Abstract
Up to 25% of patients with ALK-rearranged non-small cell lung cancer (NSCLC) experience disease progression within the first year of targeted therapy. This phase 2 trial investigates whether combining alectinib with bevacizumab can delay resistance mechanisms in advanced ALK-rearranged NSCLC. ALEK-B was an open-label, single-arm, single-center phase 2 trial (NCT03779191) evaluating alectinib (600 mg BID) and bevacizumab (15 mg/kg) in patients with advanced ALK-rearranged NSCLC confirmed by next-generation sequencing. The primary endpoint was the 12-month progression-free survival (PFS). Secondary endpoints included overall survival (OS), objective response rate (ORR), intracranial progression-free survival (icPFS), safety, and patient-reported quality of life (QoL). Between April 2020 and August 2022, 41 patients were enrolled, including 17.1% with brain metastases. As of December 14, 2023, with a median follow-up of 34.5 months, the 12-month PFS rate was 97.1% (95% CI 92.6–100). The 36-month PFS and OS rates were 64.2% (95% CI 56.1–85.2) and 87.9% (95% CI 74–96.6), respectively. The ORR was 100%, and the 36-month icPFS rate was 87.8% (95% CI 74.0–96.6). Grade 3–4 adverse events occurred in 46.3% of patients, most commonly proteinuria and hepatotoxicity, with no fatal events reported. QoL significantly improved from baseline at 12 months and was maintained through 36 months. These findings support the efficacy and safety of alectinib plus bevacizumab and justify further investigation in ALK-rearranged NSCLC.
Similar content being viewed by others
Introduction
Anaplastic lymphoma kinase (ALK) rearrangements drive 3–9% of non–small cell lung cancers (NSCLC)1,2. ALK oncoproteins promote cell survival and growth through aberrant activation of intracellular signaling, including the PI3K/AKT/mTOR and RAS/Raf/MEK/ERK pathways3. NSCLC cancers harboring ALK rearrangements (ALK-positive) are highly sensitive to ALK-tyrosine kinase inhibitors (ALK-TKIs), which can induce apoptosis. In the last decade, the development of ALK-TKIs has significantly improved the survival outcomes of patients with ALK-positive NSCLC. Next-generation ALK-TKIs have become the standard first-line treatment option for patients with advanced ALK-positive NSCLC because of their greater potency, selectivity, and central nervous system (CNS) penetration compared to crizotinib.
Alectinib, a second-generation ALK-TKI, has demonstrated a prolonged progression-free survival (PFS) compared to crizotinib. Initial results from the ALEX trial reported a 12-month PFS of 68.4% for alectinib versus 48.7% for crizotinib4. The median PFS, as assessed by independent review, was 25.7 months for alectinib compared to 10.4 months for crizotinib4. The median PFS assessed by independent review was of 25.7 months versus 10.4 months. However, despite the initial efficacy of ALK-TKIs, the development of drug resistance and subsequent disease progression inevitably occur5, with the CNS being a common site of relapse. Therefore, exploring biologically synergistic combinations to enhance efficacy and overcome resistance to ALK-TKIs is a crucial goal in translational research.
Vascular endothelial growth factor (VEGF) plays a crucial role in promoting primary tumor growth, and metastasis in NSCLC6. Bevacizumab, a recombinant, humanized, anti-VEGF monoclonal antibody, has shown efficacy in combination with platinum chemotherapy for advanced non-squamous NSCLC7. Recently, the combination of epidermal growth factor receptor TKIs plus antiangiogenic monoclonal antibodies has overcome acquired resistance to and improve PFS among this subset of patients8,9,10, especially for those with co-mutations such as TP5311.
Based on preclinical findings, the dual blockade of ALK and VEGF signaling enhances antitumor effects and overcomes resistance by preventing the activation of MAPK, PI3K/AKT, and hypoxia pathways12,13. In a phase I/II study, the combination of alectinib and bevacizumab demonstrated safety in patients with advanced ALK-positive NSCLC, including those with baseline brain metastases (BM)14. Given the promising safety and tolerability of this combination, we designed a phase II trial to evaluate its clinical efficacy. In January 2022, the first reported outcomes, with a median follow-up of 15.6 months, indicated a 12-month PFS rate of 97.1% (95% CI 91–99)15.
Here, we present the updated efficacy and safety analysis at 36-month follow-up, representing, to-the-best-of-our-knowledge, the largest and longest trial testing this combination therapy.
Results
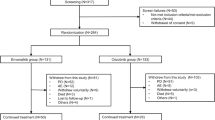
Between April 2020 and August 2022, 54 patients were comprehensively assessed in this one-arm clinical trial. Of these, 41 individuals were specifically allocated to the intervention group. (Fig. 1). The median age of this cohort was 50.0 (43.5–62.0) with a predominant representation of females accounting for 56.1% of the participants. Most subjects (80.4%) exhibited an ECOG PS of 0–1, and all patients had clinical stage IV. Histological examination confirmed a non-squamous histology in 41 patients, with the prevailing subtype being predominant solid lung adenocarcinoma (41.5%).
BM were identified at the time of diagnosis in seven (17%) patients. Among the thirty-three patients with complete molecular data, the EML4-ALK rearrangement emerged as the most prevalent fusion partner (70.8%). Variants 1 and 3 constituted the majority, accounting for 48.3% (n = 14) and 31.0% (n = 9), respectively. Concurrent alterations to ALK rearrangement were observed in twenty-one patients (63.6%), with a median of one co-alteration per patient. The most common co-mutations included the homozygous loss of CDKN2A/B (12.1%) and TP53 mutations (12.1%). Baseline patient characteristics are shown in Table 1.
Progression-free survival and overall survival
As of the data cutoff on December 14, 2023, the median follow-up duration was 34.5 months (95% CI 32.1–36.8). The PFS rates at 12 and 36 months for the entire population were 97.1% (95% CI 92.6–100) and 64.2% (95% CI 56.1–85.2), respectively (Fig. 2A). Previous studies have linked the EML4-ALK variant 3 to poorer survival outcomes. Among 27 patients with known EML4-ALK variant types, the median PFS was non-estimable for both, variant 3 (95% CI 30.4-NR) and other variants (n = 18; 95% CI 28.9-NR). The 12 and 36-month PFS rates were 100% and 55.6% (95% CI 15.0–96.0) for variant 3 (n = 9), and 100% and 59.8% (95% CI 49.3–95.1) for other variants (n = 18), respectively. Univariate analysis revealed no significant association between clinical characteristics and increased risk of disease progression (Supplementary Table 1).
Efficacy outcomes in patients with ALK-rearranged NSCLC who received upfront alectinib plus bevacizumab A Progression free survival with 95% Confidence Interval B Overall survival C Swimmer plot of the trial sample (n = 41), showing the time and type of response, duration of response (DOR), time on the experimental therapy, time without bevacizumab, number of progressive diseases, persistent adverse events, and ongoing treatment, according to the main baseline and molecular characteristics.
Out of the 41 patients, four died during a median follow-up of 37.3 months (95% CI 32.5–42.1) and 6 were deceased by the DCO. The 12 and 36-month OS rates of 100% and 87.9% (95% CI 74.0–96.6), respectively, as shown in Fig. 2B. Duration of response (DoR), response types, and other events are depicted in Fig. 2C.
Overall response rate, duration of response, and time on treatment
Among the 41 evaluated patients, the overall response rate (ORR) was 100%. Specifically, 36 patients (87.8%) achieved a partial response, while five patients (12.2%) experienced a complete response based on RECIST v1.1 criteria. The median time to response was 1.34 months (1.31–2.39), with a median time to best overall response (BoR) of 13.7 months (95% CI: 8.6–18.9) (Supplementary Table 2). The 36-month DoR rate was 62.6% (95% CI: 56.1–85.2) (Fig. 3A). The median maximum reduction in tumor size from baseline was −84.9% (−67.2 – −93.0) Collectively, these results highlight a substantial and durable response in the majority of patients (Fig. 3B).
CNS efficacy analysis
The cumulative incidence of brain metastases was 8.8% (95% CI: 7.2–9.7) after a median follow-up of 34.4 months, with a median of 1.8 new brain lesions observed per patient (Fig. 4A). At baseline, seven patients (17.1%) presented with brain metastases, with a median of five lesions (range: 1–6). Of these, six patients were neurologically asymptomatic, while one symptomatic patient underwent whole-brain radiotherapy (WBRT) at diagnosis. The median follow-up for detecting CNS progression was 33.1 months (95% CI: 28.5–37.7). The 36-month intracranial progression-free survival (icPFS) rate was 87.8% (95% CI: 74.0–96.6%) (Fig. 4B). The intracranial response (ICR) rate reached 85.7% (95% CI: 51–99%), with three patients achieving a complete intracranial response (Fig. 4C, D).
CNS activity of the alectinib plus bevacizumab combination in ALK-rearranged NSCLC. A Cumulative incidence of brain metastasis in patients without brain lesions at diagnosis; B Intracranial progression-free survival in the intended-to-treat population. C Swimmer plot of the course of the patients with baseline BM (n = 7), showing duration of response (DOR), time on the experimental therapy, time without bevacizumab, CNS progression, deaths, adverse events, and ongoing treatment according EML4-ALK variant type. D Best percentage of tumor shrinkage in the CNS.
Safety
Adverse events of any grade were observed in 40 (97.5 %) patients. The most prevalent symptoms were diarrhea (75.6%), proteinuria (70.7%), anemia (58.5%), peripheral edema (41.5%), increased ALT (39.0%), increased AST (39.0%), and increased CPK (39.0%). Grade ≥3 adverse events affected 46.3% of patients, with the most frequent being proteinuria (22.0%), ALT increase (17.1%), and AST increase (9.8%) (Supplementary Table 3).
Dose reductions were observed in five patients (12.1%), all involving alectinib. Among them, three patients were reduced to 450 mg twice daily and two had a second reduction to the lowest permitted administration dose of 300 mg twice daily. Treatment interruptions were noted in 16 patients (39.0%), with 12 patients interrupting bevacizumab and four patients interrupting both medications. The primary adverse events associated with treatment interruption were proteinuria in all cases involving bevacizumab and increased AST or ALT levels in those interrupting alectinib.
Definitive discontinuation of bevacizumab was observed in 18 patients (43.9%), who continued with alectinib as monotherapy. The median duration of bevacizumab treatment was 22.7 months (95% CI: 21.1–26.7). Grade 3 proteinuria was the primary cause of discontinuation in 88% of cases. Among these patients, only one persisted with grade 2 proteinuria after 12 weeks from the definitive suspension, while the remaining cases were completely resolved. Treatment-related serious adverse events occurred in 7.3% of patients, including bowel perforation due to ulcerative colitis, nephrotic syndrome, and pulmonary thromboembolism. No fatal adverse events were observed during the clinical trial.
Patient-reported outcomes
All patients completed both questionnaires at baseline and at least once during the follow-up period, making them evaluable for PROs data. At the 12-month follow-up (54 weeks), all patients still on protocol treatment (n = 41) completed their questionnaires. By the 24-month follow-up (96 weeks), 30 of the 30 patients still on protocol treatment completed the questionnaire, representing 73.1% of the ITT cohort. At 36 months (144 weeks), 17 of the 17 patients still on protocol treatment completed the forms, representing 41.4% of the total cohort. Baseline and subsequent assessments are detailed in Supplementary Table 4.
The global Quality of Life (gQoL) improved clinically and statistically compared to baseline at month 12 (mean 65.2 vs. 77.4; p = 0.0116) and was maintained until week 144 (mean 65.2 vs. 75.98; p = 0.07) (Fig. 5A). All functioning scales, except the social scale, showed significant improvement compared to baseline. At the 24-month timepoint, physical and emotional functioning demonstrated a statistically significant increase compared to baseline (74.63 vs. 86.67, p = 0.004 and 72.97 vs. 85.28, p = 0.004, respectively). Furthermore, emotional functioning continued to show significant improvement at 36 months (72.97 vs. 88.73, p = 0.02). Clinical and statistical improvements were maintained throughout the three years analyzed (Supplementary Note 1: Fig. S1A–C).
Mean change from baseline (±Standard Error) in EORTC QLQ-C30 for A Global Quality of Life and in EORTC QLQ-LC13 for B cough, C chest pain, D dyspnea (multi-scale item), and E composite symptom endpoint. Baseline was defined as the last assessment performed prior to administration of the first cycle of the study combination. The composite score was calculated as the mean of the scores for cough, dyspnea, and chest pain. Score changes of ≥10 points were considered clinically meaningful.
Significant improvements from baseline in the symptom scores assessed using the EORTC QLQ-C30 were observed for fatigue, nausea and vomiting, pain, dyspnea, insomnia, appetite loss, and constipation at the 12-month timespan. However, diarrhea was the only symptom that worsened significantly at the 12-month milestone but declined in the last interval analyzed (Supplementary Note 1: Table S3 and Fig. S1D).
The EORTC QLQ-LC13 results showed significant amelioration in coughing and dyspnea symptoms at 12 and 24 months. (Figs. 5B and S2C). Regarding the composite symptom score, significant changes from baseline and overtime were observed at all analyzed timepoints (28.82 vs. 10.66, p < 0.0001 for 12 months; 28.82 vs. 11.60, p = 0.0013 for 24 months; and 28.82 vs. 12.20, p = 0.0091 for 36 months) (Fig. 5E). The median time-to-deterioration (TTD) in gQoL was not reached. At week 144, among 17 of the 17 patients that reached this timepoint, patients without clinically meaningful deterioration was 68.8% (95% CI: 56.1–85.2) (Supplementary Note 1; Fig. S1D).
Discussion
In the ALEK-B trial, the addition of bevacizumab to alectinib demonstrated a potent and effective combination for patients with metastatic ALK-positive NSCLC. This combination achieved meaningful PFS rates of 97% at 12 months and 64% at 36 months. Additionally, the 36-month overall survival (OS) rate was an impressive 88% with the alectinib plus bevacizumab regimen. This combination also showed significant efficacy in preventing CNS progression in patients with brain metastasis, with a 36-month icPFS of 80%. For patients without brain metastasis at baseline, the cumulative incidence (CI) of new brain lesions was 10.6%, highlighting the preventive benefit of the treatment. Furthermore, the study confirmed the feasibility and safety of the alectinib and bevacizumab combination in the study population, indicating its potential to be explored in further randomized trials for this patient group.
Despite the well-documented efficacy of alectinib and brigatinib as first-line treatments, a proportion of patients (around 35%) have been reported to experience progression within the first 12 months of therapy in prior studies4,16. Similarly, the use of the third-generation ALK-TKI lorlatinib in the CROWN trial showed that 22% of patients experienced progression during the first year17,18. In our phase 2 study evaluating the combination of alectinib and bevacizumab, only one patient experienced disease progression within 12 months. This observation stands out when considering historical data on alectinib monotherapy, such as the 12- and 36-month PFS rates of 76% and 46.4%, respectively, reported in the ALEX trial4. While acknowledging the inherent challenges in drawing conclusions across different studies, our findings suggest that the combination of alectinib and bevacizumab may have the potential to mitigate primary resistance or delay the emergence of early resistance mechanisms associated with second-generation ALK-TKIs.
These findings were further supported by a post hoc analysis with extended follow-up, which reported a 36-month PFS rate of 64.2% (95% CI 56.1–85.2) with the combination of alectinib and bevacizumab. The potential impact of the antiangiogenic agent continues to show a sustained benefit. In comparison, the 36-month PFS rates for alectinib and brigatinib in the ALEX and ALTA-1L trials were 46.4% and 43%, respectively4,16. Lorlatinib demonstrated a promising 36-month PFS rate of 63.5%, confirming its more potent inhibition compared to second-generation ALK-TKIs17. More recently, the updated data from the CROWN study confirmed a striking 60-month PFS rate of 60%19. While these improved progression-free intervals represent significant clinical benefits, they also come with increased costs in terms of toxicity which must be balanced against the enhanced efficacy observed in prolonging PFS.
In the present study, clinically meaningful systemic responses were observed in all patients, resulting in an ORR of 100%. The combination of alectinib and bevacizumab demonstrated robust, deeper, and durable responses, reaching a 36-month DOR rate of 62.6% (95% CI 56.1–85.2), indicating more prolong benefits than second generation ALK-TKIs as monotherapy16,17,20.
Although our cohort had a lower frequency of brain metastases at diagnosis (17%), this is lower than the 30–42% typically reported in most clinical trials and real-world cohorts21,22, including the largest LATAM cohort, where the reported rate was 31%22. This difference may be attributed to the sequential nature of our sampling process combined with our selection criteria, which excluded symptomatic brain metastases. The addition of bevacizumab to alectinib was highly efficacious in preventing CNS progression, likely contributing to the lower overall risk of progression observed in this study. Notably, the 36-month intracranial PFS was 87.8%, even though only one patient had received previous radiotherapy. ALK-positive NSCLC is characterized by a high prevalence of brain metastases, with approximately 60% of patients developing brain metastases within six years of diagnosis, representing a significant adverse prognostic factor in this population23. Historical data from the ALEX trial reported a higher risk of progression within the first 12 months, with a 16% cumulative incidence of brain metastases21. In contrast, with nearly 3 years of intracranial follow-up using the alectinib plus bevacizumab combination, the cumulative incidence was 8.8% which suggest an intriguing potential protective role of the antiangiogenic in this population.
These findings must be contextualized alongside the recent results from lorlatinib trials, which demonstrated the highest CNS efficacy reported in a randomized trial for patients with and without brain metastases, with 60-month PFS rates of 83% and 96%, respectively. This evidence underscores the potency of third-generation ALK inhibitors in preventing CNS progression24. Our phase 2 trial suggests that combining alectinib with bevacizumab could further delay resistance mechanisms and enhance CNS protection with second-generation ALK TKIs, as reflected in the impressive 36-month intracranial PFS and lower cumulative incidence of new brain metastases. However, whether the addition of an antiangiogenic agent can provide a similar benefit with third-generation TKIs like lorlatinib remains unknown. Future randomized trials are warranted to determine if this combination could further optimize CNS outcomes in ALK-positive NSCLC.
ALK-positive NSCLC is a heterogeneous population with varied prognoses influenced by EML4-ALK variants and the presence of concurrent genomic alterations, both of which have been associated with worse clinical outcomes and a higher risk of brain metastases. Identifying subgroups that may benefit from treatment escalation is becoming increasingly relevant in clinical practice. Although not a primary objective of this study, an exploratory analysis was conducted to assess the potential impact of EML4-ALK variants and concurrent co-alterations on treatment outcomes. No differences in efficacy were observed with the combination of alectinib plus bevacizumab, which contrasts with previous evidence from brigatinib and alectinib monotherapy. However, these findings are likely limited by the small sample size of our trial25. Interestingly, patients with poor-prognosis mutations, such as homozygous loss of CDKN2A/B and TP53 mutations, did not experience outcomes as unfavorable as previously reported in our LATAM cohort, where shorter PFS and OS were observed22,26. Further studies with larger cohorts are warranted to clarify the prognostic impact of these genetic features and identify subgroups that could benefit from treatment intensification.
The proportion of patients who developed any grade or grade 3–5 adverse events was slightly higher than those reported with alectinib monotherapy in the ALEX trial, particularly due to increased incidences of diarrhea, peripheral edema, and hepatotoxicity, which might have been potentiated by the addition of bevacizumab. Notably, all patients showed complete resolution of these adverse events with medical support or temporary treatment cessation. Of special interest was the rate of all grades and grade 3–4 proteinuria, reported in 70.7% and 22% of patients, respectively, leading to bevacizumab treatment discontinuation in 16 patients (39%). These discontinuation rates were considerably higher than those previously reported for combinations of alectinib with antiangiogenic agents or chemotherapy plus antiangiogenic treatments14,27. We hypothesize that this may be partially attributed to the prolonged bevacizumab exposure, nearly two years of continuous administration, exceeding the duration reported in other metastatic settings or larger trials such as the phase 4 SAiL study28,29. Furthermore, this study used the highest recommended dose of bevacizumab (15 mg/kg) without dose adjustments allowed. Despite the high discontinuation rate of bevacizumab, adherence to alectinib remained uncompromised, with no significant increase in treatment interruptions. Remarkably, only one non-fatal thrombosis-related event was observed, and no cardiac or hemorrhagic events were reported.
Unlike the pivotal ALEX and CROWN trials19,20, which required only a single positive test for ALK rearrangement, ALEK-B mandated NGS for all patients. This standardized approach ensured detailed prognostic information, such as variant type, co-mutations, and variant allele frequency, and may have reduced false-positive cases compared to the phase III trials, as recent studies suggest false-positive rates could lead to early progression30.
Quality of Life (QoL) deterioration is a common concern for almost all patients with metastatic NSCLC due to both disease burden and treatment-related side effects. In their respective trials, alectinib, brigatinib, and lorlatinib monotherapy have demonstrated numerical improvements in patient-reported outcomes (PROs) assessed using the EORTC QLQ-C30 and the lung cancer-specific module (EORTC QLQ-LC13) compared to crizotinib31. ALK-TKIs have been associated with sustained symptom relief, particularly for cough, gastrointestinal issues, and the composite symptom endpoint (cough, dyspnea, and chest pain).
In the present analysis, the combination of alectinib and bevacizumab significantly improved global QoL and functioning scales, with notable reductions in individual symptoms such as cough and the composite endpoint compared to baseline. These improvements were observed as early as the first two months of treatment and were sustained throughout the analysis period. Despite the increased frequency of clinic visits and the morbidity associated with intravenous infusions, these factors did not negatively impact PROs over time. However, a significant limitation of this study was the high proportion of patients (43.9%) who discontinued bevacizumab during the trial. While QoL analyses included all evaluable patients, the results did not differentiate between those receiving the combination therapy and those who continued on alectinib monotherapy after bevacizumab discontinuation. Despite this limitation and the lack of maturity of this analysis, the sustained trends in QoL improvements observed throughout the study suggest that the discontinuation of bevacizumab did not compromise the overall positive impact on QoL outcomes. Nonetheless, a more detailed future QoL analysis, distinguishing between treatment phases and patient subsets, could provide further insights into the contribution of each component to the observed outcomes.
This study had other limitations. As a single-center, open-label, investigator-assessed outcome trial, definitive conclusions regarding its effectiveness cannot be drawn, and there is a risk of overestimating the potential benefits. The single-arm design and the lack of a comparison with the standard treatment further limit the ability to draw robust conclusions. Although the overall toxicity profile was reassuring, specific symptoms, such as the increased risk of proteinuria and diarrhea, raise concerns about the chosen regimen in the ALEK-B trial. The optimal dose and duration of antiangiogenic therapy, particularly in ALK-positive NSCLC patients where the median treatment duration could exceed two years under active treatment, remain to be elucidated19,20,25, considering that more than one-third of the patients stopped bevacizumab. Additionally, it is necessary to question whether this regimen is suitable for upfront treatment, especially in light of recent positive results for lorlatinib.
Despite the promising results recently published for lorlatinib, specific populations may not be eligible due to comorbidities or may face access limitations to these medications. However, these limitations do not diminish the intriguing results of alectinib plus bevacizumab combination, which may potentiate an already effective treatment without compromising safety and adherence to the main therapy. A longer follow-up of the present study, analysis of mechanisms of resistance, and subsequent therapy analysis are needed to address these questions. Currently, other trials are exploring escalating strategies, such as adding platinum-based chemotherapy to anti-ALK TKI in the advanced setting as frontline therapy (NCT05200481)32.
In conclusion, the addition of bevacizumab to alectinib significantly prolonged PFS and effectively prevented early systemic and CNS progression events in patients with advanced ALK-positive NSCLC, regardless of the presence of brain metastases at baseline. This combination induced profound and durable responses, including within the CNS, without compromising QoL. While the toxicity profile was higher than expected, no permanent damage or treatment-related deaths were reported. Limiting the number of antiangiogenic cycles may mitigate these issues. These findings support the need for a phase III randomized controlled trial to definitively determine whether the addition of an antiangiogenic to a second or even a third-generation TKI provides significant benefits over a next generation ALK-TKI monotherapy, particularly in high-risk ALK-positive populations.
Methods
Study design, participants, and data collection
The ALEK-B trial was a single-arm, open-label, phase 2 study conducted at the Instituto Nacional de Cancerología in Mexico. Consecutive patients with metastatic non-squamous NSCLC, treatment-naïve, underwent molecular assessment using FDA-approved methods, including fluorescence in situ hybridization or immunohistochemistry (D5F3 assay). Adequate evaluable tissue was mandatory for next-generation sequencing (NGS) analysis at diagnosis and progression. Our trial was designed, conducted and reported in compliance with CONSORT and STARD guidelines.
Other inclusion criteria were the presence of measurable target lesions according to the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.133, and an Eastern Cooperative Oncology Group performance status (ECOG PS) score of 0–2. Patients with leptomeningeal carcinomatosis, active hepatitis infection, history of other malignant diseases, previous targeted therapy, or hypersensitivity to any of the drugs in the study were excluded from the trial.
Informed consent was obtained from all patients prior to enrollment. This study was approved by the Institutional Ethics Committee under the project ID: CI/2017/054 which was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines outlined by the International Conference on Harmonization and registered at ClinicalTrials.gov (NCT03779191). See trial protocol in Supplementary Note 2.
The ALEK-B trial has completed patient enrollment and is currently in the follow-up phase. As of the current data cut-off (December 2023), all patients have completed at least 12 months of follow-up, and the current analysis includes mature 36-month data. Follow-up will continue as per protocol until the final planned evaluation at 60 months (5 years) post-treatment initiation.
Pathology and molecular analysis
NGS employed the Foundation One CDX platform (Roche Pharma, Penzberg, Germany), utilizing targeted high-throughput hybridization-based capture technology to detect alterations and copy number alterations (CNAs) in 324 genes and select gene rearrangements. NGS analyses were mandatory in tissues or plasma at disease progression. Foundation Liquid was used in cases where tissue was not available, or the report was undetermined. Foundation One Liquid analyzed 311 genes for mutations, rearrangements, and CNAs changes using a highly sensitive and specific capture system.
Treatment
All patients received alectinib (600 mg twice daily) plus bevacizumab (15 mg/kg) every three weeks until disease progression or unacceptable adverse events. Dose reductions were allowed only for alectinib, based on international guidelines and the supplier´s fact sheet. Treatment interruptions were allowed for a maximum of 10 weeks and then resumed until grade 1 toxicity was reached or complete resolution of the adverse event was achieved. After progression, alectinib can be continued at the discretion of the treating physician in cases of oligoprogression, isolated CNS progression after local therapy, or clinical benefit.
Outcomes measures
The primary endpoint, 12-month PFS, was assessed in the intent-to-treat population, which included all patients who received at least one dose of the study treatment. Patients who were lost to follow-up, discontinued treatment for reasons unrelated to progression or death, or were alive without progression at the data cut-off date were censored at the time of their last adequate evaluation. A progression event was defined according to RECIST v1.1 criteria in the scheduled imaging follow-up studies. A contrast-enhanced computed tomography was conducted at baseline and then every six weeks until disease progression. Brain magnetic resonance imaging was performed at diagnosis and every 12 weeks in patients with and without BM until the occurrence of the first progressive CNS event. We employed the RECIST 1.1 criteria to evaluate intracranial response, utilizing MRI with contrast to measure target and non-target lesions.
The secondary endpoints were overall survival (OS), objective response rate (ORR), duration of response (DoR), best overall response (BoR), icPFS, intracranial response (ICR), duration of intracranial response (DIR), and PROs. OS was defined as the time from diagnosis to death or last follow-up. ORR was measured as the percentage of patients achieving a significant reduction in tumor size based on RECIST V1.1 criteria. The DoR represented the interval from the first documented response to the first occurrence of disease progression while BoR was the best response recorded from the start of treatment until disease progression. ICR was evaluated using modified RECIST criteria, and DICR was the duration from the onset of ICR to the progression of disease in the CNS.
PROs data were collected using the European Organization for Research and Treatment of Cancer Quality of Life of Cancer Patients Questionnaire (EORTC QLQ-C30) and the questionnaire for Lung Cancer symptoms (EORTC QLQ-LC13), as in previous studies of ALK-positive NSCLC patients34. PROs were assessed at baseline and every 21 days thereafter, corresponding to a new cycle until the end of treatment. Previously validated Mexican Spanish versions of these questionnaires were used to fulfill the translation and cultural adaptation requirements34. Higher scores on these scales indicate greater impact of symptoms. Raw scores were standardized from 0 to 100 points, defined as clinically meaningful changes in the mean score above ten-point score from baseline. TTD was defined as the time from allocation until confirmed clinically meaningful ≥10-point variation from baseline sustained for at least two consecutive evaluations or an initial ≥10-point change from baseline followed by death within the following five weeks.
Statistical analysis
The sample size was determined using a two-stage Simon design35, assuming a true 12-month PFS rate of 68% based on outcomes from the ALEX trial. The alternative hypothesis proposed a 12-month-PFS rate of at least 85% with a one-sided type I error level of 5% and a power of 80%. In this design, if nine or more of the initially intended 12 patients remained free of disease progression during stage 1, the treatment would warrant further investigation. Upon completion of stage two, if 33 or more patients remained without progression within the total cohort of 41 patients, the null hypothesis would be rejected.
Following the accrual of the first 12 patients, any experienced disease progression, prompting continuation to the second stage. Upon completion of recruitment with a 12-month follow-up, only one progression event was observed, crossing the efficacy boundary specified by the design and justifying further exploration of this combined therapy. For the current publication, we extend our analysis to include outcomes at 36 months, providing a comprehensive assessment of long-term PFS. This extended follow-up period allows us to evaluate the durability of the treatment response beyond the initial 12-month endpoint, offering insights into the sustained efficacy of the combined therapy.
Continuous variables were presented as means and standard deviations or medians and 25th and 75th percentiles (p25–p75), depending on the data distribution assessed by the Shapiro-Wilk test. To estimate PFS rates at 12 and 36 months, we utilized the Kaplan-Meier method, which accommodates censored data and provides robust survival probability estimates over time. The median follow-up duration for both PFS and overall survival (OS) was estimated using the reverse Kaplan-Meier method. To estimate hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs), we employed the Cox proportional hazards model. The CIs were computed using the Wald method. The length of follow-up precluded the determination of median times for certain event-free survival endpoints. Instead, survival rates at 12, 24, and 36 months with their respective 95% confidence intervals (CIs) were reported. For participants lost to follow-up, their last contact date was recorded along with documented reasons for loss. Differences between exploratory subgroups were analyzed using the log-rank test, with statistical significance set at p < 0.05.
PROs DCO and analysis were performed three months after the efficacy and safety DCO, for all treated patients who completed the baseline assessment and at least one PRO questionnaire post-baseline. These DCO discrepancies make the efficacy and QoL datasets differ in analysis date and thus evaluable population. PROs were assessed at baseline and subsequently on day 1 of each 3-week treatment cycle. For the statistical analysis, a mixed-effects model was used to assess questionnaire score changes from baseline to 12, 24, and 36 months. Longitudinal mean scores change from baseline of 10 points or higher were considered clinically meaningful34. Patients without clinically meaningful deterioration were censored at the time of their last PRO assessment.
Analyses and plots were performed using IBM SPSS Statistics for Windows version 26 (Chicago IL. USA), RStudio 2023.03.0 + 386 “Cherry Blossom” for Windows, and GraphPad Prism for Windows version 8.0.2 (263).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The trial protocol and statistical analysis plan can be found in the Supplementary Information File. Source data are provided as a Source Data file. Detailed individual de-identified patient data will be shared for only for research purposes and clinical study analyses, up to request to the corresponding author (O.A.; oscararrietaincan@gmail.com). Patient-level data are summarized in Table 1 and Fig. 2. Source data are provided with this paper.
Change history
12 December 2025
A Correction to this paper has been published: https://doi.org/10.1038/s41467-025-67648-x
References
Arrieta, O. et al. Molecular epidemiology of ALK rearrangements in advanced lung adenocarcinoma in Latin America. Oncology 96, 207–216 (2019).
Schneider, J. L., Lin, J. J. & Shaw, A. T. ALK-positive lung cancer: a moving target. Nat. Cancer 4, 330–343 (2023).
Hallberg, B. & Palmer, R. H. The role of the ALK receptor in cancer biology. Ann. Oncol. 27, iii4–iii15 (2016).
Peters, S. et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N. Engl. J. Med. 377, 829–838 (2017).
Gainor, J. F. et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 6, 1118–1133 (2016).
Jackson, A. L., Zhou, B. & Kim, W. Y. HIF, hypoxia and the role of angiogenesis in non-small cell lung cancer. Expert Opin. Ther. Targets 14, 1047–1057 (2010).
Zinner, R. G. et al. PRONOUNCE: randomized, open-label, phase III study of first-line pemetrexed + carboplatin followed by maintenance pemetrexed versus paclitaxel + carboplatin + bevacizumab followed by maintenance bevacizumab in patients ith advanced nonsquamous non-small-cell lung cancer. J. Thorac. Oncol. 10, 134–142 (2015).
Nakagawa, K. et al. Ramucirumab plus erlotinib in patients with untreated, EGFR-mutated, advanced non-small-cell lung cancer (RELAY): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 20, 1655–1669 (2019).
Passaro, A., Janne, P. A., Mok, T. & Peters, S. Overcoming therapy resistance in EGFR-mutant lung cancer. Nat. Cancer 2, 377–391 (2021).
Piccirillo, M. C. et al. Addition of bevacizumab to erlotinib as first-line treatment of patients With EGFR-mutated advanced nonsquamous NSCLC: the BEVERLY multicenter randomized phase 3 trial. J. Thorac. Oncol. 17, 1086–1097 (2022).
Nishio, M. et al. RELAY, Ramucirumab Plus Erlotinib (RAM+ERL) in untreated metastatic EGFR-mutant NSCLC (EGFR+ NSCLC): association between TP53 status and clinical outcome. Clin. Lung Cancer 24, 415–428 (2023).
Hrustanovic, G. et al. RAS-MAPK dependence underlies a rational polytherapy strategy in EML4-ALK-positive lung cancer. Nat. Med. 21, 1038–1047 (2015).
Martinengo, C. et al. ALK-dependent control of hypoxia-inducible factors mediates tumor growth and metastasis. Cancer Res. 74, 6094–6106 (2014).
Lin, J. J. et al. Safety and activity of alectinib plus bevacizumab in patients with advanced ALK-rearranged non-small-cell lung cancer: a phase I/II study. ESMO Open 7, 100342 (2022).
Arrieta, O. et al. A phase II study of alectinib in combination with bevacizumab as first-line treatment in advanced NSCLC with confirmed ALK fusion: ALEK-B trial. J. Clin. Oncol. 40, 9074–9074 (2022).
Camidge, D. R. et al. Brigatinib versus crizotinib in advanced ALK inhibitor-naive ALK-positive non-small cell lung cancer: second interim analysis of the phase III ALTA-1L trial. J. Clin. Oncol. 38, 3592–3603 (2020).
Solomon, B. J. et al. Efficacy and safety of first-line lorlatinib versus crizotinib in patients with advanced, ALK-positive non-small-cell lung cancer: updated analysis of data from the phase 3, randomised, open-label CROWN study. Lancet Respir. Med. 11, 354–366 (2023).
Shaw, A. T. et al. First-line lorlatinib or crizotinib in advanced ALK-positive lung cancer. N. Engl. J. Med 383, 2018–2029 (2020).
Solomon B. J., et al. Lorlatinib versus crizotinib in patients with advanced ALK-positive non-small cell lung cancer: 5-year outcomes from the phase III CROWN study. J. Clin. Oncol. 42, 3400–3409 (2024).
Mok, T. et al. Updated overall survival and final progression-free survival data for patients with treatment-naive advanced ALK-positive non-small-cell lung cancer in the ALEX study. Ann. Oncol. 31, 1056–1064 (2020).
Gadgeel, S. et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann. Oncol. 29, 2214–2222 (2018).
Lara-Mejia, L. et al. Impact of concurrent genomic alterations on clinical outcomes in patients with ALK-rearranged NSCLC. J. Thorac. Oncol. 19, 119–129 (2023).
Johung, K. L. et al. Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J. Clin. Oncol. 34, 123–129 (2016).
Solomon, B. J. et al. Post hoc analysis of lorlatinib intracranial efficacy and safety in patients with ALK-positive advanced non-small-cell lung cancer from the phase III CROWN study. J. Clin. Oncol. 40, 3593–3602 (2022).
Camidge, D. R. et al. Brigatinib versus crizotinib in ALK inhibitor-naive advanced ALK-positive NSCLC: final results of phase 3 ALTA-1L trial. J. Thorac. Oncol. 16, 2091–2108 (2021).
Parikh, K. et al. Impact of EML4-ALK variants and co-occurring TP53 mutations on duration of first-line ALK tyrosine kinase inhibitor treatment and overall survival in ALK fusion-positive NSCLC: real-world outcomes from the GuardantINFORM database. J. Thorac. Oncol. 19, 1539–1549 (2024).
Watanabe, S. et al. Phase II trial of the combination of alectinib with bevacizumab in alectinib refractory ALK-positive nonsquamous non-small-cell lung cancer (NLCTG1501). Cancers 15, 204 (2022).
Zhu, X., Wu, S., Dahut, W. L. & Parikh, C. R. Risks of proteinuria and hypertension with bevacizumab, an antibody against vascular endothelial growth factor: systematic review and meta-analysis. Am. J. Kidney Dis. 49, 186–193 (2007).
Crino, L. et al. Safety and efficacy of first-line bevacizumab-based therapy in advanced non-squamous non-small-cell lung cancer (SAiL, MO19390): a phase 4 study. Lancet Oncol. 11, 733–740 (2010).
Frankel, D. et al. Comparison between immunocytochemistry, FISH and NGS for ALK and ROS1 rearrangement detection in cytological samples. Int. J. Mol. Sci. 23, 10556 (2022).
Mazieres, J. et al. Patient-reported outcomes from the randomized phase 3 CROWN study of first-line lorlatinib versus crizotinib in advanced ALK-positive non-small cell lung cancer. Lung Cancer 174, 146–156 (2022).
Duruisseaux, M. et al. A phase II randomized, open-labelled, multicenter study of safety and efficacy of combination brigatinib and carboplatin-pemetrexed therapy or brigatinib monotherapy as first-line treatment in patients with advanced ALK-positive non–small cell lung cancer (IFCT-2101 MASTERPROTOCOL ALK). J. Clin. Oncol. 40, TPS9144–TPS9144 (2022).
Eisenhauer, E. A. et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer 45, 228–247 (2009).
Perol, M. et al. Patient-reported outcomes from the randomized phase III ALEX study of alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer. Lung Cancer 138, 79–87 (2019).
Simon, R. Optimal two-stage designs for phase II clinical trials. Control Clin. Trials 10, 1–10 (1989).
Acknowledgements
We express our gratitude to the patients, their families, site investigators, and the personnel who participated in this study. Roche provided funding and access to bevacizumab. The funder had no role in the study design, data collection, analysis, interpretation or writing of this report. The corresponding author had full access to all the data and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
O.A.: Conceptualization, Writing - Review & Editing, Formal Analysis, Supervision, Resources. L.L.-M.: Conceptualization, Writing - Original Draft, Analysis, Investigation, Data curation. E.R.-G.: Formal analysis, Data Curation, Visualization, Investigation, Writing – Review & Editing. E.C.-P. Formal Analysis, Investigation, Data curation, Writing - Original Draft. L.C.-M.: Investigation, Data curation. M.R.-R.: Investigation, Data curation. D.D.D.: Investigation, Data curation. A.F.C.: Data curation, Formal analysis Writing - Review & Editing, G.C.-R.: Data curation, Formal analysis. J.R.: Formal analysis. A.G.-R.: Investigation, Data curation. R.R.: Writing - Review & Editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
O.A. reports personal fees from Pfizer, Lilly, Merck, and Bristol Myers Squibb, and grants and personal fees from Astra Zeneca, Boehringer Ingelheim, and Roche. L.L.-M. has participated as a speaker for Astra Zeneca, Roche, Pfizer, Takeda, Janssen Cilag and Boehringer Ingelheim and personal fees from Janssen Cilag, Pfizer, Takeda, and Roche. A.F.C.: reports grants from Merck Sharp & Dohme, Boehringer Ingelheim, Roche, Bristol-Myers Squibb and The Foundation for Clinical and Applied Cancer Research—FICMAC., other from Pfizer, Boehringer Ingelheim, Astra Zeneca, MSD, BMS, Celldex, Roche, personal fees from Merck Sharp & Dohme, Boehringer Ingelheim, Roche, Bristol-Myers Squibb, Pfizer, Novartis, Celldex Therapeutics, Foundation Medicine, Eli Lilly and Foundation for Clinical and Applied Cancer Research—FICMAC, outside the submitted work. The remaining authors declare no conflicts of interest.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Arrieta, O., Lara-Mejía, L., Rios-Garcia, E. et al. Alectinib in combination with bevacizumab as first-line treatment in ALK-rearranged non-small cell lung cancer (ALEK-B): a single-arm, phase 2 trial. Nat Commun 16, 4553 (2025). https://doi.org/10.1038/s41467-025-59744-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-59744-9