a Blood Routine: Comparison of white blood cell count (WBC), neutrophil count (NEU), lymphocyte count (LYM), monocyte count (MONO), C-reactive protein (CRP), and their respective percentages across healthy controls, Omi-Asymptomatic, Omi-Symptomatic, and ancestral groups. b Biochemistry: Plasma levels of various biochemical markers including Blood urea nitrogen (BUN), Glucose (GLU), Creatinine (Cr) and Calcium (Ca). c Thromboembolism and Myocardial Injury: Coagulation parameters including activated partial thromboplastin time (APTT), D-dimer (D-D), fibrinogen (FIB), prothrombin time (PT), and markers of myocardial injury such as myoglobin (MYO), lactate dehydrogenase (LDH), creatine kinase (CK), and aspartate aminotransferase (AST). d Blood Gas Analysis: Parameters indicative of respiratory and metabolic status including pH, hemoglobin (Hb), methemoglobin (MetHb), hematocrit (Hct), standard base excess (SBE), and standard bicarbonate (SBC). e Lymphocyte Subpopulations: Levels of various lymphocyte subpopulations including CD3 + CD8 + , CD3 + CD19 + , CD3 + CD15 + , CD4 + CD8 + , CD3 + CD4 + , CD3 + CD45 + , CD3 + CD56 + CD16 + , and CD3 + CD16 + CD56+ across the different patient groups. Data are presented as mean values ± SEM. n (healthy control) = 20. n (Omi-Asymptomatic) = 20. n (Omi-Symptomatic) = 20. n (ancestral) = 20. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for multiple comparisons. ***P < 0.001; **P < 0.01; *P < 0.05.
Proteomic characterization analysis and pathway enrichment
No Omicron viral proteins were detected in any of the samples. In this study, we conducted a comparative analysis among three groups: healthy participants, participants infected with Omicron, and participants infected with the ancestral variant SARS-CoV-2. This approach enabled a retrospective exploration of the proteomic characteristics of Omicron compared to the healthy control group and the ancestral variant (Fig. S1a). The proteomic analysis encompassed 726 proteins, for which high-quality quantitative data were obtained (Fig. S1b). By comparing data from the asymptomatic infection group with the healthy control group, we identified 51 differentially expressed proteins (DEPs) within the plasma proteome. Employing a similar methodology, we detected 62 DEPs in symptomatic participants infected with Omicron and 83 DEPs in participants with the ancestral variant. Furthermore, in comparison to participants with the ancestral variant, 82 DEPs were observed in asymptomatic participants infected with Omicron, while symptomatic participants infected with Omicron exhibited 98 DEPs (Fig. S1c-h and Supplementary Data 1). Notably, minimal differences were observed in the plasma proteome analysis between asymptomatic and symptomatic participants. Among the DEPs, we have identified several ubiquitous proteins that are potential contributors to the complex inflammatory exudation process affecting the blood-gas barrier (Fig. S1i-k, Supplementary Data 2). Enrichment analysis employing Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways revealed several pathways linked to platelet response and vascular system damage in participants infected with various viral variants.
Comparing Omi-Asymptomatic and healthy control (Fig. 2a), the enrichment analysis showed significant GO pathways involved in hemostasis, coagulation, blood coagulation, and the regulation of body fluid levels. Other notable pathways included platelet activation, vesicle lumen, and cytoplasmic vesicle lumen. Metabolic and cellular processes such as glycolysis/gluconeogenesis, focal adhesion, and the Rap1 signaling pathway were highlighted in the KEGG pathways. These findings suggest that even asymptomatic participants experience substantial changes in platelet function and vascular responses. Comparing Omi-Symptomatic and healthy control (Fig. 2b), the enrichment analysis showed significant GO pathways involved in homeostasis, blood coagulation, and extracellular matrix organization. Prominent metabolic processes were also highlighted, such as glycolysis and glucagon signaling. KEGG pathways pointed to glycolysis/gluconeogenesis, focal adhesion, and the PI3K-Akt signaling pathway, suggesting significant metabolic reprogramming and changes in cell adhesion mechanisms during symptomatic Omicron infection. For the Omi-Asymptomatic vs. ancestral comparison (Fig. 2c), dominant GO pathways were complemented and coagulation cascades, blood coagulation, and immune response. Platelet activation and neutrophil degranulation were particularly noted, indicating a focused immune reaction. The KEGG pathways included complement and coagulation cascades, platelet activation, and regulation of the actin cytoskeleton, with a notable enrichment of neutrophil extracellular trap formation pointing to an enhanced immune defense mechanism. In the comparison between Omi-Symptomatic and ancestral (Fig. 2d), major GO pathways involved blood coagulation, complement activation, and vesicle-mediated transport. Cellular detoxification and oxidative stress responses were also significant. KEGG pathways highlighted glycolysis/gluconeogenesis, focal adhesion, and leukocyte trans endothelial migration, suggesting increased cell adhesion and significant metabolic changes in symptomatic participants compared to ancestral variant.
When comparing the different groups, several common pathways such as blood coagulation and platelet activation were consistently altered, indicating a universal response to SARS-CoV-2 infection. However, pathways like glycolysis/gluconeogenesis and focal adhesion in symptomatic participants infected with Omicron point to more nuanced metabolic and cellular changes compared to ancestral variant infection. The presence of immune-related pathways such as neutrophil degranulation and extracellular trap formation in participants infected with Omicron also highlights potentially distinct immune response mechanisms compared to ancestral variant. Details of GO and KEGG pathways are shown in Supplementary Data 3–7.
Selection of Omicron core pathways and targets
To gain deeper insights into the core pathways of Omicron, a protein-protein interaction network analysis (PPI) was conducted using the differentially expressed proteins identified in the previous analysis. By examining the interactions among proteins, we aimed to elucidate the mechanisms underlying disease progression following infection with different viral variants.
In the comparison of Omi-Asymptomatic vs. healthy control (Fig. 3a), core pathways centered around proteins such as ALDOA, LDHA, and ACTG1, indicating significant metabolic and structural protein alterations. This suggests that even asymptomatic Omicron infections impact fundamental cellular processes, particularly those involved in metabolism and structural integrity. Similarly, in the Omi-Symptomatic vs. healthy control comparison (Fig. 3b), key proteins like GSN, FLNA, and VCL were highlighted, pointing to changes in the cytoskeleton and cellular adhesion mechanisms. These alterations in structural proteins and adhesion pathways underscore the significant cellular remodeling occurring during symptomatic Omicron infections. In the Omi-Asymptomatic vs. ancestral comparison (Fig. 3c), proteins such as VWF, FGG, and C9 were central, suggesting notable differences in coagulation and immune response pathways. This indicates that even without symptoms, Omicron infection elicits distinct immune and coagulative responses compared to the ancestral variant. For the Omi-Symptomatic vs. ancestral comparison (Fig. 3d), key proteins included ITIH3, F12, and FGB, emphasizing the significant involvement of coagulation and inflammatory pathways. These findings highlight the robust inflammatory and coagulative responses in ancestral variant infections, which are more pronounced than in Omicron infections.
a–d Hub Proteins Analysis showing the PPI network of differentially expressed proteins in Omi-Asymptomatic vs. healthy control, Omi-Symptomatic vs. healthy control, Omi-Asymptomatic vs. ancestral, and Omi-Symptomatic vs. ancestral. e–h Function Enrichment of Hub Proteins Bar charts showing enriched Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways in different comparative groups, emphasizing pathways related to actin cytoskeleton, coagulation, and immune response. i, j Heatmaps Revealing patterns and correlations of key hub proteins in asymptomatic and symptomatic groups. k, l RT-qPCR Verification Validation of VCL and ICAM-1expression levels in different patient groups. Data are presented as mean values ± SEM. n (healthy control) = 20. n (Omi-Asymptomatic) = 20. n (Omi-Symptomatic) = 20. n (ancestral) = 20. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for multiple comparisons. *P < 0.05. **P < 0.01.***P < 0.001.
Functional enrichment analysis of hub proteins further elucidates these differences. In Omi-Asymptomatic vs. healthy control (Fig. 3e), GO pathways highlighted actin filament organization, pyruvate metabolic processes, and lactate metabolic processes. KEGG pathways included glycolysis/gluconeogenesis, adherens junction, and pyruvate metabolism. This enrichment underscores the metabolic reprogramming and alterations in cell adhesion even in the absence of symptoms. In Omi-Symptomatic vs. healthy control (Fig. 3f), significant GO pathways included actin cytoskeleton organization, coagulation, and platelet activation. KEGG analysis revealed focal adhesion, leukocyte transendothelial migration, and bacterial invasion of epithelial cells. These findings suggest that symptomatic Omicron infections impact both structural cellular functions and immune responses, leading to enhanced cellular adhesion and migration activities.
For Omi-Asymptomatic vs. ancestral (Fig. 3g), dominant GO pathways included acute inflammatory response, biological processes involved in immune response, and collagen-containing extracellular matrix. KEGG pathways highlighted complement and coagulation cascades, platelet activation, and neutrophil extracellular trap formation. This indicates that asymptomatic Omicron infections still provoke significant immune responses, although they differ from those seen in ancestral variant infections. In Omi-Symptomatic vs. ancestral (Fig. 3H), major GO pathways involved blood coagulation, fibrin clot formation, and collagen metabolic process. KEGG pathways included complement and coagulation cascades, platelet activation, and cell adhesion molecules. These pathways suggest that symptomatic Omicron infections lead to complex immune and coagulative responses similar to those observed in ancestral variant infections, but with certain distinctions in specific biological processes. Details of GO and KEGG pathways are shown in Supplementary Data 8–12.
Heatmaps revealing patterns and correlations of key hub proteins in asymptomatic and symptomatic groups are shown in Fig. 3i-k. These heatmaps highlight different expression levels of hub proteins, with notable patterns for proteins like VCL and ICAM1 across different patient groups. Elevated VCL and ICAM1 levels were confirmed in participants infected with SARS-CoV-2 through RT-qPCR verification (Fig. 3k-l), supporting the proteomic findings and suggesting their role in adhesion and exudation processes. When comparing the different groups, several common pathways such as blood coagulation and platelet activation were consistently altered, indicating a universal response to SARS-CoV-2 infection. However, specific pathways like glycolysis/gluconeogenesis and focal adhesion in symptomatic participants infected with Omicron highlight nuanced metabolic and cellular changes compared to ancestral variant infection. The presence of immune-related pathways such as neutrophil degranulation and extracellular trap formation in participants infected with Omicron also underscore potentially distinct immune response mechanisms compared to ancestral variant. Our validation cohort (Fig. S2, Supplementary Table 3) and previous work12 confirmed our findings.
Metabolite screening and pathway enrichment analysis
Metabolomic analysis, employing the same grouping strategy, extended our investigation into the microenvironment, identifying a total of 1780 valid metabolites in this study. By excluding metabolite sets linked to dietary intake and steroids, which can be influenced by external factors, and focusing on the inflammatory microenvironment in participants infected with SARS-CoV-2, we identified several significant differences. These differences encompassed metabolites central to maintaining inflammatory equilibrium, including arachidonic acid, 11-HETE, and DHA, along with metabolic pathways associated with energy homeostasis, such as tricarboxylic acid (TCA) metabolism and pyruvate-lactate metabolism. Target metabolites were selected based on VIP > 1, |logFC | > 1, and p < 0.05 criteria.
Our comprehensive metabolite screening and pathway enrichment analysis revealed distinct metabolic signatures among the different groups: healthy controls, Omi-Asymptomatic, Omi-Symptomatic, and ancestral. Heatmaps illustrated these metabolic profiles, underscoring significant metabolic reprogramming in response to SARS-CoV-2 infection (Fig. 4a). In the Omi-Asymptomatic vs. healthy control comparison (Fig. 4b), significant pathways included purine metabolism, drug metabolism (cytochrome P450), sphingolipid metabolism, retinol metabolism, steroid hormone biosynthesis, and caffeine metabolism. These findings indicate that even asymptomatic Omicron infections induce substantial metabolic changes affecting nucleotide metabolism, xenobiotic detoxification, lipid signaling, and hormone biosynthesis. For the Omi-Symptomatic vs. healthy control comparison (Fig. 4c), notable pathways were drug metabolism (cytochrome P450), glycerophospholipid metabolism, sphingolipid metabolism, ether lipid metabolism, steroid hormone biosynthesis, caffeine metabolism, and purine metabolism. These changes reflect the metabolic burden and cellular stress in symptomatic Omicron infections, with extensive modifications in lipid metabolism and hormone biosynthesis. The ancestral vs. healthy control comparison (Fig. 4d) highlighted pathways such as metabolism of xenobiotics by cytochrome P450, aminoacyl-tRNA biosynthesis, tryptophan metabolism, anandamide metabolism, lysine degradation, retinol metabolism, and steroid hormone biosynthesis. The broad metabolic reprogramming in ancestral variant infections suggest extensive impacts on amino acid metabolism, neurotransmitter biosynthesis, and hormonal regulation.
a Profiles of metabolites between different groups showing distinct metabolic signatures across healthy controls, Omi-Asymptomatic, Omi-Symptomatic, and ancestral groups. b-f Venn diagrams and pathway enrichment analyses for Omi-Asymptomatic vs. healthy control, Omi-Symptomatic vs. healthy control, ancestral vs. healthy control, Omi-Asymptomatic vs. ancestral, and Omi-Symptomatic vs. ancestral. Key pathways include purine metabolism, drug metabolism, sphingolipid metabolism, steroid hormone biosynthesis, and more. g–o Tricarboxylic Acid Cycle Metabolites and Anaerobic Glycolysis Metabolites showing differential expression of key metabolites involved in energy production and metabolic regulation. Data are presented as mean values ± SEM. n (healthy control) = 20. n (Omi-Asymptomatic) = 20. n (Omi-Symptomatic) = 20. n (ancestral) = 20. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for multiple comparisons. *P < 0.05. **P < 0.01.***P < 0.001.
In the Omi-Asymptomatic vs. ancestral comparison (Fig. 4e), pathway enrichment identified changes in metabolism of xenobiotics by cytochrome P450, purine metabolism, aminoacyl-tRNA biosynthesis, primary bile acid biosynthesis, pyrimidine metabolism, and biosynthesis of unsaturated fatty acids. These findings highlight differential metabolic adjustments in response to asymptomatic Omicron and ancestral variant infections, particularly in nucleotide metabolism and lipid biosynthesis. For the Omi-Symptomatic vs. ancestral comparison (Fig. 4f), significant pathways included metabolism of xenobiotics by cytochrome P450, drug metabolism (cytochrome P450), aminoacyl-tRNA biosynthesis, primary bile acid biosynthesis, pyrimidine metabolism, and biosynthesis of unsaturated fatty acids. The enrichment in xenobiotic metabolism and bile acid biosynthesis pathways underscores the hepatic and detoxification challenges in symptomatic Omicron infections compared to ancestral.
Analysis of Tricarboxylic Acid (TCA) cycle intermediates showed differential expression of metabolites such as fumaric acid, L-malic acid, citric acid, succinic acid, isocitric acid, oxoglutaric acid, and oxaloacetic acid among the groups (Fig. 4g-m). These metabolites are critical for energy production and metabolic homeostasis, with significant variations reflecting the impact of SARS-CoV-2 on cellular respiration and metabolic flux. Notably, participants infected with ancestral variant exhibited concurrent increases in TCA levels and anaerobic glycolysis, whereas participants infected with Omicron displayed heightened TCA cycle activity while maintaining relatively normal anaerobic glycolysis. Levels of anaerobic glycolysis metabolites, including pyruvic acid and lactic acid, were measured (Fig. 4n-o). These changes indicate a shift towards anaerobic energy production, possibly due to hypoxic conditions induced by severe infections.
Integrated proteomics and metabolomics analysis
To comprehensively understand the interplay between proteomic and metabolomic changes in participants infected with SARS-CoV-2, we performed an integrated analysis using MetaboAnalyst. This approach allowed us to identify interconnected pathways involving differentially expressed proteins and metabolites across various patient groups. The identified pathways were then subjected to functional enrichment analysis to elucidate their biological significance.
In the comparison between Omi-Asymptomatic and healthy control (Fig. 5a), the interaction network highlighted key connections among proteins like ICAM1, VCL, GRN, THBS1, and CALM1, with all-trans-retinoic acid being a central metabolite. For Omi-Symptomatic vs. healthy control (Fig. 5b), a similar network was observed with proteins ICAM1, VCL, CA2, PRDX2, THBS1, and CALM1 interacting through all-trans-retinoic acid. These networks suggest that retinoic acid metabolism plays a pivotal role in both asymptomatic and symptomatic Omicron infections. In the ancestral vs. healthy control comparison (Fig. 5c), the network included proteins such as CAT, GAPDH, MMP9, and TIMP1, with hypoxanthine and all-trans-retinoic acid as central metabolites. Additionally, thymol was identified as another significant metabolite interacting with proteins like ELANE and IGFBP4. This indicates more complex metabolic interactions and suggests that ancestral variant SARS-CoV-2 infection affects a broader range of biological processes compared to Omicron.
a–c Different groups of protein and metabolite interaction networks showing key proteins and metabolites in Omi-Asymptomatic vs. healthy control, Omi-Symptomatic vs. healthy control, and ancestral vs. healthy control. d–f Interactive protein enrichment pathway bar charts for Omi-Asymptomatic vs. healthy control, Omi-Symptomatic vs. healthy control, and ancestral vs. healthy control, emphasizing pathways related to cell migration, immune response, coagulation, and various signaling mechanisms.
The functional enrichment of interactive proteins in Omi-Asymptomatic vs. healthy control (Fig. 5d) revealed pathways related to epithelial cell migration, macrophage activation, coagulation regulation, and calcium ion transport. Notably, pathways such as the Rap1 signaling pathway and focal adhesion were enriched, indicating significant changes in cell adhesion and signaling mechanisms. For Omi-Symptomatic vs. healthy control (Fig. 5e), enriched pathways included regulation of coagulation, platelet activation, and immune response regulation. Key signaling pathways such as the Rap1 signaling pathway, TGF-beta signaling pathway, and p53 signaling pathway were also highlighted, suggesting alterations in cell survival, proliferation, and immune modulation in symptomatic Omicron infections. In ancestral vs. healthy control (Fig. 5f), enriched pathways encompassed cell killing, acute inflammatory response, interferon production, and regulation of epithelial cell proliferation. Significant signaling pathways included the NF-kappa B signaling pathway, TNF signaling pathway, and Toll-like receptor signaling pathway, highlighting robust immune and inflammatory responses in ancestral variant SARS-CoV-2 infections.
Correlation analysis of the VCL pathway and clinical/metabolomic markers
Based on the proteomic findings, the VCL pathway appears to serve as a central hub in the extravasation pathway. To gain further insights into the role of the VCL pathway in inflammation, adhesion, and extravasation functions, a correlation analysis was conducted with clinical inflammation markers and inflammation-related molecules identified in the study. The correlation analysis unveiled a significant positive association between VCL and several clinical inflammation markers, including CRP, PCT, and SAA (serum amyloid A). VCL also displayed a positive correlation with the inflammation-related metabolite ARA (arachidonic acid) and DHA (docosahexaenoic acid). Additionally, a noteworthy positive correlation was noted between VCL and CT scores, which directly assess extravasation levels clinically (Fig. 6a–c). These correlations suggest that VCL may play a critical role in mediating inflammatory responses and vascular permeability in participants infected with SARS-CoV-2. Scatter plots were utilized to graphically represent specific correlation parameters (Fig. 6d-f). In the Omi-Asymptomatic group (Fig. 6d), VCL showed significant correlations with CRP and CT scores. In the Omi-Symptomatic group (Fig. 6e), VCL correlated strongly with CRP, CT scores, and SAA. In the ancestral group (Fig. 6f), significant correlations were observed between VCL and ICAM-1, CRP, PCT, and CT scores. These plots highlight the consistent relationship between VCL expression and inflammatory and extravasation markers across different patient groups.
a–c Correlation analysis between VCL and key indicators in Omi-Asymptomatic, Omi-Symptomatic, and ancestral groups. d–f Scatter plots illustrating the correlation of VCL with CRP, CT scores, and other clinical markers in Omi-Asymptomatic, Omi-Symptomatic, and ancestral groups. g Overall differences in N-glycosylation across healthy controls, Omi-Asymptomatic, Omi-Symptomatic, and ancestral groups. h N-glycosylation model diagram of VCL. Created in BioRender. Xue, M. (2025) https://BioRender.com/m14t653. i-j Comparison of N-glycosylation levels of VCL and ICAM-1 across different patient groups. Data are presented as mean values ± SEM. n (healthy control) = 20. n (Omi-Asymptomatic) = 20. n (Omi-Symptomatic) = 20. n (ancestral) = 20. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for multiple comparisons. *P < 0.05. **P < 0.01.***P < 0.001.
N-glycosylation of VCL and ICAM-1
N-glycosylation is a crucial protein modification for extracellular extravasation and adhesion functions with significant biological implications in immune responses and host-virus interactions. N-glycans can form covalent bonds with proteins through the free NH2 group of aspartic acid residues. The study investigated the N-glycosylation levels across the entire proteome (Fig. 6g). It was observed that N-glycosylation modifications of VCL in participants infected with SARS-CoV-2 exhibited a macroscopic trend of gradual increase, progressing from asymptomatic participants infected with Omicron to symptomatic participants infected with Omicron, and further to participants infected with SARS-CoV-2 ancestral variant, displaying a significant linear rise (Fig. 6h-i). This increase in N-glycosylation may enhance the extravasation and adhesion capabilities of VCL, contributing to the inflammatory and vascular changes observed in severe COVID-19 cases. In contrast, ICAM-1 displayed a linear decrease in N-glycosylation levels (Fig. 6j). The differential glycosylation patterns of VCL and ICAM-1 underscore the complex regulatory mechanisms governing protein function in response to SARS-CoV-2 infection. These findings shed light on the role of VCL pathway modifications in inflammation, adhesion, and extravasation functions, as well as their correlation with clinical markers and disease outcomes in participants infected with SARS-CoV-2.
Validation and analysis of the lung injury rat model
To validate the findings from our studies, we conducted animal experiments using a lung injury rat model. The experimental process is illustrated in Fig. 7a, which outlines the stages of adaptive feeding, nasal drip intervention, sampling, and comprehensive analysis. Blood plasma analysis (Fig. 7b-e) revealed notable increases in VCL, ICAM-1, HBP, and CRP levels in the lung injury model group. These elevated levels were significantly reduced following Anti-VCL intervention, suggesting a mitigation of the inflammatory response. Histological examination using hematoxylin and eosin (HE) staining demonstrated that healthy rats had intact alveolar structures with a thin and uniform interstitium, and an absence of inflammatory cell infiltration (Fig. 7f). In contrast, lung injury rats showed collapsed alveolar structures, thickened interstitium with inflammatory cell infiltration, the presence of red blood cells, and alveolar edema (Fig. 7g). Post-Anti-VCL intervention, there was a marked reduction in alveolar edema, though some alveoli did not fully expand, and interstitial thickening persisted (Fig. 7h). A detailed analysis of the alveolar-capillary barrier in HE-stained sections (Fig. 7i-l) revealed severe damage to the respiratory membrane in the lung injury group, characterized by interstitial thickening or rupture, reduced surfactant material on alveolar surfaces, alveolar edema, and mucus release by airway mucosal cells obstructing peripheral alveoli. Despite intervention, the interstitium still contained numerous fibroblasts, resulting in an abnormal alveolar structure, which might contribute to incomplete lung function recovery.
a Flowchart of the animal experiment process. Created in BioRender. Xue, M. (2025) https://BioRender.com/b88o369. b-e Plasma analysis showing increases in VCL, ICAM-1, HBP, and CRP levels in the lung injury model group, with reductions following Anti-VCL intervention. f-h HE-stained sections showing histological differences in alveolar structures among control, no-intervention, and inhibitor injection groups (n = 5). i-l Schematic diagrams illustrating the effects of lung injury patterns on the air-blood barrier. i Created in BioRender. Xue, M. (2025) https://BioRender.com/r67l605. j Created in BioRender. Xue, M. (2025) https://BioRender.com/x01c615. k Created in BioRender. Xue, M. (2025) https://BioRender.com/l87k962. l Created in BioRender. Xue, M. (2025) https://BioRender.com/m91k627. m–o Lung tissue immunofluorescence showing the distribution of VCL and its increased expression in lung injury (n = 5). p–u Transmission electron microscopy images of the alveolar-capillary barrier across different groups (n = 5). Data are presented as mean values ± SEM. n (Control) = 5. n (No-intervention) = 5. n (Inhibitor injection) =5. Statistical significance was determined using one-way ANOVA followed by Tukey’s post hoc test for multiple comparisons. *P < 0.05. **P < 0.01.***P < 0.001.
Protein immunofluorescence was employed to observe the distribution of the cellular skeleton protein VCL. The results demonstrated a significant increase in VCL expression during lung injury, indicating heightened cellular activity in the inflammatory environment. VCL’s distribution distinctly outlined the alveolar structure, and its presence in edema fluid was notably absent, further underscoring VCL’s crucial role as a support protein for alveolar cell skeleton structure (Fig. 7m-o). Transmission electron microscopy was utilized to visualize the alveolar-capillary barrier. In normal respiratory membranes, the structure included uniform alveolar surfactant thickness, ACE type I alveolar epithelium, matrix cells, and collagen fibers (Fig. 7p). ACE II cells featured intact lamellar bodies, essential for supplementing surfactant material and maintaining alveolar structure (Fig. 7q). In lung injury tissues, the alveolar-capillary barrier significantly thickened, alveolar surfactant and ACE type I alveolar epithelium sustained damage, the matrix was exposed in the alveolar cavity, leading to thickening, and fibroblasts proliferated massively (Fig. 7r). Lamellar bodies were depleted, rendering it impossible to promptly replenish the gap in the alveolar surfactant layer, leading to the rupture of ACE II surface microvilli (Fig. 7s). Post Anti-VCL intervention, the respiratory membrane structure essentially returned to normal, although fibroblasts continued to proliferate (Fig. 7t-u).
Discussion
Omicron variant as a milestone in understanding SARS-CoV-2 evolution
Studying the Omicron variant, even after its peak has passed, importantly advances our knowledge on virus evolution, and refining public health strategies for future pandemics. This study compared participants infected with Omicron to healthy participants and those with the ancestral variant, utilizing clinical tests and multi-omics methods to reveal Omicron’s pathogenic characteristics. Participants infected with Omicron exhibited milder symptoms, such as cough, dyspnea, chest distress, and fever, with no apparent lung issues or gas exchange problems. Clinical tests showed elevated infection markers like CRP in both participants infected with Omicron and those infected with ancestral variant, along with abnormalities in D-dimer and clotting times, indicating extrapulmonary organ damage in both groups.
Some studies have suggested that the clinical indicators of Omicron do not show specificity compared to healthy controls, possibly due to a shorter acute symptom window period15. To validate this viewpoint, further subgroup analysis was conducted, revealing that symptomatic participants infected with Omicron generally presented with acute symptoms (e.g., fever, cough, dyspnea, fatigue) at the time of enrollment, whereas asymptomatic participants infected with Omicron were only nucleic acid-positive without the aforementioned symptoms. However, even so, in this study, asymptomatic and symptomatic participants infected with Omicron showed differences only in white blood cell counts in terms of laboratory parameters, with no significant differences in inflammatory factors like CRP, PCT, etc., and inflammatory cells between the two groups. On the other hand, we found that monocytes and MYO were increased in participants infected with Omicron compared with HC and ancestral variant. Imaging findings also showed no significant differences, consistent with another study that was able to only mildly differentiate participants infected with Omicron16, highlighting the inconsistency between clinical symptoms, laboratory tests, and imaging findings in participants infected with Omicron. Overall, compared to the ancestral variant, Omicron induces milder inflammation and damage, but the severity of clinical symptoms and laboratory parameters is not entirely consistent.
In addition to clinical findings, immune cell counts, especially CD8 + T lymphocytes, were affected in both participants infected with Omicron and those infected with ancestral variant. CD8 + T lymphocytes, crucial for virus suppression, exhibited different responses in the early stages of SARS-CoV-2 infection, with more pronounced impairments in severe cases. Furthermore, while the majority of participants infected with ancestral variant experienced reduced lymphocyte counts, symptomatic participants infected with Omicron also showed decreased T lymphocyte counts. Asymptomatic participants infected with Omicron, on the other hand, had T lymphocyte counts similar to healthy controls17. Utilizing various omics techniques, this study compared Omicron and ancestral variant infections, identifying abnormal inflammation and coagulation pathways in ancestral variant. In the Omicron group, despite subtle clinical changes, distinctive inflammatory responses and abnormal metabolic pathways were detected. These findings indicate an energetically demanding state due to localized inflammation, contributing to symptoms resembling previous variants18. Although our study identified enrichment of heart disease-related pathways in Omicron infections, acute myocarditis (AM) has been considered a rare complication of COVID-19. A recent study found that most individuals infected with the Omicron variant did not exhibit significant myocardial damage19. Another study further supported this finding, demonstrating that compared to the ancestral variant, the Omicron variant exerts a significantly attenuated effect on human iPSC-derived cardiomyocytes20. Given that the incidence of myocardial injury in participants infected with Omicron has not been thoroughly investigated, future research is needed to explore the potential pathophysiological mechanisms between cardiovascular disease and Omicron variant. Despite these findings, troponin remains a more reliable and accurate marker for detecting even subtle cardiac injury. However, since the potential for Omicron-related heart injury was an unexpected discovery in our study, troponin was not included in our original clinical tests. Our proteomics data did not reveal elevated troponin levels, which may be due to insufficient sensitivity to detect such low-abundance troponin. We acknowledge this as a limitation of our study. The potential cardiac risks in participants infected with Omicron underscore the importance of incorporating more specific cardiac markers, such as troponin, in future studies. This will enhance the monitoring and understanding of cardiovascular health in this population.
The unchanged FEV/FVC ratio observed in our study likely reflects the reversibility of lung function impairment and the milder structural impact of Omicron on lung tissue. Consistent with other studies, Omicron’s effect on lung function appears less severe, with lung function recovering post-infection21,22. While some exudative impairment of the gas-blood barrier was noted23, it does not seem sufficient to cause significant pulmonary function abnormalities in ventilation phenotypes.
VCL pathway central to vascular-alveolar integrity
The current study expands on our previous research12 by employing multi-omics and collaborative validation methods to understand SARS-CoV-2 variants’ pathology, specifically identifying the VCL pathway as a distinctive feature in Omicron infections. This pathway, crucial for lung exudation, was validated as an Omicron-associated biomarker along with ICAM1. These findings not only complement prior studies but also enhance the robustness of our conclusions. Rat model studies further indicated the therapeutic potential of targeting VCL, offering the strategic directions for developing therapies against emerging SARS-CoV-2 variants. While the previous study discovered a number of dysregulated proteins and metabolites12, the current study emphasizes the specific mechanisms and therapeutic potential of the VCL pathway, while also comparing the similarities and differences between Omicron and the original variant. This study highlights the critical role of the VCL pathway in maintaining vascular-alveolar integrity, offering insights into its mechanism and potential therapeutic targets for drug development in treating COVID-19 and similar respiratory diseases.
Our findings underscore the VCL pathway’s pivotal role in promoting vascular-alveolar leakage, impacting gas exchange, and manifesting radiological signs of exudation (Fig. 8). The VCL pathway in ancestral variant infections are also strongly correlated with inflammation markers such as CRP, PCT, and SAA. SAA is an acute-phase protein primarily synthesized by the liver in response to pro-inflammatory cytokines. It has been identified by Pieri et al. as a valuable biomarker for predicting the severity and prognosis of COVID-1924. Building on this, our study presents evidence that VCL is positively associated with SAA. In symptomatic participants infected with Omicron and ancestral variant SARS-CoV-2, the high correlation between SAA and VCL suggests that SAA plays a significant role in the inflammatory response and disease progression. The elevated levels of SAA in these participants are indicative of a heightened inflammatory state, which aligns with the upregulation of VCL and its increased N-glycosylation. This upregulation could enhance cell adhesion and migration processes critical during inflammation and immune responses, underscoring the importance of SAA as a marker for disease severity. In contrast, the lower correlation between SAA and VCL in asymptomatic participants infected with Omicron suggest a different inflammatory and immune response dynamic. In these cases, the body may effectively control the virus without triggering a high inflammatory state, reflected in lower SAA levels. This indicates that the levels of SAA and the modification state of VCL can reflect the disease’s severity and progression.
VE-cadherin Vascular endothelial-cadherin, CC Calcium-calmodulin complex, α-cat α-Catenin, TCA Tricarboxylic acid cycle, ATP Adenosine triphosphate, ICAM-1 Intercellular adhesion molecule-1, PMN Polymorphonuclear neutrophils, HBP Heparin binding protein, VCL Vinculin, F-actin Filamentous actin, N-gly N-glycan, DPPC Dipalmitoyl phosphatidylcholine. Created in BioRender. Xue, M. (2025) https://BioRender.com/c69j935.
Elevated ICAM-1 levels trigger a cascade of events including enhanced adhesion effects, PMNs activation, HBP release, and cytoskeletal remodeling, leading to increased vascular leakage. Inflammation also affects vascular endothelium and ACT cell cytoskeleton, potentially contributing to elevated ACT content in participants infected with ancestral variant. Conversely, even in seemingly “mild” Omicron infections, the VCL/ICAM-1 pathway shows significant differences compared to healthy individuals, with a trend of elevation from asymptomatic to symptomatic cases. The correlation between this pathway and disease characteristics is not linear, suggesting that an increase in VCL/ICAM-1 does not necessarily disrupt the blood-gas barrier. Research has proposed infection-related inflammation score thresholds to determine the relationship between indicators and disease presentation. Surpassing this threshold may increase the risk of disease exacerbation25,26,27,28. This pathway’s alteration in response to inflammation suggests a potential target for modulating disease severity, especially noted in the differential activation between ancestral variant SARS-CoV-2 and the Omicron variant infections.
Research indicates that endothelial cells are the primary sites where the blood-gas barrier induces pulmonary exudation, and most endothelial adhesion molecules undergo significant N-glycosylation modifications29,30. During inflammation, endothelial cell dysfunction leads to significant alterations in N-glycosylation processing mechanisms and surface N-glycan content31. The results of this study demonstrate a significant increase in N-glycosylation levels corresponding to VCL, thereby validating this perspective. For effective leukocyte adhesion to occur, VCL must bind with N-glycans. Therefore, the elevation of VCL N-glycosylation levels further illustrates the dynamic activation of the VCL pathway within participants infected with Omicron. N-glycans influence leukocyte migration and endothelial cell morphological changes by affecting intercellular adhesion and binding to the actin cytoskeleton32. Our study indicates that during Omicron infection, the N-glycosylation level of VCL significantly increases. This heightened N-glycosylation may affect cell adhesion and the binding of VCL to the actin cytoskeleton, impacting overall cytoskeletal stability and indirectly influencing the interaction between the virus and host cells, contributing to the host’s pathogenic state. The increased N-glycosylation of VCL can modulate host cell immune responses to Omicron infection by affecting signaling pathways, influencing cytokine production, and recruiting inflammatory factors. Furthermore, this study found a significant decrease in N-glycosylation of ICAM-1, which is associated with adhesion function. Research indicates that highly glycosylated ICAM-1 plays a critical role in innate immune responses, and reduced N-glycosylation may lead to recurrent infections in participants33. Alpha-mannosidase, a key enzyme in N-glycosylation, can reduce N-glycan expression and enhance cell adhesion function when inhibited34, potentially offering the avenues for COVID-19 treatment. While no literature explicitly details the synergistic effects of N-glycosylation of VCL and ICAM-1 during Omicron infection, it is established that VCL maintains cytoskeletal stability, and ICAM-1 may influence cytoskeletal dynamics35. During Omicron infection, altered N-glycosylation of ICAM-1 could affect its interaction with VCL, impacting cytoskeletal stability and virus-host cell interactions. This study has focused on fixed modifications of glycosylation sites without investigating the variable glycan structures. As a limitation of this study, we recognize that studying the detailed structural variations of glycans would enhance our understanding of the full biological and functional diversity of N-glycosylation related to COVID-19.
VCL’s influence on cytoskeletal remodeling, demonstrated by associated changes in ACTN-ACTB1 (Actin N-B1) levels, emphasizes its role in modulating the inflammatory response and cell migration. Cytoskeletal rearrangement and intercellular gap regulation in vascular endothelial cells facilitate inflammation diffusion30. ACT is crucial for cell junctions and cell polarity maintenance36,37. VCL plays a significant role in driving inflammatory cell chemotaxis in participants infected with SARS-CoV-2, not only by coordinating the cytoskeleton but also by promoting the outward migration of white blood cells38. The VCL pathway coordinates the cytoskeleton, promotes white blood cell migration, and qPCR mRNA sequence analysis confirms increased VCL expression. The VCL/ICAM-1 pathway is a critical mechanism in inflammatory exudation and blood-gas barrier injury, possibly relevant to exudative pericardial effusion in participants infected with SARS-CoV-239.
VCL and ICAM-1 are crucial for cellular structural stability, signal transduction, and inflammatory response40. The permeability of the normal blood-gas barrier depends on stable adhesions at actin protrusion structures in cell-cell junctions. The VCL/ICAM-1 pathway plays a central role in inflammation-adhesion-exudation, involving critical cytoskeletal remodeling41. VCL’s involvement in maintaining the structural integrity of cells is crucial for understanding how SARS-CoV-2, including the Omicron variant, affects cellular interactions and stability. The dysregulation of VCL might contribute to the observed abnormalities in inflammation and coagulation pathways, particularly in extrapulmonary tissues. High tension mediated by VCL disrupts continuous linear adherens junctions42, leading to the formation of discontinuous focal adherens junctions, increasing endothelial permeability. Tension-induced desmin helps protect these junctions43. VCL is observed at higher levels in lung injury tissue but doesn’t extravasate into the alveolar cavity, emphasizing its role as a structural component of the blood-gas barrier. Electron microscopy reveals various signs of blood-gas barrier dysfunction, with radiographic manifestations reflecting structural damage due to inflammation-adhesion-exudation. The significant increase in ICAM-1 and HBP further supports the VCL/ICAM-1 pathway’s role in mediating the inflammatory exudation effect. Blocking the VCL pathway with anti-Vinculin antibodies in a lung injury model improves lung exudation and barrier damage in rats, offering a potential therapeutic intervention. However, while anti-VCL intervention shows promise in reducing pulmonary exudation and promoting lung recovery, its long-term inhibition could increase cellular structural vulnerability and negatively impact lung tissue stability. VCL’s role in maintaining mechanical stability and stress transmission suggests that its suppression might impair cell adhesion, tissue repair, and regeneration. Therefore, comprehensive studies and clinical trials are necessary to ensure a careful assessment of the potential benefits and risks of anti-VCL therapies.
ICAM-1 is crucial for the migration and aggregation of inflammatory cells44. Its activation is closely related to increased numbers of inflammatory cells and elevated levels of inflammatory markers. In our study, the activation status of ICAM-1 correlated significantly with inflammation-related lung injury, supporting its key role in the inflammatory response and lung damage. By mediating the recruitment of leukocytes to sites of inflammation, ICAM-1 contributes to the progression of inflammatory damage in the lungs. In the context of Omicron and ancestral variant infections, differences in ICAM-1 expression may underline the distinctive inflammatory responses observed. Omicron’s milder symptoms and reduced inflammation could correlate with lower ICAM-1 expression levels compared to the ancestral variant, which exhibits more pronounced inflammatory and coagulation abnormalities.
The correlation between ICAM-1 and VCL in asymptomatic and symptomatic SARS-CoV-2 infections exhibits distinct expression patterns, as illustrated in this study. In asymptomatic participants infected Omicron, both ICAM-1 and VCL levels are low, suggesting a mild immune response that maintains the stability of the vaso-alveolar barrier without severe symptoms. This likely indicates effective viral defense without excessive inflammation. The negative correlation between these markers in asymptomatic cases possibly reflects a balanced, non-inflammatory immune state where cell structure maintenance is prioritized over immune cell recruitment. In contrast, symptomatic participants infected with the ancestral variant SARS-CoV-2 exhibit significantly elevated levels of ICAM-1 and VCL. This indicates a strong immune response involving immune cell recruitment and cytoskeletal remodeling. While this intense response aims at pathogen clearance and tissue repair, it can also lead to tissue damage, vascular leakage, and pulmonary edema. The positive correlation in symptomatic participants reflect a coordinated response where the body actively recruits immune cells and restructures the cytoskeleton to combat the infection and facilitate tissue repair. Our findings about VCL and ICAM-1, along with their correlation with clinical data, provide insights into the molecular mechanisms underlying the clinical differences between Omicron and ancestral variant SARS-CoV-2 infections. Understanding these pathways can help guide targeted therapeutic strategies for future SARS-CoV-2 variants.
SARS-CoV-2’s impact on energy pathways
Our metabolomics analysis unveils a disruption in the TCA-glycolysis equilibrium due to SARS-CoV-2 infection, a pathway powering cellular activities, including cytoskeletal remodeling. This disruption manifests differently across variants: while ancestral variant infection triggers increase in both TCA cycle and glycolysis metabolites such as lactate and pyruvate, Omicron infection predominantly elevates TCA cycle activity, reflecting milder blood-gas barrier impairment and a modulated metabolic response. Intriguingly, both groups exhibit shows a significant increase in LDH, linked to hypoxia and tissue damage. Metabolites reflecting pro-inflammatory and anti-inflammatory balance, such as ARA, HETE, and DHA, display a pro-inflammatory tendency in both ancestral and Omicron groups. Asymptomatic participants infected with Omicron also exhibit elevated levels of inflammatory metabolites. Phosphorus metabolism pathway results suggest a connection between ACT-VCL-mediated cytoskeletal activity and lipid membrane stability in an inflammatory environment. This indicates distinct impacts of Omicron and ancestral variant infections on energy supply pathways and their effects on ATP-dependent cytoskeletal remodeling by ACT-VCL. This original insight not only enhances our understanding of the metabolic underpinnings of SARS-CoV-2 infections of different variants, but also opens the avenues for targeted therapeutic interventions aimed at restoring metabolic balance and preserving respiratory health in the face of evolving viral threats.
In conclusion, this comprehensive study, harnessing the power of proteomics and metabolomics, provides unprecedented insights into the impact of SARS-CoV-2 variants (ancestral and Omicron) on human physiology, enhancing significantly our understanding of the disease’s mechanisms. Unlike published GWASs that primarily emphasize host immunity and infection susceptibility in COVID-1945,46, our omics research unveils groundbreaking insights into the evolving physiological impacts induced by the Omicron variant through the VCL pathway. By elucidating these intricate mechanisms, our study significantly deepens our understanding of COVID-19’s multifaceted pathogenesis, discerning nuanced differences between symptomatic and asymptomatic participants infected with various viral variants. Notably, our findings highlight the central role of the VCL/ICAM-1 pathway, signaling a paradigm shift in our approach to combating the inflammatory and exudative challenges posed by COVID-19 at the pulmonary interface. These insights hold promise for the development of therapeutic interventions, potentially revolutionizing the management of respiratory inflammation and barrier integrity amidst the evolving landscape of viral threats. In essence, our findings mark a significant step forward in advancing our understanding of COVID-19 and offer hope for more resilient and proactive approaches to mitigating its impact on global health. The findings from this study suggest significant implications for refining clinical management and monitoring strategies for participants infected with Omicron. The identification of VCL and ICAM-1 as biomarkers associated with Omicron allows for more precise patient monitoring and tailored treatment plans. Clinicians can use these biomarkers to better assess disease progression and intervene early, potentially reducing the burden on healthcare systems. Comprehensive metabolomic analysis underscores the need for extensive monitoring of participants’ physiological status, potentially requiring additional tests beyond those used for earlier variants. This may warrant updating treatment protocols to include regular monitoring of these biomarkers and other metabolic indicators affected by Omicron. By highlighting the specific risks associated with Omicron and the importance of monitoring key biomarkers, public health authorities can educate healthcare providers and the general public about the need for vigilance and appropriate care strategies.
Methods
Study participants
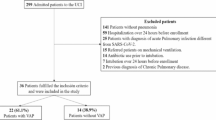
For this omics study, we involved two variant groups, which included 40 participants infected with Omicron BA.2.76 and 20 participants infected with ancestral variant from Guangzhou Medical University Affiliated First Hospital. Ancestral variant samples were collected from the first infected strains of SARS-CoV-2, defined as the Ancestral variant, in China from December 2019 to May 2020, while BA.2.76 samples were obtained during the wave of August to September 2022. Due to limited sequencing availability, identification relied on the temporal context of the initial outbreak3,47,48. All samples were from patients with primary SARS-CoV-2 infections. All participants are Chinese from China, and received a primary diagnosis based on a positive nucleic acid test via pharyngeal swab samples, following the most recent COVID-19 Omicron diagnosis and treatment guidelines, as well as the 2020 SARS-CoV-2 diagnosis and treatment guidelines for ancestral variant infections. Among the 40 participants infected with Omicron BA.2.76, those who tested positive for nucleic acid but displayed no pulmonary symptoms and only mild, self-limiting symptoms such as cough and chest tightness were categorized as the asymptomatic infection group (n = 20). Participants who tested positive for nucleic acid and exhibited related symptoms were classified as the symptomatic infection group (n = 20). Participants infected with the ancestral variant were included in the ancestral group. We collected basic information, radiological data, and clinical test results for all participants. Additionally, a control group consisting of 20 healthy participants, matched for gender and age, provided basic information. Furthermore, we incorporated a validation cohort consisting of 20 symptomatic participants infected with the Omicron variant, matched for key population characteristics (including age, sex, and comorbidities), and 15 healthy participants. This cohort was served to verify identified biomarker trends in the project through secondary testing. To ensure the validity of participant selection, we implemented a comprehensive multi-step screening process, which included structured questionnaire-based screening, electronic medical record (EMR) reviews, and verification through national vaccination records. For further details, refer to Supplementary Methods 1: Participant Selection and Vaccination Status Verification. Written informed consent was obtained from all participants, and approval was granted by the Ethics Committee of Guangzhou Medical University Affiliated First Hospital (Ethics Numbers: 2020-No.44 and 2021-No.31).
To systematically describe the molecular and cellular characteristics within the peripheral blood of participants experiencing breakthrough SARS-CoV-2 infections, we conducted multi-omics analyses encompassing various blood components at different disease stages. This comprehensive approach included (1) clinical assessments, such as laboratory biochemistry, interferon responses, immune analysis, and viral RNA PCR testing, and (2) omics analyses comprising proteomics, N-glycosylation detection, and metabolomics. In essence, we scrutinized numerous samples from participants afflicted by Omicron and ancestral variants of SARS-CoV-2 infections, enabling us to construct extensive molecular and cellular landscapes to explore the connections between key molecular targets and the observed symptoms.
Plasma sample collection and sample storage
Venous blood samples were collected from participants immediately upon hospital admission following disease onset and confirmation by etiological testing. Samples were collected using vacuum blood collection tubes containing anticoagulants such as EDTA or heparin. The tubes were gently inverted to thoroughly mix the blood with the anticoagulant and prevent coagulation. The samples were then centrifuged at 1500–2000 g for 10–15 minutes.
The yellow, transparent plasma layer was carefully extracted using a pipette, ensuring no disturbance to the lower cellular components. The extracted plasma was then transferred to new centrifuge tubes or Eppendorf tubes and immediately stored at −80 °C to maintain sample quality. The interval between sample collection and the initiation of protein extraction was one week, during which all samples remained stored at −80 °C.
Proteomics analysis
We conducted proteomic analysis on plasma from a model cohort of 20 asymptomatic participants infected with Omicron, 20 symptomatic participants infected with Omicron, 20 participants infected with ancestral variant, and 20 healthy controls, followed by proteomic analysis of plasma from a validation cohort of 20 symptomatic participants infected with Omicron and 15 healthy controls. Peptides dissolved in LC mobile phase A are separated using an EASY-nLC 1200 UHPLC system. Mobile phase A consists of 0.1% formic acid and 2% acetonitrile in water, while mobile phase B consists of 0.1% formic acid and 90% acetonitrile in water. The gradient settings are: 0–16 minutes, 7–20% B; 16–24 minutes, 20–32% B; 24–27 minutes, 32–80% B; 27–30 minutes, 80% B, with a flow rate of 500 nL/min. Peptides are separated by the UHPLC system and ionized in the NSI source, then analyzed by the Orbitrap Exploris™ 480 mass spectrometer (ThermoFisher Scientific). The ion source voltage is set to 2.3 kV, FAIMS compensation voltage (CV) to −45 V and −70 V, with both precursor and fragment ions detected by the Orbitrap Exploris™ 480 mass spectrometer (ThermoFisher Scientific). The MS1 scan range is 390–810 m/z with a resolution of 30,000; the MS2 scan range starts at 200 m/z with a resolution of 30,000. Spectronaut (v 16.0) was used for analyzing proteomics data acquired in Data-dependent Acquisition (DDA) mode, where multiple consecutive m/z windows of peptide ions enter the HCD collision cell with collision energies of 25, 30, and 35 for fragmentation, followed by MS2 analysis. AGC is set to 300% and maximum injection time to Auto to enhance mass spectrometer efficiency. For detailed protocols, refer to Supplementary Methods 2 Proteomics Analysis. The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE49 partner repository with the dataset identifier PXD054443.
Metabolomics analysis
We conducted metabolomics analysis on plasma from 20 asymptomatic participants infected with Omicron, 20 symptomatic participants infected with Omicron, 20 participants infected with ancestral variant, and 20 healthy controls. Metabolomics analysis was conducted using 4D untargeted techniques. The Waters ACQUITY UPLC ultra-high-performance liquid chromatography system was employed for omics detection, coupled with a Waters ACQUITY UPLC BEH C18 Column (1.7 µm, 2.1 mm × 100 mm). The chromatography settings included an injection volume of 10 µL, an elution flow rate of 400 µL/min, and a column temperature maintained at 40 °C. For mass spectrometry, MetaboScape 2022 was used to process the raw data, including peak extraction, alignment, and retention time correction. Both primary and secondary mass errors were controlled within 20 ppm to ensure the high accuracy of identification results. Metabolite structures and annotations were derived through spectral matching against several databases, including NIST, HMDB, proprietary databases, and integrated public databases. Quality control measures included the use of internal standards and pooled samples to ensure consistent performance across runs. For a comprehensive description of the procedures and data processing steps, please refer to Supplementary Methods 3 4D Untargeted Metabolomics Study.
Protein N-glycosylation
Tryptic peptides were reconstituted in a wash solution (80% ACN, 5% TFA) after resuspension and loaded onto the chromatography column. The peptides underwent three washes with the wash solution. Glycopeptides were subsequently eluted twice using a mixture of 0.1% TFA, 50 mM ammonium bicarbonate, and 50% ACN. Following elution, the glycopeptides were dehydrated in a SpeedVac and reconstituted in H218O with 50 μL of 50 mM ammonium bicarbonate solution. Then 2 μL of PNGase F glycosidase was added, followed by an overnight digestion at 37 °C. The deglycosylated peptides were ultimately desalted using C18 Zip Tips according to the manufacturer’s guidelines, followed by drying for subsequent MS analysis. Glycopeptides were enriched using hydrophilic interaction liquid chromatography (HILIC) microcolumns. Nonspecific deamidation was included as a variable modification during the database search to account for the artifactual deamidation observed with PNGase F enzyme treatment in heavy water. The data were analyzed using MaxQuant version 1.6.15.0. The quantification of glycoproteins was normalized using proteomics data. To determine glycosylation sites, we compared proteomic data from PNGase F-treated and untreated samples. Peptides present in the treated sample but absent in the untreated sample, showing the specific mass shift indicative of asparagine to aspartic acid conversion, were inferred to be glycosylated. For detailed protocols, refer to Supplementary Methods 4 Protein N-Glycosylation Study.
qPCR analysis
1. An initial step at 50 °C for 2 minutes. 2. Pre-processing: the temperature was raised to 95 °C for 10 minutes to denature DNA. 3. Denaturation and annealing: 15 seconds of denaturation at 95 °C, followed by 1 minute of annealing at 60 °C to facilitate primer binding to the target DNA. 4. Melting curve analysis: Three steps of melting curve analysis were executed, including 15 seconds at 95 °C, 15 seconds at 60 °C, and a final step at 95 °C.
VCL:
Forward Primer: 5’- AGCAGGACCCAGGAGTTTATG – 3’
Reverse Primer: 5’- TGTGGCACTGAGAGGAGTTAG – 3’
ICAM-1:
Forward Primer:5’- CGGTGTGGAACCTGAGGA – 3’
Reverse Primer:5’- CAGGTCAGCTCCAGAAAGG – 3’
Validation and analysis of the lung injury rat model
In this study, an acute rat lung injury model experiment was established (Fig. 7A) to further validate the target protein model which identified in Omics analysis progress. This model was developed based on the tissue modeling analysis used by Raviv et al.50 and Yang et al.51 for studying lung injury caused by ARDS. Additionally, it incorporated findings from Parhiz et al.52, Niu et al.53, and Bombaci et al.54 regarding interventions for COVID-19 lung injury. Male outbred Sprague-Dawley (SD) rats, aged 8-10 weeks, were used in this experiment to minimize potential variability related to the estrous cycle. These outbred rats were sourced from [Guangzhou Ruige Biological Technology Co., Ltd]. The rats were housed in a temperature-controlled environment, maintained at 22 ± 2 °C with a relative humidity of 50 ± 10%. The animals were kept under a 12-hour light/dark cycle, with the lights on from 7:00 AM to 7:00 PM. Each rat was housed in individual cages, with a maximum of 3 animals per cage to avoid overcrowding. The cages were equipped with appropriate bedding, nesting materials, and enrichment items to support the natural behavior of the rats. Food and water were provided ad libitum. To maintain cleanliness and prevent contamination, the cages were cleaned weekly. Using SD rats, including 10 healthy rats as controls receiving saline treatment and 20 lung injury model rats (10 receiving Anti-VCL intervention, 10 not). Lipopolysaccharide (LPS), purchased from Sigma-Aldrich (USA), was used to induce lung injury at a dosage of 5 mg/kg body weight, administered via nasal route as a single dose. Full-length vinculin protein (Thermo Fisher Scientific, USA) was utilized as an intervention reagent at a concentration of 1.2 mg/mL. It was administered to rats via the nasal route at a total volume of 50 µL/day for one week. The animal experimental protocol was approved by the Animal Welfare Ethics Committee of Zunyi Medical University (Ethics Numbers: ZMU21-2303-285).
For further validation of the lung injury model, histopathological analysis was conducted using Hematoxylin and Eosin (HE) staining to assess the extent of tissue damage and inflammatory response. Following the experimental protocol, rats were euthanized at designated time points post-treatment, and lung tissues were harvested. The tissues were immediately fixed in 4% paraformaldehyde at 4 °C for 24 hours. After fixation, the tissues were embedded in paraffin, and 4 µm thick sections were prepared. The sections were deparaffinized in xylene and rehydrated through a graded alcohol series. To perform HE staining, the tissue sections were first stained with hematoxylin for 5 minutes to visualize the nuclei, followed by eosin staining for 3 minutes to highlight the cytoplasm and extracellular matrix. After staining, the sections were dehydrated, cleared in xylene, and mounted with neutral balsam. The stained sections were observed under a light microscope (Olympus, Japan).
Immunofluorescence staining was used to examine the expression of key proteins involved in lung injury, including vinculin, to validate the target protein identified in the omics analysis. Lung tissue sections were prepared as described above, and antigen retrieval was performed by heating the slides in a citrate buffer (pH 6.0) for 20 minutes at 95 °C. After cooling, the sections were permeabilized with 0.1% Triton X-100 for 10 minutes and blocked with 5% bovine serum albumin (BSA) in phosphate-buffered saline (PBS) for 1 hour at room temperature. Primary antibodies targeting vinculin (Thermo Fisher Scientific, USA, 1:200 dilution) and other relevant proteins were incubated overnight at 4 °C. After washing with PBS, the sections were incubated with appropriate fluorescent secondary antibodies (Alexa Fluor 488 or 594, 1:500 dilution, Invitrogen, USA) for 1 hour at room temperature. Nuclei were stained with DAPI (Sigma-Aldrich, USA) for 5 minutes. The sections were then mounted with fluorescence mounting medium and imaged using a confocal microscope (Leica, Germany). The fluorescence intensity and localization of the target proteins were analyzed using image analysis software (ImageJ v1.54i), and representative images were selected for comparison across groups.
Scanning electron microscopy (SEM)
High-precision scanning of animal lung tissue, with a particular focus on the structure of the pulmonary alveolar epithelial blood-gas barrier, was conducted using Transmission Electron Microscopy (TEM), specifically Tecnai G2 Spirit 120 kV TEM.
Protein fluorescence
GFP (Green Fluorescent Protein) and BFP (Blue Fluorescent Protein) fluorescent tags were incorporated into target protein antibodies in this study. The chosen fluorescent dyes or labels reacted with the protein sample, covalently attaching the protein to the fluorescent dye. After the reaction, the mixture was washed to eliminate unbound fluorescent dye, thereby reducing background signal. The fluorescence signal of the protein was detected and localized using the fluorescence microscope and spectrometer, facilitating the detection and localization of highly specific protein complexes within the tissue.
Statistical methods
Orthogonal partial least squares discriminant analysis (OPLS-DA) was adapted as a supervised model to assess metabolic changes among different groups. The Variable Importance in Projection (VIP) score for each metabolite within the projection was computed. Permutation test was used to assess the risk of overfitting the OPLS-DA model. Differences between two groups were compared using Student’s t-test and fold change (FC). Metabolites meeting the criteria of P < 0.05, VIP > 1, and FC > 2 were deemed statistically significant. In cases involving more than three groups, analysis of variance (ANOVA) was performed by default. Subsequently, pathway enrichment analysis of these differentially expressed metabolites was performed using the KEGG database to identify significantly enriched trends in specific pathways. Fisher’s exact test was used to calculate enrichment p-values. Lastly, differential metabolites were annotated using the Human Metabolome Database (HMDB), and disease-related information pertaining to differential metabolites was identified based on the KEGG and HMDB databases.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The proteomics and glycoproteomics data have been deposited in ProteomeXchange (Submission reference: PXD054443) and The Metabolomics data have been deposited in MetaboLights (Submission reference: MTBLS12231). Supporting source data used in the generation of figures and results are provided with this paper. Source data are provided with this paper.
References
Zhou, P. et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273 (2020).
Lu, Y. et al. Recombinant protein HR212 targeting heptad repeat 2 domain in spike protein S2 subunit elicits broad-spectrum neutralizing antibodies against SARS-CoV-2 and its variants. MedComm 6, e70088 (2025).
Du, P. et al. Genomic surveillance of COVID-19 cases in Beijing. Nat. Commun. 11, 5503 (2020).
Fan, Y. et al. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal Transduct. Target Ther. 7, 141 (2022).
Rani, M., Uniyal, A., Akhilesh & Tiwari, V. Decrypting the cellular and molecular intricacies associated with COVID-19-induced chronic pain. Metab. Brain Dis. 37, 2629–2642 (2022).
Dockrell, D. H., Russell, C. D., McHugh, B. & Fraser, R. Does autonomous macrophage-driven inflammation promote alveolar damage in COVID-19? Eur. Respir. J. 60, 2201521 (2022).
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol 21, 133–146 (2023).
Pan, P. et al. SARS-CoV-2 N protein promotes NLRP3 inflammasome activation to induce hyperinflammation. Nat. Commun. 12, 4664 (2021).
Chang, H. & Li, J. “Lymphocyte * Neutrophil” count decreased in SARS-CoV-2 Omicron patients in Shanghai with no significant change in CRP and SAA. J. Clin. Lab Anal. 36, e24671 (2022).
Suzuki, K., Ichikawa, T., Suzuki, S., Tanino, Y. & Kakinoki, Y. Clinical characteristics of the severe acute respiratory syndrome coronavirus 2 omicron variant compared with the delta variant: a retrospective case-control study of 318 outpatients from a single sight institute in Japan. PeerJ 10, e13762 (2022).
Shrestha, L. B., Foster, C., Rawlinson, W., Tedla, N. & Bull, R. A. Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission. Rev. Med Virol. 32, e2381 (2022).
Yang, Q. et al. Deciphering the omicron variant: integrated omics analysis reveals critical biomarkers and pathophysiological pathways. J. Transl. Med. 22, 219 (2024).
Zhang, J. J., Dong, X., Liu, G. H. & Gao, Y. D. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 64, 90–107 (2023).
Ali, A. M., Tofiq, A. M., Rostam, H. M., Ali, K. M. & Tawfeeq, H. M. Disease severity and efficacy of homologous vaccination among patients infected with SARS-CoV-2 Delta or Omicron VOCs, compared to unvaccinated using main biomarkers. J. Med Virol. 94, 5867–5876 (2022).
Menni, C. et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet 399, 1618–1624 (2022).
Qiu, W. et al. The derived neutrophil to lymphocyte ratio can be the predictor of prognosis for COVID-19 Omicron BA.2 infected patients. Front Immunol. 13, 1065345 (2022).
Sette, A. & Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 184, 861–880 (2021).
Fernandez-de-Las-Penas, C. et al. Long-COVID Symptoms in Individuals Infected with Different SARS-CoV-2 Variants of Concern: A Systematic Review of the Literature. Viruses 14, 2629 (2022).
Liu, H. et al. Clinical characteristics, diagnosis and short-term outcomes of COVID-19-associated acute myocarditis in China. ESC Heart Failure 12, 338–352 (2024).
Nchioua, R. et al. Strong attenuation of SARS-CoV-2 Omicron BA.1 and increased replication of the BA.5 subvariant in human cardiomyocytes. Signal Transduct. Target. Ther. 7, 395 (2022).
Zhang, H. et al. 3-year outcomes of discharged survivors of COVID-19 following the SARS-CoV-2 omicron (B.1.1.529) wave in 2022 in China: a longitudinal cohort study. Lancet Respiratory Med. 12, 55–66 (2024).
Tanneti, N. S. et al. Comparison of SARS-CoV-2 variants of concern in primary human nasal cultures demonstrates Delta as most cytopathic and Omicron as fastest replicating. mBio 15, e0312923 (2024).
Uraki, R. et al. Characterization of SARS-CoV-2 Omicron BA.2.75 clinical isolates. Nat. Commun. 14, 1620 (2023).
Pieri, M. et al. Serum Amyloid A Protein as a useful biomarker to predict COVID-19 patients severity and prognosis. Int Immunopharmacol. 95, 107512 (2021).
Sayah, W. et al. Interleukin-6, procalcitonin and neutrophil-to-lymphocyte ratio: Potential immune-inflammatory parameters to identify severe and fatal forms of COVID-19. Cytokine 141, 155428 (2021).
Jiang, Z. et al. An explainable machine learning algorithm for risk factor analysis of in-hospital mortality in sepsis survivors with ICU readmission. Comput Methods Prog. Biomed. 204, 106040 (2021).
Tirotta, D. et al. Evaluation of the threshold value for the modified early warning score (MEWS) in medical septic patients: a secondary analysis of an Italian multicentric prospective cohort (SNOOPII study). QJM 110, 369–373 (2017).
de Jesus, T. J. & Ramakrishnan, P. NF-kappaB c-Rel Dictates the Inflammatory Threshold by Acting as a Transcriptional Repressor. iScience 23, 100876 (2020).
Radovani, B. & Gudelj, I. N-Glycosylation and Inflammation; the Not-So-Sweet Relation. Front Immunol. 13, 893365 (2022).
Dalal, P. J., Muller, W. A. & Sullivan, D. P. Endothelial Cell Calcium Signaling during Barrier Function and Inflammation. Am. J. Pathol. 190, 535–542 (2020).
Scott, D. W. & Patel, R. P. Endothelial heterogeneity and adhesion molecules N-glycosylation: implications in leukocyte trafficking in inflammation. Glycobiology 23, 622–633 (2013).
Liwosz, A., Lei, T. & Kukuruzinska, M. A. N-glycosylation affects the molecular organization and stability of E-cadherin junctions. J. Biol. Chem. 281, 23138–23149 (2006).
Dai, Y. et al. Association between obesity and sexual maturation in Chinese children: a muticenter study. Int. J. Obes. 38, 1312 (2014).
Qu, L. et al. Inhibition of the alpha-mannosidase Man2c1 gene expression enhances adhesion of Jurkat cells. Cell Res 16, 622–631 (2006).
Comrie, W. A., Li, S., Boyle, S. & Burkhardt, J. K. The dendritic cell cytoskeleton promotes T cell adhesion and activation by constraining ICAM-1 mobility. J. Cell Biol. 208, 457–473 (2015).
Solomon, L. M., Fretzin, D. & Pruzansky, S. Pilosebaceous dysplasia in the oral-facial-digital syndrome. Arch. Dermatol 102, 598–602 (1970).
Ziegler, W. H., Liddington, R. C. & Critchley, D. R. The structure and regulation of vinculin. Trends Cell Biol. 16, 453–460 (2006).
Conroy, L. R., Hawkinson, T. R., Young, L. E. A., Gentry, M. S. & Sun, R. C. Emerging roles of N-linked glycosylation in brain physiology and disorders. Trends Endocrinol. Metab. 32, 980–993 (2021).
Kermani-Alghoraishi, M., Pouramini, A., Kafi, F. & Khosravi, A. Coronavirus Disease 2019 (COVID-19) and Severe Pericardial Effusion: From Pathogenesis to Management: A Case Report Based Systematic Review. Curr. Probl. Cardiol. 47, 100933 (2022).
Barreiro, O. et al. Dynamic interaction of VCAM-1 and ICAM-1 with moesin and ezrin in a novel endothelial docking structure for adherent leukocytes. J. cell Biol. 157, 1233–1245 (2002).
Dorland, Y. L. & Huveneers, S. Cell-cell junctional mechanotransduction in endothelial remodeling. Cell Mol. Life Sci. 74, 279–292 (2017).
Chang, C.-W. & Kumar, S. Vinculin tension distributions of individual stress fibers within cell–matrix adhesions. J. cell Sci. 126, 3021–3030 (2013).
Spörrer, M. et al. The desmin mutation R349P increases contractility and fragility of stem cell‐generated muscle micro‐tissues. Neuropathol. Appl. Neurobiol. 48, e12784 (2022).
Bui, T. M., Wiesolek, H. L. & Sumagin, R. ICAM-1: A master regulator of cellular responses in inflammation, injury resolution, and tumorigenesis. J. Leucoc. Biol. 108, 787–799 (2020).
Pairo-Castineira, E. et al. GWAS and meta-analysis identifies 49 genetic variants underlying critical COVID-19. Nature 617, 764–768 (2023).
Ferreira, L. C., Gomes, C. E. M., Rodrigues-Neto, J. F. & Jeronimo, S. M. B. Genome-wide association studies of COVID-19: Connecting the dots. Infect., Genet. evolution: J. Mol. Epidemiol. Evolut. Genet. Infect. Dis. 106, 105379 (2022).
Feng, Z. et al. Epidemiological features, genomic characteristics, and origin tracing of the COVID-19 outbreaks in Beijing from January to September 2022. J. Med. Virol. 95, e28613 (2023).
Yisimayi, A. et al. Repeated Omicron exposures override ancestral SARS-CoV-2 immune imprinting. Nature 625, 148–156 (2024).
Perez-Riverol, Y. et al. The PRIDE database resources in 2022: a hub for mass spectrometry-based proteomics evidences. Nucleic Acids Res. 50, D543–D552 (2022).
Arber Raviv, S. et al. Lung targeted liposomes for treating ARDS. J. Control Release 346, 421–433 (2022).
Yang, C. et al. Re-Du-Ning injection ameliorates LPS-induced lung injury through inhibiting neutrophil extracellular traps formation. Phytomedicine 90, 153635 (2021).
Parhiz, H. et al. Added to pre-existing inflammation, mRNA-lipid nanoparticles induce inflammation exacerbation (IE). J. Control Release 344, 50–61 (2022).
Niu, Y. et al. Intragastric and atomized administration of canagliflozin inhibit inflammatory cytokine storm in lipopolysaccharide-treated sepsis in mice: A potential COVID-19 treatment. Int Immunopharmacol. 96, 107773 (2021).
Bombaci, G. et al. LRR-protein RNH1 dampens the inflammasome activation and is associated with COVID-19 severity. Life Sci. Alliance 5, e202101226 (2022).
Acknowledgements
This work was supported by Guangdong Zhong Nanshan Medical Foundation (ZNSA-2021005). Guangdong Province Basic and Applied Basic Research Foundation Precision Medicine Joint Foundation (2021B1515230008). Exploration and Optimization of Early Intervention Strategies and Timing for High-Risk Individuals at Risk of Severe Illness/Death (2022YFC2304803). Enhancing the Treatment and Outcome of COVID-19 Infections through the Use of Medical Consortiums as a Vehicle (ZHYG202339). National Natural Science Foundation of China (No. 82302607), Guangdong Basic and Applied Basic Research Foundation (2022A1515110555). We were grateful to Jingjie PTM BioLab (Hangzhou), Co. Ltd. and Guangzhou YuanGuJi Technology Co.,Ltd. for its technical support. Figures 6h, 7a, 7i-l, 8, S1a created with BioRender.com, with permission.
Author information
Authors and Affiliations
Contributions
These authors contributed equally to this work: M.X., Z.L., Y.W. Conception and design of the research: B.S., X.T., H.W., and Z.D. Drafting the manuscript: M.X. and Z.L. Manuscript Editing: H.Q., H.Ha. Article structure design: M.X. and Z.L. Statistical analysis: Z.L., Q.H., S.F. and Y.L. Samples collection and detection: Y.L., F.H., L.L., H.Hu., P.Z., N.L., and Q.Yu. Experimental management: J.C., C.J., P.L., M.Z., X.Z., X.W., and Q.W. Acquisition of data: Q.G., L.S., X.Z., S.F. and Y.L. Data Interpretation: M.X., Z.L., Q.Ya., J.C., H.Q., H.Ha. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xue, M., Lin, Z., Wen, Y. et al. VCL/ICAM-1 pathway is associated with lung inflammatory damage in SARS-CoV-2 Omicron infection. Nat Commun 16, 3801 (2025). https://doi.org/10.1038/s41467-025-59145-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-59145-y