Abstract
Diabetes is common in patients with chronic obstructive pulmonary disease. Sodium-glucose co-transporter-2 inhibitors are effective in treating type 2 diabetes and provide benefits for conditions like cardiovascular and kidney diseases. We use data from multiple institutions and countries to evaluate their role in patients with chronic obstructive pulmonary disease and diabetes. This study includes chronic obstructive pulmonary disease patients with diabetes who are newly prescribed sodium-glucose co-transporter-2 inhibitors or dipeptidyl peptidase-4 inhibitors between January 1, 2013, and August 25, 2024. The primary outcome is all-cause mortality. The results show that the sodium-glucose co-transporter-2 inhibitors group has a lower risk of all-cause mortality compared to the dipeptidyl peptidase-4 inhibitors group (hazard ratio, 0.757; 95% confidence interval, 0.716-0.801). It also shows significantly lower risks of all-cause hospitalization (hazard ratio, 0.864; 95% confidence interval, 0.845-0.884), exacerbation (hazard ratio, 0.924; 95% confidence interval, 0.888-0.962), pneumonia, upper respiratory infections, bronchitis, and major cardiovascular events.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent respiratory condition characterized by cough, dyspnea, and airflow limitation, affecting both males and females equally across the globe1. It is estimated that approximately 10 percent of individuals aged 40 years or older have COPD, although the prevalence varies between countries and tends to increase with age2,3,4. Prior to the COVID-19 pandemic, COPD was the third leading cause of death worldwide, underscoring its significant impact on global health5. Due to its high prevalence and chronic nature, COPD imposes a substantial burden on healthcare systems, resulting in frequent clinician visits, multiple hospitalizations due to acute exacerbations, and the necessity for chronic therapy6.
In addition, patients with COPD could have a two to five times higher risk of developing cardiovascular disease, with nearly 20% experiencing cardiovascular-related deaths. Moreover, this risk of cardiovascular events increases with the severity of COPD7,8. Therefore, it is crucial not only for controlling the respiratory condition but also for improving cardiovascular outcomes for patients with COPD9.
SGLT2 inhibitors (SGLT2is) offer multiple benefits, primarily in treating type 2 diabetes mellitus (T2DM), but also potentially for other conditions such as cardiovascular disease, chronic kidney disease, and obesity. Experimental data further supports SGLT2is’ anti-inflammatory effects. In cellular and mouse models, SGLT2i reduced pro-inflammatory cytokines (IL-1, IL-6, TNF-α) through autophagy-dependent mechanisms, as evidenced by the reversal of effects when autophagy was blocked with 3-methyladenine. This process appears mediated through AMP-activated protein kinase phosphorylation and the NF-κB pathway. These findings suggest SGLT2is’ anti-inflammatory properties extend beyond their glucose-lowering effects, potentially benefiting both acute and chronic inflammatory conditions10. Recent clinical studies suggest that SGLT2is may help reduce the risk of COPD exacerbations, adding to their potential benefits beyond diabetes management11,12. One cohort study reported that SGLT2i might be associated with a reduced risk of developing obstructive airway disease (hazard ratio [HR], 0.65; 95% CI, 0.54–0.79) and a lower exacerbation rate (HR, 0.54; 95% CI, 0.36–0.83) among patients with type 2 diabetes mellitus (T2DM)12. Another cohort study demonstrated the similar findings that SGLT2i might reduce the risk of severe exacerbations in COPD patients with T2DM (HR, 0.62, 0.48–0.81)11. However, the impact of SGLT2i on the outcomes of COPD patients remains unclear. Hence, this study was undertaken to evaluate the association between SGLT2i use and the risk of both COPD-related clinical outcomes and major adverse cardiovascular events (MACEs) in patients with COPD and T2DM.
Results
Demographic characteristics of included patients
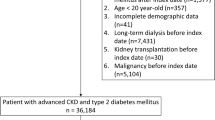
Based on screening of the TriNetX platform across 128 healthcare organizations (HCOs) from 17 countries on September 2, 2024, 1,009,463 patients with COPD and T2DM were identified, of which 91,993 and 95,048 were new users of SGLT2i and DPP-4i, respectively (Fig. 1). After excluding those with prior or concomitant use of SGLT2i and DPP-4i, and patients with malignant neoplasms, 58,899 and 41,244 patients were classified into SGLT2i and DPP-4i groups, respectively.
Table 1 shows the comparison between SGLT2i and DPP-4i groups before and after PSM. Before matching, the SGLT2i group was younger than the DPP-4i group (65.8 ± 10.8 years vs. 68.3 ± 11.6 years), and the distribution of sex and race also differed between groups. Additionally, BMI was higher in the SGLT2i group than the DPP-4i group (34.2 ± 8.5 vs. 32.4 ± 8.2), and the SGLT2i group had a higher prevalence of individuals with BMI ≥ 25 kg/m2. Furthermore, the SGLT2i group had a higher prevalence of HbA1c ≥ 8% than the DPP-4i group (43.6% vs. 37.3%).
Compared to the DPP-4i group, the SGLT2i group had a higher prevalence of overweight/obesity, nicotine dependence, hypertension, hyperlipidemia, chronic liver disease, congestive heart failure, ischemic heart disease, hypertensive disease, pulmonary heart disease, and obstructive sleep apnea. Lastly, the SGLT2i group had more patients with concomitant use of insulin, biguanides, and glucagon-like peptide-1 receptor agonists, but fewer using sulfonylureas than the DPP-4i group. Overall, PSM yielded 41,244 matched patients in each cohort, with standardized differences in all covariates between groups less than 0.1 (Table 1).
Primary and secondary outcomes
During follow-up, the SGLT2i group was associated with a lower risk of all-cause mortality than the DPP-4i group (HR, 0.757; 95% CI, 0.716–0.801, Table 2). Survival analysis showed a higher cumulative incidence of mortality in the DPP-4i group (log-rank test, p < 0.001) (Fig. 2).
Compared to the DPP-4i group, the SGLT2i group was also associated with significantly lower risks of all-cause hospitalization (HR, 0.864; 95% CI, 0.845–0.884), COPD exacerbation (HR, 0.924; 95% CI, 0.888–0.962), pneumonia (HR, 0.728; 95% CI, 0.697–0.760), acute upper respiratory tract infection (HR, 0.863; 95% CI, 0.806–0.923), bronchitis (HR, 0.710; 95% CI, 0.653–0.772), and MACE (HR, 0.918; 95% CI, 0.868–0.970) (Table 2).
Stratified and sensitivity analysis
The lower risk of all-cause mortality in the SGLT2i group compared to the DPP-4i group was observed in all stratified analyses, including both males and females, adults and older patients, and those with/without underlying diseases such as MACEs, overweight and obesity, and a history of prior exacerbation (all p < 0.01) (Table 3). Similar findings were observed for all three types of SGLT2is—canagliflozin, dapagliflozin, and empagliflozin (all p < 0.0001), with no significant differences in their effects (all p-values for interaction >0.05, Table S4). Furthermore, the survival benefits of SGLT2i remained consistent across different types of inhaled bronchodilators among patients with COPD (all p < 0.05) (Table 3). Additional landmark analyses and sensitivity tests, conducted using different models, varying enrollment periods, and assessments of medication compliance, demonstrated consistent results (Tables S5–S9). Lastly, compared to sulfonylureas, SGLT2i was associated with lower mortality (HR 0.816; 95% CI, 0.774–0.860; p < 0.0001, Table S10).
Discussion
Our study used TriNetX which enrolled approximately 150 million patients across 120 healthcare organizations worldwide found that, compared with DPP-4i, patients with COPD and T2DM received SGLT2i were associated with a lower risk of all-cause mortality. Moreover, SGLT2i associated survival benefits remained consistent across different sensitivity analyses. In addition to mortality, SGLT2i was associated with a lower risk of all-cause hospitalization, COPD exacerbation, pneumonia, upper respiratory tract infection, and MACE, compared to DDP-4i in this study. All these findings indicate the clinical benefit of SGLT2i for patients with COPD and T2DM.
For our primary outcome of all-cause mortality, we observed a hazard ratio of 0.757 (95% CI: 0.716–0.801). This substantial mortality benefit is particularly significant as few existing treatments have demonstrated survival improvements in COPD patients. The reduction in COPD exacerbations can significantly impact patient quality of life and slow disease progression. Similarly, reduction in MACE, while numerically smaller than the mortality benefit, represents a crucial advantage given the high cardiovascular mortality in COPD patients. These findings suggest that SGLT2i offering benefits beyond glycemic control to improve key respiratory and cardiovascular outcomes.
Clinical studies on the association of SGLT2i use with all-cause mortality, pneumonia and MACE in patient with COPD are limited. A population-based cohort study11 used United Kingdom Clinical Practice Research Datalink found that compared with sulfonylureas, SGLT2i were linked to a 38% reduction in the risk of severe exacerbations (2.4 versus 3.9 events per 100 person-years; hazard ratio 0.62, 95% CI 0.48–0.81). From our study, we found that compared with DPP-4i, SGLT2i not only associated with reduce acute exacerbation but also reduce mortality, hospitalization and MACE. Another study12 used electronic medical database from Hong Kong to investigate the association of SGLT2i user and DPP-4i user in patients with concomitant DM and obstructive airway disease, which included asthma and COPD and found that SGLT2i user had lower risk of exacerbation. There are some limitations in the study12. While COPD and asthma both present with similar symptoms—such as dyspnea, cough, and sputum production—that can make diagnosis challenging, they differ markedly in their pathogenesis, disease progression, prognosis, and treatment options. Because of their heterogeneous nature, varying clinical courses, and distinct treatment approaches and outcomes, asthma and COPD should be addressed separately13. Their database also lacks complete records on medication treatments, the severity of obstructive pulmonary disease, and the history of exacerbations prior to the index date in COPD patients, which is a confounding factor that significantly impacts the outcome. Their PSM accounted for major comorbidities and associated drug use, focusing on ICS/LABA. However, they did not address the use of LABA/LAMA or ICS/LABA/LAMA therapies. In their study, to differentiate the severity of obstructive pulmonary disease, their propensity score matching model utilized the maintenance therapy for obstructive pulmonary disease prior to the index date. However, they did not account for the history of exacerbations before the index date in COPD patients, which could indicate the risk of future exacerbations. In our study, we adjusted for various types of inhalation medications, including LABA, LAMA, LABA + LAMA, ICS + LABA, and ICS + LAMA + LABA. We also matched for COPD exacerbation history before the index date.
The exact mechanism linking SGLT2i to COPD exacerbations is not yet fully understood. However, one possible explanation is their anti-inflammatory properties. Research in animal models has demonstrated that SGLT2i can mitigate lung injury caused by lipopolysaccharide-induced acute lung injury and reduce inflammation by decreasing levels of IL-1β, IL-6, and TNF-α, in bronchoalveolar lavage fluid and serum. Furthermore, flow cytometry analyses of bronchoalveolar lavage fluid cells and bone marrow-derived macrophages have shown that SGLT2i can influence the balance between classically activated (M1) and alternatively activated (M2) macrophages, inhibiting M1 macrophages and promoting a shift towards the M2 phenotype. These observations suggest that SGLT2is may exert their anti-inflammatory effects by modulating alveolar macrophage polarization14. Numerous clinical and experimental studies have shown that SGLT2i combat inflammation and oxidative stress by modifying Ca2+ signaling and decreasing the production of reactive oxygen species, fibrosis, and other inflammatory processes, which are crucial molecular targets for these drugs14. SGLT2is also enhance phosphorylation of AMP-activated protein kinase and acetyl-CoA carboxylase in skeletal muscle and boost fibroblast growth factor 21 levels in the liver and plasma. They further stimulate the expression of uncoupling protein 1 in brown fat and both inguinal and epididymal white adipose tissue. Furthermore, research has demonstrated that empagliflozin effectively reduces the accumulation of M1-polarized macrophages, while simultaneously promoting the differentiation and development of the anti-inflammatory M2 macrophage phenotype in both white adipose tissue and the liver15. This further leads to reduced plasma TNFα levels and decreased obesity-related chronic inflammation. Additionally, this is accompanied by lower levels of pro-inflammatory cytokines, such as C-reactive protein, interleukin-6, and TNF-α14, along with increased levels of adiponectin16. SGLT2i also exhibit a significant effect on reducing low-grade inflammation, likely by lowering uric acid and insulin levels. This anti-inflammatory effect aligns with other proposed mechanisms that may account for the observed benefits of SGLT2is on cardiovascular and renal health17. Consequently, SGLT2is are believed to enhance COPD outcomes through their pronounced anti-inflammatory effects. Beyond COPD, SGLT2i may also benefit allergic asthma through immunomodulation, as demonstrated in both in vitro and animal studies. In human immune cells, SGLT2i treatment significantly inhibited mast cell degranulation, measured by β-hexosaminidase activity. In a mouse model, SGLT2i reduced ovalbumin-induced airway hyper-responsiveness and decreased inflammatory cell counts (lymphocytes and eosinophils) in bronchoalveolar lavage fluid. The treatment also lowered pro-inflammatory cytokine expression (IL-4, IL-5, IL-13) and suppressed airway inflammation and mucin production, suggesting potential therapeutic applications in asthma18. Moreover, several studies have investigated the anti-inflammatory mechanisms and biomarkers of SGLT2i in human models. A 52-week study in diabetes patients receiving SGLT2i treatment showed significant changes in serum biomarkers compared to glimepiride treatment: a 22% reduction in median serum IL-6 levels, a 25% decrease in serum leptin, and a 17% increase in median serum adiponectin. These findings suggest that SGLT2i may modulate these serum markers to enhance adipose tissue function, potentially improving insulin sensitivity and reducing cardiovascular risk19. A subsequent clinical trial examined SGLT2i’s impact on the inflammatory profile of patients with both diabetes and coronary artery disease. When added to standard antihyperglycemic treatment, SGLT2i led to substantial reductions in pro-inflammatory biomarkers compared to placebo. Specifically, patients receiving SGLT2i treatment showed significantly lower levels of interleukin 6, interleukin 1β, and high-sensitivity C-reactive protein. The SGLT2i-treated group also demonstrated enhanced antioxidant defenses, with elevated levels of superoxide dismutase activity, glutathione, and total antioxidant capacity. Furthermore, these patients showed improved levels of reactive oxygen species and reduced P-selectin antigen expression on platelet surfaces. These findings collectively suggest that SGLT2i can reduce inflammation, decrease platelet activity, and ameliorate oxidative stress—effects that may be particularly beneficial for patients with concurrent diabetes and cardiovascular disease20.
Our study carries important clinical implications, especially for patients who suffer from both COPD and DM, a prevalent comorbidity. DM has been documented to adversely affect lung tissue and overall pulmonary condition through inflammatory mechanisms, leading to a considerable inpatient burden among COPD patients. This burden includes an elevated risk of severe complications such as pneumonia, stroke, and respiratory failure21. Consequently, it is essential to identify antidiabetic medications that can provide protective benefits against these exacerbations, as well as reduce mortality in individuals with COPD and diabetes.
The effects of SGLT2i on the cardiovascular and renal systems have been well-documented, their potential role in the respiratory system remains largely underexplored. This study suggests that SGLT2i could play a crucial role in the management of COPD with T2DM, highlighting the need for further prospective research to fully understand their impact on respiratory health.
The strengths of our study include a large cohort of patients with COPD and T2DM sourced from TriNetX, which is the global repository of real-world data, encompassing multiple institutions and countries. This allows our findings to be generalizable to the diverse demographic representation within our COPD and diabetes study cohort, which includes various racial/ethnic groups and age ranges. We employed an active comparator design using DPP-4i to highlight the promising effects of SGLT2i in patients with both COPD and T2DM. Despite the emergence of new treatment options in recent decades, mortality rates attributable to COPD have not improved as significantly as those for other chronic diseases. To date, only two studies22,23 have demonstrated a reduction in mortality for COPD patients through triple bronchodilator therapy. Thus, our study may provide valuable insights into the potential for decreased mortality in patients with COPD and T2DM who are treated with SGLT2i therapy.
This study acknowledges several limitations. Firstly, the data we accessed lacked specific information about the study populations’ geographical locations and healthcare settings. This limitation stems from the structure of the database, which only provides aggregated data without these detailed characteristics. Secondly, the prescription data may not accurately reflect actual medication adherence, as the records of prescribed medication do not always correlate with patients’ actual consumption of the drugs. Additionally, our study was retrospective and observational in nature, relying solely on the available electronic health records and hospitalization data. Even with PSM, may still be influenced by unmeasured confounders such as differences in disease severity, healthcare quality or smoking status. Lastly, we used PSM within the TriNetX platform to obtain two comparable groups, and then applied a standard Cox proportional hazards model to estimate hazard ratios. While the TriNetX platform has limitations regarding advanced statistical methods, such as sandwich robust standard error estimation or bootstrap confidence intervals, we were able to obtain reliable effect estimates using the available standard approaches. As a result, while we observed favorable effects of SGLT2i in patients with COPD, we cannot completely rule out the possibility that other unmeasured factors might have contributed to these outcomes.
We observed that the use of SGLT2i was associated with a significant reduction in several adverse outcomes compared to the use of DPP-4i. Specifically, SGLT2i use was linked to a decreased risk of all-cause mortality, overall hospitalization, COPD exacerbations, pneumonia, upper airway infections, and MACEs in clinical settings. This suggests that SGLT2i may offer substantial benefits in managing these conditions, highlighting their potential advantages over DPP-4i in this patient population. However, further prospective study is warranted to validate our findings.
Methods
The retrospective cohort study compared the effect of SGLT2i and dipeptidyl peptidase-4 inhibitor (DPP-4i) on the outcomes of patients with COPD and T2DM. The study used data from the TriNetX Analytics network platform, a global federated health research network that provides access to electronic medical records (EMRs) from approximately 150 million patients across 120 healthcare organizations worldwide24. TriNetX offers secure, web-based, real-time access to patient records from hospitals, primary care, and specialty treatment providers, encompassing diverse geographic and ethnic populations. This study was approved by the institutional review board (IRB) of the Chi Mei Medical Center (IRB No. 11310-J01). Since patient identification information was not provided on the TriNetX platform, the IRB waived the requirement for informed consent.
Study population and definition of eligible patients
The retrospective cohort study enrolled COPD patients with T2DM who were newly prescribed either the SGLT2i or DPP-4i between January 01, 2013, and August 25, 2024. The study period began in 2013, aligning with the FDA’s approval of SGLT2i25. The index date was defined as the first prescription of SGLT2i or DPP-4i.
Eligibility criteria included COPD patients with T2DM who aged 18 years or older. The diagnosis of COPD was based on the International Classification of Diseases, Tenth Edition, Clinical Modification (ICD-10-CM) diagnostic code J41, J42, J43, or J44, while T2DM was identified with the ICD-10-CM code E11. The COPD diagnosis should be recorded within 1 year before or up to 1 year after the T2DM diagnosis. All patients were required to have at least two EMRs documented during the study period. Participants were then divided into two groups based on their medication use within 1 year after any instance of T2DM diagnosis. The SGLT2i group included patients who were new users of SGLT2i, while the DPP-4i group included patients who were new users of DPP4i.
We excluded patients who had priorly used SGLT2i or DPP-4i before the index date, those who received a combination of these two types of drugs, and those with a history of malignant neoplasms (Table S1).
Covariates
Covariates were selected based on clinical relevance, focusing on significant comorbidities and risk factors that could influence mortality of patients with COPD11,26,27,28,29,30. The covariates and the baseline characteristics, including age, sex, race, body mass index (BMI), hemoglobin A1c (HbA1c), comorbidities, and anti-diabetic medications were recorded for both groups within 1 year before the index date (Table S2).
Outcomes
The primary outcomes were the risks of all-cause mortality. Secondary outcomes included the risks of all-cause hospitalization, all-cause emergency department (ED) visit, exacerbation, pneumonia, acute upper respiratory infection, acute lower respiratory infection, bronchitis and MACEs. MACEs included acute myocardial infraction, stroke, heart failure, ventricular arrhythmia and cardiac arrest. The patients were followed up from the first day after the index date until the final clinical visit, death, or 1 years from the index date (Table S3).
Statistical analysis
Baseline characteristics were described using means and standard deviations (SDs) for continuous variables, numbers and percentages for dichotomous variables. Propensity score matching (PSM) was conducted to ensure balanced covariates between the two groups at baseline, employing a greedy nearest-neighbor algorithm with a caliper width of 0.1 pooled SDs. Adequate matching was indicated by standardized differences of less than 0.1 between the groups. After PSM, the survival analyses were conducted using the Kaplan–Meier method. A log-rank test assessed differences in survival distributions between groups. HR for the outcomes were estimated using Cox regression model. Two-tailed P values less than 0.05 were considered statistically significant.
Stratified and sensitivity analysis
Stratified analyses were performed to explore variations in the primary outcome across different categories, including age, gender, the history of overweight and obesity, MACEs, COPD exacerbation, and different types of inhaled bronchodilator. Further analyses examined variations across different types of SGLT2i, including empagliflozin, dapagliflozin, and canagliflozin, as well as among different inhaled bronchodilators for COPD treatment, such as inhaled corticosteroid (ICS)/ long-acting beta2-agonist (LABA)/ long-acting muscarinic antagonist (LAMA), LABA/LAMA, ICS/LABA, and LAMA.
Additionally, we conducted landmark analyses, starting the follow-up period at one day, one month, three months, and six months after the index date, continuing until one year31. Moreover, multiple sensitivity analyses were performed using different models, varying enrollment periods, and medication compliance. Lastly, we compared the effects of SGLT2i with those of another commonly used antidiabetic medication—sulfonylureas.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available in the article and its Supplementary information. Source data are provided as Source Data file and may be obtained from the corresponding authors upon request. Patient data can also be access on TriNetx on https://trinetx.com/. Source data are provided with this paper.
References
Agustí, A. et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am. J. Respir. Crit. Care Med. 207, 819–837 (2023).
Ford, E. S. et al. Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988-1994 to 2007-2010. Chest 143, 1395–1406 (2013).
Burney, P. et al. Chronic obstructive pulmonary disease mortality and prevalence: the associations with smoking and poverty–a BOLD analysis. Thorax 69, 465–473 (2014).
Ford, E. S. et al. COPD surveillance–United States, 1999-2011. Chest 144, 284–305 (2013).
World Health Organization. Chronic obstructive pulmonary disease (COPD). 2024; https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
Buist, A. S. et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 370, 741–750 (2007).
Sin, D. D., Anthonisen, N. R., Soriano, J. B. & Agusti, A. G. Mortality in COPD: Role of comorbidities. Eur. Respir. J. 28, 1245–1257 (2006).
Curkendall, S. M. et al. Chronic obstructive pulmonary disease severity and cardiovascular outcomes. Eur. J. Epidemiol. 21, 803–813 (2006).
Hurst, J. R. & Gale, C. P. MACE in COPD: Addressing cardiopulmonary risk. Lancet Respir. Med 12, 345–348 (2024).
Xu, C. et al. Canagliflozin exerts anti-inflammatory effects by inhibiting intracellular glucose metabolism and promoting autophagy in immune cells. Biochem Pharm. 152, 45–59 (2018).
Pradhan, R. et al. Novel antihyperglycaemic drugs and prevention of chronic obstructive pulmonary disease exacerbations among patients with type 2 diabetes: population based cohort study. Bmj 379, e071380 (2022).
Au, P. C. M. et al. Association of sodium-glucose cotransporter 2 inhibitor vs dipeptidyl peptidase-4 inhibitor use with risk of incident obstructive airway disease and exacerbation events among patients with type 2 diabetes in Hong Kong. JAMA Netw. Open 6, e2251177 (2023).
Yayan, J. & Rasche, K. Asthma and COPD: Similarities and differences in the pathophysiology, diagnosis and therapy. Adv. Exp. Med. Biol. 910, 31–38 (2016).
Lin, F. et al. Canagliflozin alleviates LPS-induced acute lung injury by modulating alveolar macrophage polarization. Int. Immunopharmacol. 88, 106969 (2020).
Xu, L. et al. SGLT2 inhibition by empagliflozin promotes fat utilization and browning and attenuates inflammation and insulin resistance by polarizing M2 macrophages in diet-induced obese mice. EBioMedicine 20, 137–149 (2017).
Wang, Y. & Xia, N. Influence of sodium-glucose cotransporter-2 inhibitors on plasma adiponectin in patients with type 2 diabetes: A meta-analysis of randomized controlled trials. Horm. Metab. Res 54, 833–844 (2022).
La Grotta, R. et al. Anti-inflammatory effect of SGLT-2 inhibitors via uric acid and insulin. Cell Mol. Life Sci. 79, 273 (2022).
Lee, Y. E. & Im, D. S. SGLT2 Inhibitors empagliflozin and canagliflozin ameliorate allergic asthma responses in mice. Int. J. Mol. Sci. 25, 7567 (2024).
Garvey, W. T. et al. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metabolism 85, 32–37 (2018).
Gohari, S. et al. The effect of EMPAgliflozin on markers of inflammation in patients with concomitant type 2 diabetes mellitus and Coronary ARtery Disease: the EMPA-CARD randomized controlled trial. Diabetol. Metab. Syndr. 14, 170 (2022).
Gunasekaran, K. et al. The impact of diabetes mellitus in patients with chronic obstructive pulmonary disease (COPD) hospitalization. J. Clin. Med. 10, 235 (2021).
Lipson, D. A. et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N. Engl. J. Med 378, 1671–1680 (2018).
Martinez, F. J. et al. Reduced all-cause mortality in the ETHOS trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. a randomized, double-blind, multicenter, parallel-group study. Am. J. Respir. Crit. Care Med. 203, 553–564 (2021).
Trinetx. Trinetx. https://trinetx.com/.
Diamant, M. & Morsink, L. M. SGLT2 inhibitors for diabetes: Turning symptoms into therapy. Lancet 382, 917–918 (2013).
Dong, H. et al. Risk factors for acute exacerbation of chronic obstructive pulmonary disease in industrial regions of China: A multicenter cross-sectional study. Int J. Chron. Obstruct Pulmon Dis. 15, 2249–2256 (2020).
Hogea, S. P. et al. Risk factors of chronic obstructive pulmonary disease exacerbations. Clin. Respir. J. 14, 183–197 (2020).
Hurst, J. R. et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir. Res 23, 213 (2022).
Müllerová, H., Shukla, A., Hawkins, A. & Quint, J. Risk factors for acute exacerbations of COPD in a primary care population: A retrospective observational cohort study. BMJ Open 4, e006171 (2014).
Lin, L., Shi, J., Kang, J. & Wang, Q. Analysis of prevalence and prognosis of type 2 diabetes mellitus in patients with acute exacerbation of COPD. BMC Pulm. Med. 21, 7 (2021).
Morgan, C. J. Landmark analysis: A primer. J. Nucl. Cardiol. 26, 391–393 (2019).
Acknowledgements
We thank Chung-Han Ho for interpreting our results.
Author information
Authors and Affiliations
Contributions
J.Y.W. and K.C.H. processed the experimental data, M.Y.L. and Y.J.W. performed the analysis, K.M.L. and C.C.L. drafted the manuscript, W.H.H. and Y.W.T. designed the figures. T.H.L. and P.Y.H. were involved in planning and supervised the work. M.H.C. and T.Y. aided in interpreting the results and worked on the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, JY., Hu, KC., Liu, MY. et al. The clinical effectiveness of sodium-glucose co-transporter-2 inhibitors on prognosis of patients with chronic obstructive pulmonary disease and diabetes. Nat Commun 16, 5478 (2025). https://doi.org/10.1038/s41467-025-60582-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60582-y