Abstract
End stage kidney disease and dialysis are lifetime limiting and lifestyle-defining conditions with enormous costs to the health care system. Despite a severe organ shortage, thousands of organs that are retrieved for transplantation go to waste every year because of the presumed inadequacy of organ quality and/or the limited organ preservation time. Normothermic kidney machine perfusion (NMP) holds the potential to resolve this through improved preservation, prolonged preservation time, kidney quality assessment, reconditioning and treatment. We herein develop a perspective on the potential, but also the hurdles towards the breakthrough of this technology.
Similar content being viewed by others
Introduction
According to a recent assessment by the International Society of Nephrology (ISN), the global prevalence for chronic kidney disease (CKD) is 9.5%1. Chronic kidney disease affects 1 out of 7 people in the US. Hence, approximately 35.5 million people are affected by CKD2 and nearly 808,000 people are living with end stage kidney disease (CKD stage 4-5) in the US alone. It is estimated that about 15−20% of patients with chronic kidney disease CKD (especially those in stages 3–5) will progress to CKD stage 5 over a span of 10−20 years. Only 30% of patients suffering from CKD stage 5 are placed on a waiting list and the average waiting time is 3−5 years1,2,3,4.
With an overall 50% 5 year patient survival, ESRD ranks in the range of many types of cancer. The prevalence continues to rise, and CKD is expected to further accelerate as a leading cause of death and a driving force of health care costs3,4. While kidney transplantation is available in 70% of the countries, the service is often underdeveloped, and the number of available kidneys is insufficient to serve the growing need for renal replacement therapy. In the US, 69% of patients with kidney failure are on dialysis and 31% are living with transplants2. In Europe, kidney transplantation constitutes between 2- and 40% of the renal replacement therapy5. The proportional distribution between patients on dialysis versus patients with transplants remains a concern. Compared to transplantation, dialysis is associated with reduced survival, impaired quality of life and high incurring costs to the health care system1,2,6,7.
The Healthy People 2020 initiative is a 10 year national objective for improving the health in the US. The initiative pursues to “Increase the proportion of patients receiving a kidney transplant within 3 years of kidney failure (CKD stage 4-5)”8. Furthermore, the Advancing American Kidney Health Initiative aims at doubling the number of available organs by 20308. One key objective to comply with this ambition is to increase the number of organs that are transplanted after procurement of deceased donor organs. To increase the number of transplantations, but also guarantee good outcomes, this requires an ability to limit organ injury caused by cold organ storage and to properly assess the donor organ quality and function prior to transplantation.
The outcomes after deceased donor kidney transplantation are generally good and there is a relatively high threshold to accept a marginal deceased donor kidney for transplantation. Nonetheless, in countries where the system penalizes below average transplant outcomes, a reluctance to transplant marginal or suboptimal kidneys is common
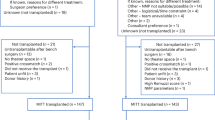
The fear of transplanting an imperfect organ outweighs the potential benefits. Hence, while the outcome of kidney transplant is generally very good, many patients remain on dialysis. This behavior inflates the number of patients remaining on dialysis for many years and with a poor prognosis9,10,11,12,13,14,15. The organ transplant rate in the US has steadily increased over the past 10 years and reached a record high in 2023, but the proportion of transplanted organs out of the pool of authorized organs has steadily declined (Fig. 1; srtr annual report, https://srtr.transplant.hrsa.gov/adr/adr2023)16. According to the SRTR database, 18,527 organs were recovered but not transplanted in 2023. The proportion of discarded organs has grown from 13,8% in 2012 to 19,4% in 2023. Reasons for kidney discard including age, histology, presumed inferior quality and long ischemia times15,16. Over the past decade, 112,622 organs have been discarded in the US. At the same time, many kidneys were transplanted with sub-optimal outcomes16,17,18. A key determining reason for both these problems is the inability to accurately define kidney quality and kidney damage resulting from donor kidney history, the process of brain death, kidney retrieval, cold storage and transplantation. The decision to transplant a kidney is made by assessment of donor factors, in some cases histological evaluation and measurement of perfusion parameters collected during hypothermic machine perfusion (HMP). HMP allows an assessment of flow and resistance indices to determine quality. However, the predictive value of these parameters to predict outcome has shown poor accuracy19.
(https://srtr.transplant.hrsa.gov/adr/adr2023), Fig. 1 describes the annual numbers of organs transplanted between 2012 – 2023. To put this into perspective of the number of organs authorized for use in transplantation, the figure and the corresponding table display the annual number of the organs authorized for transplantation and the number of organs retrieved but not transplanted (discarded after retrieval). Conceptually, all organs authorized for use in transplantation represent the donor organ pool. However, not all reasons for non-retrieval and for post-retrieval discard are immediately modifiable (see also Fig. 3).
In contrast to the kidney, discard rates in liver transplantation are declining with adoption of normothermic machine perfusion (NMP)20. NMP involves attaching an organ to a device to reestablish circulation and cellular metabolism. This enables the organ to be reconditioned, allows an assessment of function, and provides the opportunity to treat the organ prior to transplantation. In liver transplantation, NMP is increasingly well established throughout Europe and the US. Portable devices such as the OrganOx Metra and Transmedics Organ Care System facilitate transport to allow for NMP during the entire ex-situ time. In contrast to the evidence in randomized controlled trials (RCTs), the real-world use of the OrganOx Metra device mostly follows a ‘back to base’ concept, meaning the perfusion set-up is not used for transportation but that the organ is shipped on static cold storage (SCS) and NMP is only initiated when the organ arrives at the transplant center. Its application is associated with reductions in early graft dysfunction (EAD)21,22,23 and post-reperfusion syndrome24. Viability assessment based on functional parameters, bile production and bile content during NMP has enabled an increase in utilization24,25,26,27. It has also enabled livers to be preserved for extended periods of time allowing transplantation during daytime hours27,28. In heart transplantation, clinical trials have established the safety and feasibility of NMP and have enabled the safe extension of preservation to 8 h, but as yet have failed to show improvements in graft survival29. The use of NMP has increased organ utilization and facilitates donation after cardiocirculatory death (DCD) and extended criteria donor (ECD) heart transplantation30,31. While a consensus over the viability assessment remains to be established, biochemical parameters and contractile function are currently considered. Ex vivo lung perfusion (EVLP) has been shown to reduce the rate of primary graft dysfunction32. It is also used to assess viability and has played an instrumental role in the utilization of lungs from marginal donors33. This is particularly important with current utilization rates of around 20%34.
Development of NMP technology for kidney transplantation has lagged the development of other organs. HMP is well established as a superior method of preservation with better early and long-term graft function compared to static cold storage19,35,36,37 HMP, however, leaves the kidney in a metabolically inactive state and perfusion times remain limited. Therefore, HMP has limited value as a tool to assess kidney function. Oxygenated HMP supports a low level of metabolism that occurs at 4–8 °C with some indication of improved graft function compared to standard HMP19,37. Seminal work by Brasile et al has explored the importance of metabolic resuscitation for graft function upon transplantation and has laid the foundation for development of perfusion systems at warmer temperatures, such as subnormthermic perfusion (SMP) or normothermic perfusion (NMP)38. NMP offers many advantages over HMP and oxygenated HMP. The restoration of oxidative metabolism enables kidney function and assessment of kidney viability. However, the complex interactions between the anatomy of the countercurrent system needed for urine concentration, alternations in oxygen gradients in the medulla and mass solute reabsorption by the tubules under normothermic conditions indicate the complexity of kidney NMP and suggest that this is more complicated than NMP in other organs. A high energy and oxygen environment is required. Maintaining metabolic function ex-situ is demanding, particularly in ischemically injured kidneys. This metabolic paradox explains why progress has been faster in heart, liver and lung machine preservation compared to the kidney (see Table 1). For kidney NMP to advance, two aspects need to be addressed: (1) a specifically designed, automated, user friendly NMP device in combination with detailed perfusion protocols and perfusate recipes that allow the maintenance of the metabolic viability and functionality of the kidney, (2) a clear determination of ‘perfusion’ parameters that can be incorporated in the design of pivotal transplant outcome trials.
Kidney normothermic machine perfusion holds the promise to replace or shorten cold storage while enabling a thorough assessment of function and viability of kidney grafts. We expect this to facilitate a significantly higher utilization rate of procured kidneys. Further to the immediate impact on the number of organs available for transplantation, this technology may also serve as a future platform for transplant organ reconditioning, treatment and modification. While the demand is immense and the promise is apparent, the development of kidney NMP instruments and protocols is still evolving. In this perspective, we aim to describe the unmet needs in kidney transplantation and take a deep dive on the opportunities, but also the hurdles towards the clinical realization of kidney NMP in transplantation and beyond. While the opportunity is evident, the complexity of the task at hand still poses a big challenge.
Mechanisms of kidney injury during procurement and transplantation
The kidney is considered more tolerant of cold ischemic injury compared to other solid organs. Preservation times can reach over 24 h, but long cold ischemic times result in significant graft impairment after transplantation. The vulnerability of the kidney towards ischemia is determined by several mechanisms and eventually results in apoptosis, necrosis and necroptosis of various components of the nephron. The absence of oxygenation in the donor kidney affects all cell types reliant on oxidative phosphorylation for energy such as the proximal tubules. In fact, acute ischemic or inflammatory insults result in tubular epithelial necrosis, in the S3 segment which operates at near hypoxia. Podocytes and endothelial cells mainly rely on glycolysis for their function and tolerate a certain degree of ischemia39. However, the tubular epithelial cells that perform mass solute reabsorption through a very specialized energy demanding set of transporters, critically depend on intact mitochondrial TCA for function and survival40. At the mitochondrial level, ischemia results in glycolytic overload of TCA cycle intermediates and elevated intracellular Ca²⁺ concentrations, which set the stage for reperfusion injury41. In particular, accumulation of succinate at complex I of the electron transport chain in the mitochondrial membrane during ischemia was shown to be deleterious42. It is believed that succinate may be oxidized upon reperfusion by reverse electron flow through complex I leading to a burst of reactive oxygen species43 (Fig. 2). These mitochondrial metabolic alterations increase the propensity of mitochondria upon re-energizing to form mitochondrial permeability transition pores (mPTPs)44, that subsequently can set in motion a cascade of events that lead to extensive innate immune activation. The leakage of mitochondrial DNA (mtDNA) into the cytosol activates the cGAS-STING pathway45 and leads to NFkB activation and inflammation. In renal epithelial cells, such cellular activation has been directly linked to the development of future kidney fibrosis46. Moreover, mPTP opening, in conjunction with death signals from neighboring cells—such as TNF and damage-associated molecular patterns (DAMPs)—is associated with necroptosis. This is a process where necrotic cell death is induced through activation of receptor-interacting protein kinases (RIPKs) that lead to further permeabilization of mitochondrial membranes through association with mitochondrial cardiolipin47. Depending on the extent of the injury, the regenerating tubular epithelium may adopt an inflammatory and senescent-associated secretory pathway (SAS) phenotype. In response to an overwhelming injury, the so-called failed repair cells prime the kidney towards progressive fibrosis47. Hence, damage and loss of donor kidney function can occur early and be sustained after transplantation.
Accumulated succinate at complex I of the electron transport chain can be oxided by reverse electron transport upon reperfusion and replenishment of anaplerotic substrates which leads to redox stress. This then will induce the formation of mitochondrial transition pores (mPTP), leakage of mDNA to the cytosol and induction of cGAS-STING inflammatory (NfkB) and necroptotic (RIPK1) signaling setting the stage for tissue injury and future development of fibrosis.
Post-transplantation, the consequence of cold ischemic injury manifests as acute tubular injury and delayed graft function (DGF). DGF is defined as the requirement for dialysis in the first week post-transplant. DGF does not have immediate life-threatening consequences and is usually reversible with recovery of the tubule cells. However, DGF is associated with an increased risk of early graft loss and incidences of acute rejection48,49.
Further to this impact on outcome, the short- and long-term economic impact and resource implications of DGF in kidney transplantation are substantial. Extended hospitalization, dialysis, immunosuppressive drug costs and greater overall healthcare resource demand contribute to higher costs50. Both warm and cold ischemia contribute to DGF, but the duration and severity of each play an important role in the ultimate outcome of the transplant. Warm ischemia and hence hypoxia- dysregulated cell metabolism primarily leads to redox stress and lipid peroxidation51. Cold ischemia further sets the stage for reperfusion injury by inducing sustained epithelial metabolic failure and release of specific DAMPs m such as cold-inducible RNA binding protein (CRIB)52,53,54. Together, these cellular injury mechanisms translate into endothelial cell activation and inflammation and secondary profibrotic responses in the later phase upon transplantation. Managing ischemic times (both warm and cold) is thus critical in reducing the incidence of DGF.
Potential and challenges of kidney NMP
NMP provides metabolic resuscitation and may mitigate mitochondrial permeability changes by flushing out pro-inflammatory factors from the extracellular space and by providing metabolic substrates and oxygen. This may reduce the susceptibility of epithelial cells to generate mitochondrial damage. In support, recent findings have demonstrated that, compared to static cold storage, normothermic storage and perfusion can indeed better preserve mitochondrial function, reduces inflammation and improve transplant outcomes in an auto-transplantation model in pigs55. These protective effects could be further enhanced by introducing a compound that targets mitochondria and supports the electron transport chain through local release of H2S55. Subnormothermic porcine kidney perfusion with an H2S supplemented blood in a DCD model resulted in lower apoptotic injury and a pro-survival gene expression pattern56. Metabolic isotope tracing studies demonstrated that warming of discarded human donor kidneys to subnormothermic temperature enabled re-establishment of cell metabolism, particularly in the vulnerable tubular epithelial compartment57. This was achieved in the absence of red blood cells as an oxygen carrier. Metabolic viability was extended without the development of oxidative injury over a period of 4 days. Despite the great potential and the interesting outlook for kidney NMP, several limitations complicate an immediate and global clinical implementation: Given the variety of different temperatures, perfusion strategies and solutions, there is currently no standardized perfusion protocol. In particular, the need for red blood cells as oxygen carrier needs further attention. The use of RBC is not only challenging from a logistics perspective but may also be associated with hemolysis and heme-mediated tissue injury that could off-set the tissue protective effects of blood-based perfusion on mitochondria and bioenergetic performance58. As an alternative to blood-based perfusion, the use of Hemopure and Sodium Thiosulfate with and without AP39 as H2S donor was assessed in a rate kidney transplant model and pig kidney perfusion model. Studies demonstrated higher urine output, lower urine protein levels and a better proximal tubular cell viability59,60. The use of RBCs and the associated hemolysis during machine perfusion of diseased donor kidneys drives progressive iron accumulation and phospholipid peroxidation. The observed accumulation of freeHb, iron, oxidized phospholipids, and their byproducts highlights how hemolysis within kidney preservation platforms can lead to ferroptosis58. This may also be specific to kidney NMP as e.g. livers have resident macrophages that can process tissue iron deposition61. Dialysis based free Hb removal reduces, and cell-free perfusion circumvents hemolysis-driven iron accumulation, phospholipid peroxidation, and acute kidney injury58. A novel perfusion technology currently in development may help to avoid hemolysis during kidney NMP and hence serve as a breakthrough instrument in the field62. Further to this, mechanisms to enhance mitochondrial stability and to prevent cellular damage should be addressed. This could improve metabolic function, but also prevent the release of DAMPS, complement activation and cytokine release63. A deepened understanding of kidney metabolism during NMP is needed to adequately determine perfusion conditions and recipe composition. This is especially true since renal perfusion distribution patterns are unique and show a particular dynamic during NMP64.
Some aspects of kidney NMP represent specific challenges and make it different from e.g. liver perfusion. These include the functional assessment of the kidney in the context of NMP. It remains unclear for example, if a kidney needs to produce urine and if creatinine clearance in the NMP environment is indicative of the functional capacity of a kidney. Further to this, the criteria for assessment of kidney viability are not well defined. Since kidney function and kidney viability are the key quality assessment criteria, a consensus on the definitions and the benchmarking is warranted. Further differences to other organs are the allocation system of kidneys resulting in longer travel distances and longer cold ischemia times. This is the result of a matching system, which aims for an immunological compatibility and the believe, that kidneys tolerate a longer cold storage time. While heart, liver and lung are mostly accompanied by groups of surgeons and perfusionists, the kidney mostly travels without medical professional oversight. The NMP technology has a higher complexity and exposes the kidney to a higher risk of failure. Establishing a transportation service for kidney similar to the heart and liver would come at high costs. Shipping kidneys on an NMP device would create the challenge of instrument back travel or a shared NMP device pool. The lack of commercially available portable NMP perfusion devices, that would allow for normothermic perfusion during transportation has limited the clinical practice to a short-term procedure after conventional storage and transport to the transplant center just prior to transplantation. Within the last 5 years, however, three commercial devices have been approved for clinical use for normothermic kidney perfusion in Europe: The Kidney Assist (XVIVO)65, ARK Kidney® (Ebers medical technology)66 and Perlife® system (Aferetica)67. The ARK kidney is the only portable device available. While this is meaningful for advancing kidney NMP, these technologies are yet to be tested in randomized controlled trials to establish an indication for use (Table 2).
Clinical Experience with Kidney NMP
To date, NMP has only been applied following hypothermic preservation as a back-at-base approach. The safety and feasibility of the technique has been tested, but efficacy remains to be established. The first report of NMP in kidney transplantation was published in 2011 using an adapted cardiopulmonary bypass system to perform a short period of NMP with a red cell-based solution at 36 °C on a DCD kidney68. This was followed by a clinical series demonstrating a low rate of DGF in 18 ECD kidneys using the same system and 1 h period of NMP with the same red cell-based solution69. Minor et al published a single case study followed by a case series of controlled oxygenated rewarming (COR) with a cell-free solution70,71. Kidneys were gradually rewarmed from 8 °C to 35 °C over a period of 90 min followed by 30 min of NMP at 35 °C before transplantation. The case series of 6 kidneys showed an improvement in creatinine clearance on day 7 and at 3 months post-transplant compared to matched SCS kidneys. Other case series have provided evidence on the safety and feasibility of NMP but found no improvement in graft function72,73. Only one randomized controlled trial (RCT) has been carried out comparing 1 h NMP with SCS in DCD kidneys74. The analysis included 135 DCD kidneys in the NMP group and 142 in the SCS group. There was no significant difference in the rate of DGF, 60.7% in the NMP kidneys and 58.5% in SCS kidneys. There was also no significant difference in graft function or graft survival at 12 months. Importantly, there were no complications or adverse events associated with NMP, demonstrating the safety and feasibility of the technique for a short period of NMP. A single case report demonstrated how NMP could be used to perform an intermediate period of NMP. NMP was carried out for 1 h on an ECD kidney after 10.5 h of static cold storage75. After NMP the kidney was flushed with cold preservation solution and placed back in ice for a further 5.5 h before transplantation. The kidney had immediate graft function. A more recent study investigated safety and feasibility of a 1−3 h NMP period on DCD kidney transplantation. The intervention resulted in a lower DGF rate, a lower serum creatinine and a higher eGFR at 1 month76. While this concept is feasible, it may be more beneficial to maintain NMP for longer periods to add time for assessment and limit the second SCS period. The OrganOx Metra K system is a portable device in development, designed to maintain kidneys under NMP conditions for prolonged periods77. Using a prototype system in the experimental setting, the capacity to preserve human kidneys for up to 24 h was demonstrated78. A unique feature of the system to maintain a near-physiological environment was the recirculation of urine into the perfusate during NMP. Replacing high volumes of urine with a crystalloid solution can result in high levels of sodium and abnormal acid–base balance. This system was recently used in a clinical study demonstrating the safety and feasibility of NMP for up to 23 h. In a preclinical study, the feasibility of kidney preservation for 48 h was suggested79,80. Prolonged NMP would be meaningful to assess and recondition the donor organ and improve the transplantation logistics. NMP has also been used to evaluate the suitability of ‘marginal’ kidneys for transplantation using a scoring system based on the macroscopic appearance and functional parameters81,82. Other studies include the use of NMP to appraise the blood supply to the ureter83, after surgical reconstruction to ensure vascular integrity84, to determine the patency of the microcirculation of poorly flushed kidneys85 and determine the suitability of a kidney from a donor with rhabdomyolysis for transplantation86. A currently ongoing clinical trial conducted by 34 lives, assesses if allocation success can be improved by preserving and assessing hard-to-place (HTP) donor kidneys87. (see also Table 3).
The importance of developing endpoints for the further development of NMP
NMP of kidney grafts can target several unmet needs. As with all innovations in health care, the path from an invention to clinical routine application is long and complex. The definition of a clinical trial path, of endpoints that are both acceptable to the regulating bodies, but also providing a robust indication, the size that makes it reasonable and economically sustainable to perform such a trial, the cost/benefit ratio on the market and many more aspects need to be met for the technology to be successful.
Learning from the evolution of NMP in other organs such as the liver, the pathway towards approval of preservation devices is depending on the temperature at which organs are preserved. While hypothermic preservation devices are class II medical devices (considered moderate risk classification for regulatory approval), normothermic preservation devices, typically used with blood-based preservation solutions, are mostly qualified as class IIb (higher risk within class II, often requiring more detailed evaluations) or III (high risk devices, requires Premarket Approval (PMA), with extensive safety and efficacy testing prior to clinical use)88,89. This categorization largely determines the path towards clinical development. The second key determination is the establishment of an indication for use. For currently existing NMP devices, the safety as displayed by a CE mark have been established, but no pivotal trials and hence no indications for its use have been developed. A careful determination of the indication for use, the development of a safe and effective preservation device and perfusion recipe and clarification of logistics together with a robust cost/benefit ratio are the critical factors for success of kidney NMP. Minimizing the cold ischemic injury preservation time is an important objective for the development of NMP. A porcine model showed that protective effects of NMP corresponded with the achieved reduction in cold storage time90. DCD grafts not exposed to cold storge but preserved with NMP over a prolonged period had excellent outcomes, comparable to porcine living donor kidney transplantation. Prolonged NMP could exhibit additional benefits: kidney transplantation would eventually be transformed into a semi-elective daytime procedure. In addition, portable NMP devices could allow to shorten or eliminate cold storage times, extend total preservation times and hence enable organ sharing over longer distances. This would be particularly meaningful in the context of hard-to place kidneys where the search for a recipient could be extended without adding cold storage time. The time added to the process would also be beneficial for “hard to transplant patients” such as patients with high panel reactive antibodies. Due to their immunological profile, the pool of donor kidneys that are immunologically compatible with the recipient is much smaller. Hence the travel time for kidneys would often be longer. Also, pretreatment of the recipient through e.g. immunoadsorption could be become possible with NMP. A corresponding measurable endpoint would be the waiting time for hard-to-transplant patients and the utilization rate of hard to place (HTP) kidneys. Such a concept is currently being tested by 34 Lives91. In a first clinical trial, HTP kidneys are machine perfused at their center and then shipped to a recipient site after testing and advanced matching (Clinicaltrials.gov ID NCT06263023). With a similar intention, the Organ Procurement and Transplant Network supports a protocol for “accelerated placement of hard-to-place kidneys”. In this study, participating centers will offer kidneys with a kidney donor profile index of 75% and higher (indicating that kidneys are of sub-optimal quality), to high priority kidney transplant candidates92.
These developments indicate that current principles in organ allocation may no longer be sufficient or suitable. In a recent viewpoint article, Pruett TA et al addressed the evolving regulatory and governing considerations, which arise because of emerging technologies for prolonged organ preservation. Since time plays such a key role in the current system and since “out of sequence allocation” evolved as a response triggered by the ponderous allocation system, kidney NMP but also other biopreservation technologies, which allow for prolonged preservation of organs may fundamentally change the allocation process93.
Another aim for NMP is enhancing the conditions during organ preservation. An improved preservation quality would ultimately translate into better organ survival and organ function. However, use of organ survival as an endpoint in kidney transplantation is problematic, because very good short-term outcomes with graft survival rates at 1 year of 95%+ are a routine. Furthermore, clinical studies with long observation periods are financially difficult to sustain. Hence the remaining targets for such trials are early measures of organ function. Possible targets and study endpoints include DGF, GFR and composite endpoints or parameters such as the iBOX94. Strength and weaknesses can be described for all such endpoints. A first larger controlled clinical trial was negative for DGF as a primary endpoint74. While several aspects, including the short duration of NMP time in this study are possible explanations, the study result indicates, that short end-ischemic NMP may not be enough. The determination if NMP replaces cold storage time, shortens cold storage time or is applied in addition to SCS/HMP with the purpose to assess and recondition kidneys needs further attention. All these use cases are plausible, but they follow different concepts and require different study designs. At the center of this consideration is the hypothesis, indicating what kidney NMP is expected to do. In essence, NMP is not miraculously improving kidneys. Instead, it adds a reperfusion cycle to the process and could potentially be harmful95 for instance by activating the innate immune system. In this regard, use cases are likely to include replacement of SCS/HMP time and safe prolongation of preservation. Through this process, the clock on kidney ischemia could be stopped. Together with the ability to assess kidneys, this could significantly impact the allocation process and result in more successful kidney transplantations. A key consideration in the selection of endpoints, is the patient viewpoint. The Standardized Outcomes in Nephrology (SONG)-Tx Initiative defines core patient reported outcome measures (PROM) for life participation in kidney transplant recipients. Further to allograft loss, cardiovascular disease, cancer and infection, life participation was the PROM of greatest importance to recipients, caregivers, and HCPs96.
Physical, emotional, and cognitive functioning, mental health, and health-related quality of life are relevant PROM domains to be considered in trials in kidney transplantation. The PROMs life participation, medication adherence, and symptoms and side effects are suitable secondary endpoints in interventional studies. The SF-36, the Sickness Impact Profile, and the WHO-QOL may be suitable instruments to capture the patient subjective impact of an intervention97
As simple as it seems, the determination of “successful kidney transplantation” is an important challenge and accurate determination is important in the context. In summary, the kidney utilization rate, the number of successful kidney transplantations, DGF, GFR, slope GFR, iBOX, patient survival, graft survival and questionnaires to capture physical and emotional outcomes are candidates for endpoints in clinical NMP trials.
Opportunities beyond preservation
Further to the immediate impact on mitigation of ischemia reperfusion injury, organ quality assessment and kidney utilization, the potential of kidney NMP is reaching far beyond these goals. The ability to preserve a kidney in a functioning state and responsive to interventions, holds the potential to apply various kinds of organ modifications and treatment to a kidney. This concept was first explored two decades ago where it was shown that ex vivo administration of the growth factors FGF1 and FGF2 could improve outcome in a model of canina kidney transplantation98. Current options that emerge include but are not limited to targeted organ repair, bioenergetic reconditioning, cell replacement and immunologic masking, rejuvenation, but also preclinical drug and technology testing. Such considerations are particularly interesting in the light of other emerging technologies such as gene editing, blood group modification, immunomodulation, xenotransplantation, supercooling and vitrification. In this context, NMP might serve as both an intermediate step for testing prior to transplantation and/or as a platform for intervention, repair and modification.
NMP may allow to expand the time for kidney evaluation and allocation. The two are interlinked, since the surgeon’s decision to accept an organ is depending on the information on organ quality and function. Hence expanding the preservation time and adding a profound volume of data on kidney function and viability to the current dataset may have a significant impact on the decision-making process and – in turn – on the allocation system. While some of the reasons for discard such as a donor history and biopsy findings such as chronic kidney disease cannot be immediately modified by NMP, several other causes for kidney discard could be altered by adding time and information to the allocation process (Fig. 3).
The current struggle in many regions, including the US, is that non-ideal kidneys are declined for dozens and hundreds of patients triggering a more directed approach to centers or surgeon willing to accept less than optimal kidneys. Considering that the analysis during NMP will add data and that data can be made available on digital platforms to all centers immediately, a more informed, immediate, direct and a competitive decision-making process may emerge. This would potentially increase utilization of extended criteria organs, result in better matching between donor and recipient and avoid the rush against time characterizing the current allocation process.
Once available, prolonged kidney NMP will open the door to new therapeutic opportunities such as cell therapy, gene modification or enhancing mitochondria function99. In lung perfusion models blood types have been modified during ex vivo perfusion resulting in universal donors100. IL10 upregulation was associated with a reduction of inflammatory response101. tPA administration during short-term ex vivo kidney perfusion removed intravascular fibrin deposition resulting in improved arterial flow and reduced vascular resistance102. Research is exploring the combination of NMP with gene editing technologies like CRISPR. The goal is to correct genetic defects in donor kidneys before transplantation, enhancing organ quality and reducing the risk of post-transplant complications. Evolving research on NMP facilitated gene editing to modify blood group antigens on kidney cells. This could potentially allow for more universal kidney transplantation by eliminating ABO blood group incompatibility103.
Improved transplant outcomes and reduced organ wastage will decrease healthcare costs related to chronic kidney disease and dialysis. Efficient organ use and more flexibility in the scheduling of surgical cases also helps optimize planning in transplant centers. In summary, NMP holds the potential to transform kidney transplantation practices through enhancement of feasibility and outcome and addressing some of the critical challenges hampering organ donation and transplantation today. The extension of the perfusion period may be needed for additional dedicated therapeutic interventions such as genetic modulations104,105, cellular therapy106,107, or pharmacological measures.
Future directions and outlook
The next steps on the way to clinical kidney NMP are the development and testing of perfusion devices and perfusion protocols that enable prolonged kidney preservation in clinical trials. Further to the existing commercially available instruments, devices with advanced automation running under stable conditions with little user input and comprehensive data recording are emerging. A clear definition of efficacy endpoints and careful crafting of the respective clinical trials is needed. This will open the door toward clinical routine use and collection of data on viability and safety.
Further to the isolated benefit of kidney NMP, the added value needs to be put in context with other developments in the field such as normothermic regional perfusion. For example, DGF could be significantly reduced through NRP and not serve as a relevant target for NMP development108. Cryopreservation techniques may help to cold store organs for prolonged periods of time. In all current scenarios, however, the ability to assess and treat organs is only foreseeable for NMP or subnormothermic perfusion. Rather than seeing the competition in the emerging technologies, the search for their synergy is warranted. As a reference, hypothermic oxygenated machine preservation and NMP emerged simultaneously in liver transplantation. While in the early phase, the combative approach emerged, the more recent research focusses on the respective benefit and a meaningful combination of the technologies109. Working from the experience in other organ NMP, the development of NMP biomarkers with predictive value for the outcome after kidney transplantation will require the collection of a large set of data, ideally through registries and real-world experience. Hence the greatest benefit of kidney NMP may eventually be the accurate assessment of organs during preservation. For this to be possible, biomarkers which help to determine the quality of a kidney and predict the outcome after transplantation need to be established.
Further to the pathway towards clinical realization, the development of kidney NMP as a platform for kidney treatment is equally appealing and relevant. Future efforts include the extension of preservation times and the assessment of techniques for kidney recondition, repair and treatment. This entails a long list of options, including endothelial cell stabilization or replacement, bioenergetic reconditioning, immune cell extraction/replacement or modification, gene editing, MHC and blood group editing as well as cell therapy and regeneration (Fig. 4).
NMP is challenging for all organs. It is costly, requires space, dedicated personnel and with many different perfusion protocols, the best perfusion strategy for each organ is still unknown. To establish NMP in kidney transplantation significant resources including funding, equipment, personnel and further research are needed. Hence a careful alignment between the unmet needs and endpoints with the business case and the industry expectations is advisable.
References
CDC. Chronic Kidney Disease in the United States, 2023. https://www.cdc.gov/kidney-disease/php/data-research/index.html (2024).
Liu, P. et al. Progression and regression of chronic kidney disease by age among adults in a population-based Cohort in Alberta, Canada. JAMA Netw. Open 4, e2112828 (2021).
ISN. Global Kidney Health Atlas. https://www.theisn.org/initiatives/global-kidney-health-atlas/ (2025).
Francis, A. et al. Chronic kidney disease and the global public health agenda: an international consensus. Nat. Rev. Nephrol. 20, 473–485 (2024).
Stel, V. S. et al. Supplemented ERA-EDTA Registry data evaluated the frequency of dialysis, kidney transplantation, and comprehensive conservative management for patients with kidney failure in Europe. Kidney Int 100, 182–195 (2021).
Zhang, Y. et al. Healthcare costs after kidney transplantation compared to dialysis based on propensity score methods and real world longitudinal register data from Sweden. Sci. Rep. 13, 10730 (2023).
Axelrod, D. A. et al. An economic assessment of contemporary kidney transplant practice. Am. J. Transpl. 18, 1168–1176 (2018).
OASH. Healthy People 2020. https://health.gov/our-work/national-health-initiatives/healthy-people/healthy-people-2020 (2025).
Kilambi, V. et al. Evaluation of opening offers early for deceased donor kidneys at risk of nonutilization. Clin. J. Am. Soc. Nephrol. 19, 233–240 (2024).
Bowring, M. G. et al. Kidney offer acceptance at programs undergoing a systems improvement agreement. Am. J. Transpl. 18, 2182–2188 (2018).
Mohan, S. et al. Factors leading to the discard of deceased donor kidneys in the United States. Kidney Int. 94, 187–198 (2018).
Ojo, A. O. et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J. Am. Soc. Nephrol. 12, 589–597 (2001).
Merion, R. M. et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 294, 2726–2733 (2005).
Schaapherder, A. F. et al. Donor characteristics and their impact on kidney transplantation outcomes: results from two nationwide instrumental variable analyses based on outcomes of donor kidney pairs accepted for transplantation. eClinicalMedicine 50, 101516 (2022).
Husain, S. A. et al. Characteristics and performance of unilateral kidney transplants from deceased donors. Clin. J. Am. Soc. Nephrol. 13, 118–127 (2018).
HRSA. OPTN/SRTR Annual Data Reports. https://srtr.transplant.hrsa.gov/ (2025).
Dahmane, D. et al. Retrospective follow-up of transplantation of kidneys from ‘marginal’ donors. Kidney Int 69, 546–552 (2006).
Wolfe, R. A. et al. Developing organ offer and acceptance measures: when ‘good’ organs are turned down. Am. J. Transpl. 7, 1404–1411 (2007).
Jochmans, I. et al. The prognostic value of renal resistance during hypothermic machine perfusion of deceased donor kidneys. Am. J. Transpl. 11, 2214–2220 (2011).
Mergental, H. et al. Transplantation of discarded livers following viability testing with normothermic machine perfusion. Nat. Commun. 11, 2939 (2020).
Gaurav, R. et al. Liver transplantation outcomes from controlled circulatory death donors: SCS vs in situ NRP vs ex situ NMP. Ann. Surg. 275, 1156–1164 (2022).
Quintini, C. et al. Transplantation of declined livers after normothermic perfusion. Surgery 171, 747–756 (2022).
Nasralla, D. et al. A randomized trial of normothermic preservation in liver transplantation. Nature 557, 50–56 (2018).
Chapman, W. C. et al. Normothermic machine perfusion of donor livers for transplantation in the United States: a randomized controlled trial. Ann. Surg. 278, e912–e921 (2023).
Watson, C. J. E. et al. Predicting early allograft function after normothermic machine perfusion. Transplantation 106, 2391–2398 (2022).
Panconesi, R. et al. Viability assessment in liver transplantation-what is the impact of dynamic organ preservation? Biomedicines 9, 161 (2021).
Krendl, F. J. et al. Normothermic liver machine perfusion at a large European center -real world outcomes following 238 applications. Ann. Surg. 47, 1184−1191(2025).
Cardini, B. et al. Clinical implementation of prolonged liver preservation and monitoring through normothermic machine perfusion in liver transplantation. Transplantation 104, 1917–1928 (2020).
Ardehali, A. et al. Ex-vivo perfusion of donor hearts for human heart transplantation (PROCEED II): a prospective, open-label, multicentre, randomised non-inferiority trial. Lancet 385, 2577–2584 (2015).
Schroder, J. N. et al. Transplantation outcomes with donor hearts after circulatory death. N. Engl. J. Med 388, 2121–2131 (2023).
Scheuer, S. E. et al. Heart transplantation following donation after circulatory death: expanding the donor pool. JHLT 40, 882–889 (2021).
Cypel, M. et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N. Engl. J. Med 364, 1431–1440 (2011).
Steen, S. et al. First human transplantation of a nonacceptable donor lung after reconditioning ex vivo. Ann. Thorac. Surg. 83, 2191–2194 (2007).
Smith, S. et al. Donor lung utilization for transplantation in the United States. JHLT 39, S374 (2020).
Moers, C. et al. Machine preservation trial study group. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 366, 770–771 (2012).
Moers, C. et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med 360, 7–19 (2009).
Jochmans, I. et al. Oxygenated versus standard cold perfusion preservation in kidney transplantation (COMPARE): a randomised, double-blind, paired, phase 3 trial. Lancet 396, 1653–1662 (2020).
Brasile, L. et al. Overcoming severe renal ischemia: the role of ex vivo warm perfusion. Transplantation 73, 897–901 (2002).
Dumas, S. J. et al. Phenotypic diversity and metabolic specialization of renal endothelial cells. Nat. Rev. Nephrol. 17, 441–464 (2021).
Wang, G. et al. Spatial dynamic metabolomics identifies metabolic cell fate trajectories in human kidney differentiation. Cell Stem Cell 29, 1580–1593.e7 (2022).
Rabbani, N. & Thornalley, P. J. Hexokinase-2 Glycolytic overload in diabetes and ischemia–reperfusion injury. Trends Endocrinol. Metab. 30, 419–431 (2019).
Oh, C. J. et al. Inhibition of pyruvate dehydrogenase kinase 4 ameliorates kidney ischemia-reperfusion injury by reducing succinate accumulation during ischemia and preserving mitochondrial function during reperfusion. Kidney Int. 104, 724–739 (2023).
Martin, J. L. et al. Succinate accumulation drives ischaemia-reperfusion injury during organ transplantation. Nat. Metab. 1, 966–974 (2019).
Bernardi, P. et al. Identity, structure, and function of the mitochondrial permeability transition pore: controversies, consensus, recent advances, and future directions. Cell Death Differ. 30, 1869–1885 (2023).
Vance, R. E. How DNA sensing drives Inflammation. N. Engl. J. Med. 391, 1456–1458 (2024).
Dondelinger, Y. et al. MLKL compromises plasma membrane integrity by binding to phosphatidylinositol phosphates. Cell Rep. 7, 971–981 (2014).
Kirita, Y. et al. Cell profiling of mouse acute kidney injury reveals conserved cellular responses to injury. Proc. Natl Acad. Sci. USA 117, 15874–15883 (2020).
Wu, W. K. et al. Delayed graft function and the risk of acute rejection in the modern era of kidney transplantation. Kidney Int. 88, 851–858 (2015).
Yarlagadda, S. G. et al. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol. Dial. Transpl. 24, 1039–1047 (2009).
Kim, D. W. et al. Financial impact of delayed graft function in kidney transplantation. Clin. Transpl. 34, e14022 (2020).
Maassen, H. et al. Prolonged organ extraction time negatively impacts kidney transplantation outcome. Transpl. Int 35, 10186 (2021).
Prudhomme T. et al. Cortex kidney tissue partial oxygen pressure depends on percentage of active oxygenation during oxygenated hypothermic machine perfusion. Artif. Organs. 49, 600−614 (2024).
Lucas-Ruiz, F. et al. Danger signals released during cold ischemia storage activate NLRP3 inflammasome in myeloid cells and influence early allograft function in liver transplantation. EBioMedicine 87, 104419 (2023).
Leng, Q. et al. Assessing donor kidney function: the role of CIRBP in predicting delayed graft function post-transplant. Front Immunol. 15, 1518279 (2025).
Kawamura, M. et al. Normothermic ex vivo kidney perfusion preserves mitochondrial and graft function after warm ischemia and is further enhanced by AP39. Nat. Commun. 15, 8086 (2024).
Juriasingani, S. et al. Subnormothermic perfusion with H2S donor AP39 improves DCD porcine renal graft outcomes in an ex vivo model of kidney preservation and reperfusion. Biomolecules 11, 446 (2021).
de Haan, MJA. et al. A cell-free nutrient-supplemented perfusate allows four-day ex vivo metabolic preservation of human kidneys. Nat. Commun. 15, 3818 (2024).
de Haan MJA. et al. Normothermic human kidney preservation drives iron accumulation and ferroptosis. Nat Commun 16, 5420 (2025).
Abou Taka, M. et al. Evaluating the effects of kidney preservation at 10 °C with Hemopure and sodium thiosulfate in a rat model of syngeneic orthotopic kidney transplantation. Int. J. Mol. Sci. 25, 2210 (2024).
Juriasingani, S. et al. Evaluating the effects of subnormothermic perfusion with AP39 in a novel blood-free model of ex vivo kidney preservation and reperfusion. Int. J. Mol. Sci. 22, 7180 (2021).
Theurl, I. et al. On-demand erythrocyte disposal and iron recycling requires transient macrophages in the liver. Nat. Med 22, 945–951 (2016).
Messner, F. et al. Development of an automated multi-sensor normothermic kidney perfusion device for ex-vivo preservation and assessment. Transplantation 108, 396 (2024).
Hunter, J. P. et al. Assessment of mitochondrial function and oxygen consumption measured during ex vivo normothermic machine perfusion of injured pig kidneys helps to monitor organ viability. Transpl. Int 35, 10420 (2022).
Schutter, R. et al. Magnetic resonance imaging assessment of renal flow distribution patterns during ex vivo normothermic machine perfusion in porcine and human kidneys. Transpl. Int 34, 1643–1655 (2021).
Kidney. XVIVO https://www.xvivogroup.com/organ-perfusion/kidney/ (2025).
EBERS. Medical Technology SL. https://ebersark.life/ (2025).
Apheresis. PerLife ®. Aferetica - Aferesi Come Terapia. https://www.aferetica.com/sistemi-terapeutici/perlife-tm/ (2025).
Hosgood, S. A. & Nicholson, M. L. First in man renal transplantation after ex vivo normothermic perfusion. Transplantation 92, 735–738 (2011).
Nicholson, M. L. & Hosgood, S. A. Renal transplantation after ex vivo normothermic perfusion: the first clinical study. Am. J. Transpl. 13, 1246–1252 (2013).
Minor, T. et al. First-in-man controlled rewarming and normothermic perfusion with cell-free solution of a kidney prior to transplantation. Am. J. Transpl. 20, 1192–1195 (2020).
Zlatev, H. et al. Clinical use of controlled oxygenated rewarming of kidney grafts prior to transplantation by ex vivo machine perfusion. A pilot study. Eur. J. Clin. Invest 52, e13691 (2022).
Rijkse, E. et al. Safety and feasibility of 2 h of normothermic machine perfusion of donor kidneys in the eurotransplant senior program. BJS Open 5, zraa024 (2021).
Mazilescu, L. I. et al. Normothermic ex vivo kidney perfusion for human kidney. Transplant. First North Am. Results Transplant. 106, 1852–1859 (2022).
Hosgood, S. A. et al. Normothermic machine perfusion versus static cold storage in donation after circulatory death kidney transplantation: a randomized controlled trial. Nat. Med. 29, 1511–1519 (2023).
Hosgood, S. A. & Nicholson, M. L. The first clinical case of intermediate ex vivo normothermic perfusion in renal transplantation. Am. J. Transpl. 14, 1690–1692 (2014).
Hameed, A. M. Normothermic ex vivo perfusion before transplantation of the kidney (NEXT-kidney): a single-center, nonrandomized feasibility study. Transplantation 109, 881−889 (2024).
Dumbill, R. et al. Normothermic kidney perfusion phase 1 – a clinical trial of up to 24-hour normothermic machine perfusion prior to transplantation. Am. J. Transplant. 23, S1–S6 (2023).
Weissenbacher, A. et al. Twenty-four-hour normothermic perfusion of discarded human kidneys with urine recirculation. Am. J. Transpl. 19, 178–192 (2019).
Weissenbacher, A. et al. Forty-eight hours of normothermic kidney preservation applying urine recirculation. Artif. Organs 46, 710–714 (2022).
Messner, F. et al. 48 h Normothermic machine perfusion with urine recirculation for discarded human kidney grafts. Transpl. Int. 36, 11804 (2023).
Hosgood, S. A. et al. Normothermic machine perfusion for the assessment and transplantation of declined human kidneys from donation after circulatory death donors. Br. J. Surg. 105, 388–394 (2018).
Hosgood, S. A. et al. Successful transplantation of human kidneys deemed untransplantable but resuscitated by ex vivo normothermic machine perfusion. Am. J. Transpl. 16, 3282–3285 (2016).
Nicholson, M. & Hosgood, S. Preoperative assessment of renal transplant ureteric blood supply using ex vivo normothermic perfusion. Transplantation 99, e166 (2015).
Pearson, R. et al. Living donor kidney transplant following nephrectomy for renal artery stenosis with arterial reconstruction and viability assessment using ex vivo normothermic perfusion. BMJ Case Rep. 14, e245273 (2021).
Georgiades, F. et al. Use of ex vivo normothermic machine perfusion after normothermic regional perfusion to salvage a poorly perfused DCD kidney. Am. J. Transpl. 19, 3415–3419 (2019).
Pearson, R. et al. Viability assessment and utilization of declined donor kidneys with rhabdomyolysis using ex vivo normothermic perfusion without preimplantation biopsy. Am. J. Transpl. 21, 1317–1321 (2021).
Home. 34 Lives. https://34lives.com/ (2025).
Medical Devices. Guidance on Classification of Medical Devices. https://health.ec.europa.eu/system/files/2021-10/mdcg_2021-24_en_0.pdf (2021).
Health, C. for D. & R. Classify Your Medical Device. https://www.fda.gov/medical-devices/overview-device-regulation/classify-your-medical-device (2023).
Kaths, J. M. et al. Continuous normothermic ex vivo kidney perfusion improves graft function in donation after circulatory death pig kidney. Transplant. Transplant. 101, 754–763 (2017).
WCG CenterWatch. A Central Preservation and Assessment Service to Optimize Donor Kidney Allocation. https://www.centerwatch.com/clinical-trials/listings/NCT06263023/a-central-preservation-and-assessment-service-to-optimize-donor-kidney-allocation (2025).
OPTN. Accelerated Placement of Hard-to-Place Kidneys. https://optn.transplant.hrsa.gov/professionals/improvement/improving-organ-usage-and-placement-efficiency/protocols-for-expedited-placement-variance/accelerated-placement-of-hard-to-place-kidneys/ (2025).
Pruett, T. L. et al. Governing new technologies that stop biological time: Preparing for prolonged biopreservation of human organs in transplantation. Am. J. Transpl. 25, 269–276 (2025).
Klein, A. et al. Qualifying a novel clinical trial endpoint (iBOX) predictive of long-term kidney transplant outcomes. Am. J. Transpl. 23, 1496–1506 (2023).
Jager, N. M. et al. Complement is activated during normothermic machine perfusion of porcine and human discarded kidneys. Front. Immunol. 13, 831371 (2022).
Tong, A. et al. Implementing core outcomes in kidney disease: report of the standardized outcomes in Nephrology (SONG) implementation workshop. Kidney Int 94, 1053–1068 (2018).
Tong, A. et al. Patient-reported outcomes as endpoints in clinical trials of kidney transplantation interventions. Transpl. Int 35, 10134 (2022).
Brasile, L. et al. Potential of repairing ischemically damaged kidneys ex vivo. Transpl. Proc. 37, 375–376 (2005).
Pühringer, M. et al. Normothermic machine perfusion of kidney grafts: devices, endpoints, and clinical implementation. Eur. Surg. 57, 88–99 (2025)
Wang, A. et al. Ex vivo enzymatic treatment converts blood type A donor lungs into universal blood type lungs. Sci. Transl. Med. 14, eabm7190 (2022).
Mesaki, K. et al. Immunomodulation of the donor lung with CRISPR-mediated activation of IL-10 expression. J. Heart Lung Transpl. 42, 1363–1377 (2023).
DiRito, J. R. et al. Lysis of cold-storage-induced microvascular obstructions for ex vivo revitalization of marginal human kidneys. Am. J. Transpl. 21, 161–173 (2021).
MacMillan, S. et al. Enzymatic conversion of human blood group A kidneys to universal blood group O. Nat. Commun. 15, 2795 (2024).
Bonaccorsi-Riani, E. et al. Delivery of genetic load during ex situ liver machine perfusion with potential for CRISPR-Cas9 gene editing: an innovative strategy for graft treatment. HBPD Int. 20, 503–505 (2021).
Lascaris, B. et al. Normothermic liver machine perfusion as a dynamic platform for regenerative purposes: What does the future have in store for us? J. Hepatol. 77, 825–836 (2022).
eGenesis. eGenesis Presents Preclinical Data Demonstrating Recipient Survival and Compatibility With Genetically Engineered Porcine Kidneys at 2023 IPITA-IXA-CTRMS Joint Conference. https://egenesisbio.com/press-releases/egenesis-presents-preclinical-data-demonstrating-recipient-survival-and-compatibility-with-genetically-engineered-porcine-kidneys-at-2023-ipita-ixa-ctrms-joint-conference/ (2025).
Thompson, E. R. et al. Cell therapy during machine perfusion. Transpl. Int. 34, 49–58 (2021).
Padilla, M. et al. Improved short-term outcomes of kidney transplants in controlled donation after the circulatory determination of death with the use of normothermic regional perfusion. Am. J. Transpl. 21, 3618–3628 (2021).
van Leeuwen, O. B. et al. Transplantation of high-risk donor livers after ex situ resuscitation and assessment using combined hypo- and normothermic machine perfusion: a prospective clinical trial. Ann. Surg. 270, 906–914 (2019).
Acknowledgements
TR is supported by the Novo Nordisk Foundation Center for Stem Cell Medicine (reNEW, supported by Novo Nordisk Foundation grant (NNF21CC0073729)) and is funded by the European Union by ERC grant (SPARK 101140863). We thank Manon Zuurmond in helping design the illustrations.
Author information
Authors and Affiliations
Contributions
T.R. contributed to the development of the outline, took a key role in the writing and production of figures. S.H. contributed to conceptualization, writing, and reviewing of the final manuscript. T.M. contributed to conceptualization, writing, and reviewing of the final manuscript. M.S. contributed to conceptualization, writing, and reviewing of the final manuscript. A.W. contributed to conceptualization, writing, and reviewing of the final manuscript. H.L. contributed to conceptualization, writing, and reviewing of the final manuscript. S.S. engaged the group of authors, developed the outline, coordinated the writing and the production of figures and tables, performed and edited the revisions.
Corresponding author
Ethics declarations
Competing interests
S.S. has the following disclosures: Grants/Research Support: Chiesi, Neovii, Organ Recovery; Speakers Bureau/Honoraria: Sanofi, OrganOx, Chiesi, Astra Zenica, XVIVO; Consulting Fees: Merck, Atara, NefroHealth, ITB, iCoat Medical, Dialectica, Johnson & Johnson, Sanofi, MSD; None of these represents a conflict of interest, but the interaction with companies in the perfusion industry informed the thinking and the understanding of the field. H.L. is part-time Chief Scientific Officer of 34Lives, PBC, Speakers/consulting honoraria: Neovii, Astra Zenica, NefroHealth. T.R., S.H., T.M., M.S. and A.W. have no competing interests to declare.
Peer review
Peer review information
Nature Communications thanks Germaine Wong, and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rabelink, T.J., Hosgood, S., Minor, T. et al. Opportunities and challenges with the implementation of normothermic machine perfusion in kidney transplantation. Nat Commun 16, 6883 (2025). https://doi.org/10.1038/s41467-025-60410-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60410-3