Abstract
The monkeypox virus (MPXV) outbreak of 2022 caused a human disease with unusual epidemiological and clinical features, notably an increase in human-to-human transmission through sexual contact, predominantly among men who have sex with men (MSM). This evolution underscores the need to reassess prevention and control strategies in the context of a sexually transmitted disease. Here, we show that rectal challenge of male cynomolgus macaques with a 2022 clade IIb MPXV isolate mimics sexual transmission, leading to rectal infection, with systemic and male genital tract dissemination and seminal fluid shedding. Vaccination with modified-vaccinia Ankara (MVA) protected the macaques from subsequent rectal MPXV challenge. However, MVA failed to prevent the disease when administered four days post-exposure to MPXV. These findings have a critical impact on outbreak management and highlight the importance of reevaluating MVA post-exposure prophylaxis protocols.
Similar content being viewed by others
Introduction
Monkeypox virus (MPXV), responsible for monkeypox disease (mpox), is an Orthopoxvirus of the large Poxviridae family, including the variola virus (VARV), which causes smallpox1. Until 2022, MPXV was considered to be an emerging zoonotic pathogen circulating mainly in limited areas of Africa (forested regions of West and Central Africa), with sporadic cases brought from the continent and limited human-to-human transmission. In May 2022, a case of the strain B.1 lineage clade IIb was reported in the United Kingdom, and in July of the same year, the World Health Organization (WHO) declared mpox a public health emergency of international concern2. Mpox related to clade IIb virus strain then spread rapidly throughout Europe and the Americas, affecting more than 124,753 people and causing more than 272 reported deaths, as reported in February 2025. This was the first global non-African mpox epidemic3.
The 2022 mpox outbreak had the unusual profile of being a sexually transmitted infection (STI), with more than 95% of patients during this outbreak being men who have sex with men (MSM) or bisexual men. It is now established that MPXV has the ability to human-to-human transmission through intimate contact and sexual intercourse4. Mild clinical manifestations were observed in most pandemic sexually-transmitted cases4,5, including a rash and less than 10 external lesions, predominantly in the anogenital and oral areas, while endemic mpox cases previously reported led to severe illness and hospitalizations of about 30% of the patients and provokes more than 100 lesions in 20–42% of the patients6,7. During the 2022 pandemic, common systemic features preceding the rash include fever, lethargy, myalgia, headache, and lymphadenopathy. Approximately 5–10% of patients were hospitalized, mostly for pain management8. The vast majority of patients recovered within a few weeks and only a few cases of reinfection in the following year were reported9,10. Since the end of 2023, a new Clade Ib MPXV outbreak occurred in Democratic Republic of Congo (DRC) with high fatality rates and enhanced spreading ability between humans, which makes clade Ib a major public health concern requiring urgent attention and containment measures11. Both Clade Ia and Clade Ib are still co-circulating in 2025 and sexual transmission seems to predominate in some DRC areas12. In the rest of the country, clade Ia was the most widespread strain, accounting for 95% of cases.
Whether MPXV clade IIb sexual transmission occurs through strict mucosal contact or via a combination of cutaneous and mucosal routes has yet to be clearly demonstrated13,14,15. There is strong evidence for sexual mucosal transmission of MPXV IIb during the 2022 mpox pandemic, including histories of unprotected sexual activity with multiple partners, eruptions in the anogenital area, and detection of the virus in semen and rectal swabs at levels consistent with transmission13. Moreover, mpox prevalence has been associated with HIV-1 infection and other sexually transmitted diseases16,17,18,19.
Faced with the 2022 new outbreak, the WHO proposed pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) using second-generation (ACAM2000) or third-generation vaccines such as modified-vaccinia Ankara (MVA) and LC16 vaccines20. Vaccination campaigns have been initiated worldwide and the MVA produced by Bavarian Nordic (MVA-BN) is still recommended by the US Centers for Disease Control and Prevention and in Europe21,22. Between September 2022 and February 2023, more than one million doses were administrated worldwide, including 336,976 vaccine doses used in 25 European countries, with most (86%) given as primary preventive (PrEP) vaccinations22. The MVA vaccine is an replication-deficient attenuated poxvirus obtained through more than 500 serial passages in chicken embryo fibroblast cells, offering a lower risk of serious adverse events than previous generations of vaccines23,24,25,26. In a European observational study, the efficacy of MVA in a PrEP design (MVA-PrEP) was estimated to be 68.2% (95% CI: 4.3–89.5%)27, confirming global data from the clade IIb outbreak demonstrating Jynneos vaccine effectiveness of the 2-dose series ranging from 66% to 89%28,29,30,31,32,33. A systematic search and meta-analysis supported the use of vaccinia-binding antibody titers as a correlate of the effectiveness of vaccinia-based vaccines34. The analysis showed that two doses of MVA-BN were more efficient than a single dose, with respective effectiveness of 81.8% and 73.6%, and predicted that delaying the second dose of MVA-BN vaccination would provide more durable protection and thus could be the optimal approach during an outbreak with a limited vaccine stock34. Additional cohort studies conducted in Spain and Italy confirmed MVA-BNʼs efficacy. A single dose offered protection against mpox in most-at-risk population shortly after the vaccination35 but a two-dose schedule is preferable, especially for people living with HIV (PLWH), to maximize the neutralizing antibodies response36. However, infections can occur in rare cases among fully vaccinated individuals, in particular, among individuals vaccinated by the subcutaneous route37. Indeed, some recent data suggest a short-lived neutralizing antibody response against MPXV in MVA-naive human volunteers38,39 and reported a critical decrease in neutralization capacity in MVA vaccinated individuals and at lower level in convalescent patients40,41. Finally, the effectiveness of administering MVA-BN as post-exposure prophylaxis remains poorly documented.
Animal models are particularly helpful in identifying correlates of protection and optimizing immunization strategies. MVA-BN administered by the subcutaneous (SC) or intradermal (ID) routes, ACAM2000, and the Ad35 vector-based vaccines Ad35-L1R/B5 and Ad35-L1R/B5/A27L/A33R have provided significant protection against high-dose intravenous (IV) challenge with lineage B.1, Clade IIb MPXV in macaques42. However, although IV infection represents a highly stringent challenge, it does not mimic the natural route of transmission observed during the 2022 outbreak. Mucosal exposure may involve distinct mechanisms of transmission and viral dissemination, and prevention may require adapted vaccination strategies that favor local immunity. Studies more accurately reproducing rectal mucosa transmission43 or combined skin and rectal transmission44, as observed in the recent human epidemics, are required. To date, no animal study has investigated the efficacy of MVA against rectal mucosal challenge in a MVA-PrEP or MVA-PEP design similar to the administration scheme recommended for humans.
Here, we evaluated the immunogenicity and protective efficacy of the MVA vaccine against MPXV in cynomolgus macaques. We confirmed that the MVA-PrEP approach provides protection against a subsequent Clade IIb MPXV rectal challenge. However, we demonstrated that a single dose of MVA administered four days post-exposure failed to protect macaques from MPXV transmission, raising concerns about the emergency protocol implemented by health authorities in 2022.
Results
MPXV transmission route modulates the disease severity and the humoral response of macaques
We challenged four male cynomolgus macaques via the non-lesional rectal route with a clade IIb strain isolated from a French patient during the 2022 outbreak (MPXV/France/IRBA-CNR-22-11/2022)45 at an infective dose of 1 × 107 plaque forming units (pfu) (Fig. S1). Two animals were retained for long-term follow-up until 83 days post-challenge, and two were euthanized for necropsy on day 11, corresponding to the peak of clinical symptoms. Clinically, animals displayed localized proctitis, rectal exudate, weight loss, and moderate skin lesions, mostly in the genital area (Fig. 1a). Skin lesions were also observed, strikingly akin to those observed in patients, in scattered areas, such as the paws, perianal zone, and other mucosal areas such as the mouth. Microscopically, skin sections showed pustular epidermal necrosis associated with numerous neutrophils and cellular debris (Fig. S2). The lesions concurrently manifested in all four animals, approximately one week post-challenge, and spontaneously resolved within 2 weeks. The infection also led to anemia, as well as transient lymphopenia, with a nadir on day 6 followed by lymphocytosis peaking on day 11 post-challenge and lymphadenomegaly (Fig. S3). Viral DNA was detected in the blood from day 6 to day 11 post-challenge (Fig. S4a). Prolonged shedding, assessed by qPCR and the detection of infectious virus by replication assay in Vero cells, were observed in rectal fluids and seminal plasma up to three weeks post-challenge (Fig. 1b, c). Beyond three weeks, infectious virus was no longer detectable in the rectal or seminal fluids, although the presence of DNA persisted. We also observed viral DNA and infectious virus at distant mucosal sites, such as the nasopharyngeal fluids and saliva (Figs. S4b, S1c and Table S1).
Four cynomolgus macaques were challenged with MPXV IIb virus on day 0 with 1 × 107 pfu of MPXV by the rectal route. Two animals were euthanized on day 11 and two were followed for 83 days for clinical and immunological monitoring (a). Five clinical signs were monitored for 34 days (n = 2): the presence of rectal exudate, loss of appetite, presence of lesions, lymphadenomegaly, and weight loss >10% were recorded for each animal. b Viral load assessment in rectal and seminal fluids (n = 4 for rectal fluid and n = 2 for seminal plasma). MPXV DNA was quantified by qPCR and is expressed as viral DNA copies/mL. The lower limit of detection (LLOD) was 90,000 copies/mL, and the lower limit of quantification (LLOQ) was 100,000 copies/mL. c The rectal and seminal fluid samples containing viral DNA were tested for virus infectivity in Vero cells. Viral infectivity is quantified in pfu/mL. The LLOD was established at 10 PFU/mL, indicated by the dotted line. All samples below this LLOD were considered negative and are represented by a value of 1. d Orthopoxvirus-binding IgG concentrations are reported in arbitrary units (arb. unit./mL). Serum (left) and seminal plasma (right) from two NHPs (n = 2) were evaluated for the total anti-MPXV protein IgG concentration before challenge and at various time points up to days 62 and 83 post-challenge for serum and seminal plasma, respectively. Each symbol represents one animal, and the different shapes represent different antigens. The dashes represent the mean. Ag: antigen. Source data are provided as a Source Data file.
We detected viral DNA in the digestive tract, including the rectum, colon, and duodenum, in the two animals euthanized on day 11 post-challenge, estimated to correspond to the peak of viral replication (Table 1). Infectious virus particles were also detected in the digestive tract of both animals. Various lymph nodes draining the digestive tract were positive, suggesting dissemination of MPXV from the digestive tract through the lymphatic system. The spleen was also positive in one animal (Table 1). The recto-colonic lesions were characterized by marked inflammatory infiltration, with numerous neutrophils (calprotectin+) and T lymphocytes (CD3+), and limited infiltration by B cells (CD20+) and macrophages (CD68+) (Fig. 2a, e–h), as well as those of the skin (Fig. S2, panels c–f). Pustular and ulcerative lesions were observed in the colon (Fig. 2a), along with the accumulation of fibrin and necrotic material (Fig. 2, panel c). In addition, animals exhibited hyperplastic epidermis and necrotic changes in the epidermal lesions (Fig. S2), with lymphocyte-rich interface dermatitis (Fig. S2, panel a). Hyperplastic epithelial cells contained 1-3 µm wide, highly acidophilic to amphophilic intracytoplasmic inclusion bodies (marked by arrows in Fig. S2, panel b). Staining for Orthopoxvirus by immunohistochemistry (using anti-vaccinia antibodies) or in situ hybridization (RNAscope) of viral RNA showed the virus to be present inside lesions of the rectum and skin (Fig. 2i, d, g and Fig. S2, panels h, I, and j). We finally compared the dynamics of infection following strict rectal mucosa transmission with the dynamics observed after ID administration or after a combined rectal and ID routes administration. We also tested a lower dose of 1 x 106 pfu by strict rectal route. We observed more severe disease when animals were exposed by the ID route, associated or not with the rectal route, characterized by a higher number of skin lesions, a more marked episode of fever, and prolonged shedding of viral DNA and infectious virus (Figs. S4–S6).
Representative Hematoxylin-Eosin staining of the rectal mucosa on day 11 post-challenge from a cynomolgus macaque infected with MPXV. The analysis was performed on 2 animals. a Ulcerated rectal mucosa at the margin of the anus showing ulcerative, necrotizing rectitis (*) characterized by b hyperplastic mucosa (arrowhead) and c fibrin and extravasated erythrocytes (hemorrhage) (arrow head). d rectal submucosa, with numerous inflammatory cells (arrow head), mostly e neutrophils (calprotectin staining), f T cells (CD3 staining), g follicular-like B-cell aggregates (CD20 staining), and h minimal diffuse macrophage infiltration (CD68 staining). i RNA scope using a specific MPXV probe in the submucosal ulcerated tissue and adjacent epithelium (purple staining localized mostly in the ulcerated area). j RNAscope with the negative control probe DapB. Scale-bars: a = 500 µm, b–j = 100 µm.
Both the ID route alone or associated with the rectal route MPXV challenge induced rapid seroconversion, with specific MPXV IgG antibodies detected from day 13 and reaching a plateau by day 20 post-challenge at the latest (Figs. 1d, S7). Here, we evaluated exclusively the response against five late proteins produced at the end of the virus cycle which are mainly structural proteins forming the mature viral particles. All challenged animals developed high concentrations of serum IgG targeting two of the extracellular enveloped virion (EEV) proteins tested here (A35 and B6) and two intracellular mature virion (IMV) proteins (A29 and E8), as assessed by electrochemiluminescence assays (ECLAs; Figs. 1d, S7). The infectious challenge did not appear to trigger a significant antibody response against the M1 IMV protein, as previously reported46. The response against vaccinia (VACV) proteins sharing structural, functional and sequence homology with MPXV proteins showed similar antibody response patterns, confirming broad cross-reactivity against poxvirus family members (Figs. S7, S8). Indeed, the comparison of the structural models of the neutralization determinants M1/L1, A35/A33, A29/A27, E8/D8, between a MPXV strain and a VACV strain showed that the MPXV models exhibited approximately 90% identity to the VACV template with a perfect match of 99% for M1/L147. In more detail, the animals, except those challenged by the rectal route at 1 x 106 pfu, showed similar levels and kinetics of anti-Orthopoxvirus IgG in the serum, whereas the 1 x 106 pfu rectal challenge group showed a delayed and weaker IgG-specific response in the serum than the 1 × 107 pfu rectal challenge group (Figs. 1d, S7, and S8). Whether after ID or rectal administration, anti-MPXV and anti-VACV IgG were also detected in seminal plasma, although at lower levels than in serum (p = 0.0078 at day 13 or day 15 post-challenge). As in the serum, rectal exposure at 1×107 pfu resulted in comparable levels of seminal plasma MPXVspecific IgG (significance not tested because of the low number of animals) as the ID and “ID + rectal” route challenge at 1 x 106 pfu (Figs. 1d, S7 and S9). Serum-neutralizing antibodies against live MPXV virus, assessed by plaque reduction neutralization titers (PRNTs), showed that rectal challenge triggered either no response (n = 1) or low and delayed response (83 days post-challenge) relative to the ID route (n = 2) which triggers a rapid neutralizing response (Fig. S10). These results suggest differences in the pathophysiological mechanisms of the induction and maturation of the immune response depending on the transmission route. Differences in levels and kinetics between specific binding IgG and neutralization titers also suggest that not all IgG have neutralizing capacities and that other antibody functionalities deserve to be explored.
MVA-N33 vaccine efficiently prevents infection of non-human primates
We assessed the efficacy of MVA-N33 in a pre-exposure prophylaxis (MVA-PrEP) setting against sexual MPXV transmission. Four cynomolgus macaques were vaccinated with two SC doses of 1 × 108 pfu of MVA 4 weeks apart (Fig. 3a). The quality of the humoral and cellular immune responses, as well as the efficacy against MPXV challenge, was compared to that of a group of six convalescent (Conv.) animals composed of the above-mentioned NHPs infected by the rectal or ID routes 37–46 weeks before the second challenge. These MVA-N33 vaccinated animals and mpox convalescent animals were challenged, along with four non-vaccinated MPXV -naïve NHPs as controls (CTRLs), with 1 × 107 pfu of clade IIb MPXV administered via the strict rectal route as we reported above. Four additional naïve animals were vaccinated four days after challenge with 1 × 108 pfu of MVA-N33 by the SC route to assess the efficacy in a post-exposure prophylaxis (MVA-PEP) experimental setting, thus reproducing the recommendations for the management of exposed populations during the 2022 epidemic.
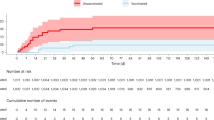
a Study design on NHP immunization and challenge periods in weeks, and a description of the four groups of cynomolgus macaques. One group was vaccinated before the challenge with two doses of MVA administered 4 weeks apart (MVA-PrEP, n = 4; gray). Another group was vaccinated with a single dose four days after the MPXV IIb challenge (MVA-PEP, n = 4; black). In addition, we challenged one group of convalescent NHPs previously exposed via the rectal or ID route alone or in combination 37–46 weeks before the challenge and described previously (Conv., n = 6; orange) and one control group (CTRL, n = 4; red). The four groups were challenged with 1 × 107 pfu of MPXV by the rectal route as indicated in blue. MVA-PrEP animals were monitored during the MVA immunization phase, with blood samplings for immunogenicity analysis. Following the MPXV challenge, blood, rectal fluid, seminal plasma, and skin swab samples were collected. The blue vertical dotted line represents the challenge. The image was created in BioRender. Herate, C. (2025) https://BioRender.com/lkzvios. b Rectal fluids collected during the challenge phase were evaluated for viral DNA content by qPCR. Viral load is expressed as viral DNA copies/mL. Each graph represents the viral kinetics of one group during 27 days. The LLOD was 36,000 copies/mL and the LLOQ 100,000 copies/mL. c Rectal fluid containing viral DNA was tested for virus infectivity in Vero cells and measured in pfu/mL. The LLOD was established at 10 PFU/mL, indicated by the dotted line. All samples below the LLOD were considered negative and are represented by a value of 1. When qPCR was negative, samples were considered negative and are represented by a value of 1. d Area under the curve (AUC) of viral DNA in rectal fluids during the 27 days of follow-up and statistical analysis. (CTRL, n = 4; red), (MVA-PEP, n = 4; black) (MVA-PrEP, n = 4; gray) (Conv., n = 6; orange). **:p = 0.0079. Each circle represents one animal. e Viral load measured by qPCR in skin swabs (left) and seminal plasma (right) sampled at day 11 and statistical analysis. The mean value is represented by the horizontal bar. (CTRL, n = 4 for skin and seminal fluid; red), (MVA-PEP, n = 3 for skin and n = 4 for seminal fluid; black) (MVA-PrEP, n = 3 for skin and n = 4 for seminal fluid; gray) (Conv., n = 5 for skin and n = 6 for seminal fluid; orange). *:p = 0.0333. Each circle represents one animal. Statistical analyses were performed using the Kruskal-Wallis test followed by a two-tailed non-parametric Mann-Whitney test (*p < 0.05, **p < 0.01). Source data are provided as a Source Data file.
MPXV challenge resulted in similar rectal fluid viral loads in the CTRL and MVA-PEP animals, as measured by quantitative PCR (qPCR) and infectious viral titers (Fig. 3b–d). By contrast, Conv. animals showed complete protection as viral load remained below the limit of detection at all time points measured after challenge (Fig. 3b–d). The MVA-N33 vaccine significantly prevents infection in the PrEP setting (Fig. 3d) with only two animals having detectable virus and at only a single time point (day 4 or day 11 post-challenge) (Fig. 3c). In the PrEP group, a significant reduction (p = 0.03) of area under the curve (AUC) for the rectal DNA viral load was observed between days 0 and 28 post challenge when compared to control animals (mean AUCs of 1.39 x 109 and 4.12 x 1012 copies·days/mL, for PrEP and CTRL groups respectively). In addition, complete control of viral dissemination in the seminal plasma was confirmed for all MVA-PrEP animals (Fig. 3e). Skin swabs carried out at the site of the lesions, when they existed, and saliva (Fig. 3e and Table S2) also confirmed the control of infection in MVA-PrEP animals. Viral control in MVA-PrEP and Conv. animals was associated with protection from the disease, as demonstrated by the clinical scoring, the lack of fever, the low number of lesions or no detectable lesions, and the absence of lymphopenia (Fig. S11).
MVA-N33 Vaccine induced specific cross-neutralizing antibody response against Orthopoxvirus family
In the search of immune parameters associated with protection, we assessed anti-vaccinia virus (anti-VACV) and anti-MPXV humoral and cellular response following MVA-N33 vaccination and clade IIb MPXV challenge. As demonstrated, two injections of MVA-N33 were required to reach significant levels of anti-VACV IgG in the serum48. Late proteins, because they primarily encode surface proteins of mature virions and enveloped virions, are ideal vaccine targets; they are exposed, immunogenic, involved in viral dissemination, and shared across multiple orthopoxviruses49. We tested the IgG response against five late proteins, including L1 and A27 proteins present on the IMV membrane. All animals seroconverted against the A33, B5 and D8 vaccinia proteins following the first injection, and the MVA-N33 boost induced a significant increase in specific IgG titers (Tables S3 and S4), which then slowly decreased (Fig. 4a). Similar level and dynamics of IgG responses was observed in two animals administered with the commercial MVA-BN vaccine (Fig. S12), showing equivalence between the two vaccines. The responses induced by MVA-N33 remained detectable for all vaccinated animals at the time of challenge corresponding to W12 post first-immunization, with mean titers ranging from 9152 ± 12,719 (mean ± SD) to 13,450 ± 20,831 and 33,072 ± 30,706 for the A33, B5, and D8 proteins, respectively. Only low to moderate IgG responses were induced against the L1 and A27 IMV proteins, and we observed a particularly low IgG titer specific to A27, for which there were only three responders among the four vaccinated macaques. This was expected because the L1 protein is a late expressed protein and retained in the IMV membrane50. Previous reports also showed that A27 encoded by MVA does not elicit a strong antibody response42,51,52. Specific anti-VACV IgG induced by MVA-N33 also cross-reacted with the A35, B6, E8, and M1 of MPXV clade IIb proteins, all remaining at significant levels (Fig. 4a and Tables S3 and S4) until the challenge. We then questioned the possibility of MVA-N33 to induce cross clade anti-MPXV binding antibodies, and in particular against clade Ia virus currently circulating in DRC. Five particularly immunogenic antigens of MPXV clade IIb show a high level of homology with clade Ia with 100% identity between the B6 and M1 proteins sequences. Sequence analysis also reveals that A29 and A35 proteins vary only by 2 amino acids and that currently circulating clade Ia and Ib possess only the mutation A19T in E8 protein (Fig. S13). The high degree of homology between Clade Ia and Ib suggests that it is thus unlikely that the in vitro assay used for IgG quantification can differentiate between anti-Clade Ia and Ib binding antibodies. This high degree of homology between Orthopoxviruses immunogenic regions was recently confirmed by analysis of T cell epitopes in humans53. At the time of challenge, the average of anti-VACV and anti-MPXV responses were in the same range as those detected for Conv. animals, except for MPXV A35, for which the Conv. animals that were previously exposed to homologous MPXV during the first challenge study and thus showed higher IgG levels than the MVA-PrEP animals (p = 0.0095). However, similar levels of IgG against A33 vaccinia virus antigen were detected in the two groups (Tables S3 and S4).
a The concentrations of five MPXV (upper panel) and homologous VACV (lower panel) protein-binding IgG were quantified in the serum of NHPs that were either immunized with MVA and/or challenged with MPXV. The data are expressed in arbitrary units (arb. unit./mL). Total IgG concentrations in NHP serum were monitored during the immunization phase for the MVA-PrEP group and after the challenge phase. For the remaining three groups, IgG follow-up began two weeks prior to the challenge. b Seroneutralization titers were measured in the serum collected at week -1 and week 4 post-challenge using Vero cells and live MPXV or VACV. The mean PRNT50 with standard deviation were calculated using infectious MPXV IIb (left panel): *:p = 0.0159, MPXV Ia (middle panel): *:p = 0.0159 or VACV-107 (right panel): *:p = 0.0190 and **:p = 0.0095. (CTRL, n = 4; red), (MVA-PEP, n = 4; black), (MVA-PrEP, n = 4; gray), (Conv., n = 6 at W-1 and n = 5 at W4; orange). c, d Cellular immunity conferred by MVA vaccination and/or MPXV challenge. (CTRL, n = 4; red), (MVA-PEP, n = 4; black) (MVA-PrEP, n = 4; gray) (Conv., n = 6 and n = 5 from W14; orange). Intracellular staining of PBMCs, collected during the MVA immunization phase and after MPXV challenge, after an overnight MPXV or MVA stimulation in vitro. Panels represent the mean percentage with standard deviation of CD4+ CD154+ cells expressing IFN-γ (c) and IL17A (d) upon MPXV 2b (left) or MVA (right) stimulation. For (b–d), each circle represents one animal. When represented, statistical analyses were performed using the Kruskal-Wallis test followed by a two-tailed non-parametric Mann-Whitney test (*p < 0.05, **p < 0.01). Ag: antigen; Stim. Stimulation. Source data are provided as a Source Data file.
In order to explore mucosal immunity, we assessed specific IgA response in serum (Fig. S14a and S14b). MVA-N33 vaccination induced specific IgA against A35/A33, E8/D8, while B6/B5 response remained limited and responses did not last as compared to specific IgG. Almost no response was observed against A29/A27 and M1/L1. No anti-VACV or anti-MPXV specific IgA was detectable in the rectal mucosa of MVA-PrEP vaccinated animals following vaccination, while we observed an IgA-specific response in this compartment after MPXV challenge (Fig. S14c).
MVA vaccination also induced anti-VACV neutralizing antibodies in MVA-PrEP group, as measured using specific fluorescent MVA based assay (Fig. S15). Although the neutralizing titers significantly increased (p = 0.0286) following the boost, they then rapidly decreased.
One week before challenge, we compared neutralizing activities between all groups using the PRNT assay that allowed testing neutralizing activities against two clades of replicative MPXV, the clade Ia and IIb (Fig. 4b). As expected, no response was detected in the control or MVA-PEP animals. We detected a limited and no significant response in the MVA-PrEP animals against the two tested clades Ia and IIb of MPXV (p = 0.4286) and VACV (p = 0.4286) when compared to controls. Two MVA-PrEP animals had decreased neutralizing response at time of challenge, below the detection limit. In the two MVA-PrEP animals similar neutralization capacity (Table S5) was observed against MPXV IIb and MPXV Ia, suggesting that the MVA-N33 vaccine may have cross-clade efficacy. As expected, the titers in Conv. animals remained at levels significantly higher (p = 0.0095 and p = 0.0159 for VACV and both MPXV clades, respectively, Fig. 4b). Correlation between seroneutralization titers and anti-EEV protein-binding IgG (Table S6), in particular for A33 and B5 VACV antigens and A35 and B6 MPXV antigens, suggest a particular involvement of these antibodies in the control of viral replication.
MPXV rectal challenge recalls specific antibodies in preimmunized macaques
Rectal challenge with MPXV elicited a recall response against MPXV and VACV antigens in all MVA-PrEP animals, confirming cross-reactivity of the vaccine-induced antibodies with the challenge virus (Fig. 4a). The two vaccinated animals with a low-level anamnestic response were also those that showed the highest binding following vaccination and no detectable virus following challenge, confirming that anti-OPXV responses are known to contribute to protection. (Fig. 3b). In addition, the two animals showing an amnestic response and transient viremia also had the highest antibody concentration and neutralizing activity against the two clades of MPXV after the challenge, revealing a complete cross-reactivity between the clades Ia and IIb. The Conv. macaques did not show a significant increase in the anti-VACV or anti-MPXV binding response, thus confirming the observed complete protection from re-infection (Fig. 4b).
The challenge also resulted in an increase in the anti-MPXV Ia and IIb neutralizing response in CTRL, MVA-PEP and MVA-PrEP infected macaques (2 out of 4), with comparable levels, making it difficult to discriminate between a potential anamnestic response in the MVA-vaccinated animals and the generation of new neutralizing specificities.
Finally, the MVA-PEP animals developed a binding and neutralizing response against MPXV IIb with levels and kinetics similar to those of the CTRL macaques, confirming the absence of protection. We observed a weak neutralizing response against VACV in this group, suggesting that in the absence of pre-existing MVA immunization, the anti-MPXV response observed 4 weeks post-challenge did not fully cross-neutralize VACV, and that a single MVA-N33 vaccine injection was insufficient to improve this response (Fig. 4a, b).
MVA-N33 vaccine elicits CD4+ and CD8+ specific cellular immune response
We assessed the Orthopoxvirus-specific cellular immune response by measuring the production of five intra-cellular cytokines by CD4+ CD154+ and CD8+ CD137+ activated T cells upon overnight stimulation of fresh isolated PBMCs with 0.3 pfu of infectious MPXV IIb or MVA-N33 (Figs. 4c, d, and S16). Two injections of MVA-N33 vaccine (MVA-PrEP group) induced CD4+ T-cell activation (measured by increased CD154 expression) and a specific response characterized by IFN-γ (p = 0.029) and TNF-α production (p = 0.029). We also observed detectable IL-13 and IL-17A responses in CD4+ T cells after MVA-N33 vaccination (Fig. 4d and S16d). At the time of challenge, similar levels of activation of the CD4+ T cells were observed in Conv. and MVA-PrEP animals upon MPXV and MVA-N33 stimulation (Fig. 4c, d, and S16). Conv. animals tended to have a higher proportion of polyfunctional cells, mainly expressing IFN-γ and TNF-α than MVA-PrEP animals (Figs. 5 and S17).
CD4+ and CD8+ cells producing TNF-α, IL-2, and IFN-γ are represented for each animal (one pie chart per animal) at W12 post-immunization (W−1 post-challenge) and W15 post-immunization (W2 post-challenge). The polyfunctionality of CD4+ CD154+ (left) and CD8+ CD137+ (right) cells upon MPXV IIb stimulation is shown. Non-responder cells are not represented. Cells secreting only one of the three cytokines are in blue, two of them in green, and three in orange. Source data are provided as a Source Data file.
Following challenge, three of four MVA-PrEP animals and all six Conv. NHPs did not develop an increase in the specific CD4+ response, consistent with low or absence circulation of the virus resulting from the almost complete control of MPXV replication to undetectable levels (Figs. 4c, d and S16a, c, and d). The MVA-PrEP animal showing an increase in the number of CD4+ T cells producing IFN-γ, TNF-α, and IL-2 after the challenge corresponded to one of the two vaccinated animals with low detectable virus in rectal fluids. The challenge triggered a significant (p = 0.029) increase in the number of specific CD4+ T cells in CTRL and MVA-PEP animals, peaking at week 2 post-challenge (Figs. S16a and S16b). In addition to IFN-γ, TNF-α, and IL-2 production, IL-17- and IL-13-producing cells were also elicited, both in the CTRL and MVA-PEP groups at week 2 and week 6 post-challenge, respectively (Figs. 4d and S16). The frequency of anti-MPXV CD4+ T cells appeared to be significantly (p = 0.0078 for IFN-γ and TNF-α secreting cells) higher than that of anti-VACV CD4+ T cells in naïve animals, likely confirming the specificity of the anti-MPXV CD4+ T cell response.
Following the vaccine boost, we also observed a CD8+-specific response driven by IFN-γ and TNF-α in 3 of 4 animals of the MVA-PrEP group (Fig. S16c, e), which appeared to cross-react between VACV and MPXV antigens. After challenge, the CD8+ cell response also tended to be driven by these two cytokines and most responder CD8+ cells secreted IFN-γ and remained cross-reactive (Figs. 4e and S17). All groups except convalescent animals showed an increased IFN-γ and TNF-α response (Fig. S14c, e), suggesting that eliciting specific CD8+ T cells may require lower exposure to viral antigens than that required to elicit specific CD4+ cells and antibodies. It is noteworthy that the lack of increase in the cellular and humoral immune responses in Conv. animals following the MPXV challenge suggests early and highly effective control of the virus.
Anti-MPXV antibody response correlates with mpox protection
We aimed to identify immune parameters associated with protection in a correlation analysis using all the data obtained in this preclinical study, including the cellular response and the humoral response, often considered as critical for mpox protection54. Here, the viral load of MPXV in rectal swabs negatively correlated with MPXV EEV and IMV antibody levels at the time of challenge (R = −0.817, R = −0.825, and p < 0.0001, respectively, for the MPXV A35 and E8 antibodies) and neutralizing capacity of antibodies against MPXV IIb and VACV (R = −0.768, R = −0.756, and p ≤ 0.001, respectively) (Fig. 6). These analyses, together with IgG binding titer data (Fig. 4a and Tables S3 and S4) suggested that a higher anti-A35 binding titer in convalescent animals could contribute to the protection observed. Recently, a study evaluating multiple antibody functions revealed that only three antibody features were determinant for predicting viral load in NHPs, including VACV A33-IgG2 titers, VACV-neutralizing antibody titers, and A33-FcgR3a binding levels55.
The frequency of CD4+ and CD8+ T cells secreting IFN-γ at the time of challenge negatively correlated with the peak viral load in the rectal fluid (R = −0.799, R = −0.751, and p ≤ 0.001, respectively). Overall, these data suggest that pre-exposure prophylactic vaccination induced protection involving both cellular and humoral immunity. Conversely, the MVA-PEP failed, in our experimental setting, to elicit an immune response capable of at least partially controlling viral infection and disease.
Discussion
In this study, we demonstrate that MPXV clade IIb can be transmitted in macaques via the atraumatic rectal route only, and that this is sufficient to recapitulate the clinical infection and moderate disease observed in humans during the 2022 outbreak4,56,57. Although not excluding other transmission modalities, or a combination of modalities, during this epidemic, these results confirm the STI nature of the disease, involving mechanisms allowing the virus to cross the mucosal barriers. We also showed here the relevance of NHP models in the characterizing these mechanisms and the consequences on pathogenesis. In particular, the study shows that the seminal fluids have a viral burden compatible with a role in transmission and that the rectal mucosa is susceptible to infection and allows local replication of the virus, probably contributing to both virus shedding into the environment and systemic dissemination. What could be the origin of the virus in semen, and what are the molecular and cellular factors allowing mucosal transmission requires further investigation to which NHP models can usefully contribute. In addition, whether mucosal transmission results from a specific adaptation of MPXV clade IIb58 or can be more generally extended to other viral clades may be of important interest for further development of prevention and therapeutic strategies, particularly regarding the ongoing upsurge of clade Ib MPXV in the Democratic Republic of the Congo (DRC) and in a growing number of countries in Africa, constituting, according to WHO, a public health emergency of international concern59.
We also provide novel data on the host response to MPXV infection and MVA vaccine. We clearly confirm the strong antibody and T-cell cross reactivity between vaccinia and MPXV antigens, including neutralizing antibodies against both clades of MPXV and suggest the broad spectrum of protection against a diversity of orthopoxvirus infections that can be expected with MVA based vaccine used in a pre-exposure prophylactic setting.
We were not able to identify specific neutralizing targets in MPXV antigens associated with protection. Antigens other than VACV A33 may be involved since there is reported low cross-reactivity with the MPXV A35 due to the heterogeneity of the A33 protein family60. Immune mechanisms correlating with protection observed in our studies appeared to include a diversity of B as well as CD4+ and CD8 + T-cell-specific responses. Whether the combination of these immune effectors is required for protection or only a few mechanisms are involved may need further elucidation in order to foster the development of immunotherapies or a new generation of vaccines. The association between IgG binding titers to A33/A35 and B5/B6 antigens and neutralization suggests their contribution to protection.
Other antibody functionalities in protection like Fc-related functions may also play a role. In addition, the observation of a Th17 response also argues for a role of mucosal T cells in the response to infection. Whether this is specific to mucosal transmission or not, and may be of importance to vaccine-induced protection remains to be addressed. Consistent with our findings, previous reports indicated that rectal infection in NHPs is less immunogenic for cell-mediated immunity than the IV or ID routes43. This weaker response after infection could explain the few observed reinfection in humans during the recent epidemics9,10,61,62.
We present novel data comparing the efficacy of MVA vaccination in a classical pre-exposure prophylaxis protocol versus post-exposure vaccination administered shortly (between 4 days and 14 days in absence of symptoms after close contact with someone having mpox), as recommended by the WHO and most international and national health authorities63 despite limited data on the actual efficacy of the post-exposure prophylaxis protoco l20,22,64.
Our findings validate two doses of MVA-PrEP as an efficient vaccine protocol against mpox in the context of the current epidemics, including in cases of mucosal transmission. However, both protection and immunological response data indicate that MVA-PEP is not effective, as it failed to prevent MPXV replication in the rectal or seminal fluids. In our experimental setting, all PEP animals were naïve to any exposure to VACV or MPXV antigens. This may be the case for an increasing proportion of exposed individuals during the 2022 pandemic who were born after interruption of smallpox mass vaccination campaigns in 1981. The current post-exposure protocol was established during the smallpox eradication era using first-generation vaccines, which were administered as a single dose and were recently shown to be more immunogenic than MVA in an NHP model42. At that time, the human population possessed global immunity from childhood immunization campaigns. In that context, the post-exposure vaccine protocol likely proved to be more efficient by reactivating immune memory, serving as a booster to the preexisting immunity conferred by the first-generation vaccine. Our data suggest the urgent need for reconsideration of PEP protocols since vaccination 4 days after mpox exposure did not prevent infection and disease in our NHP model.
Methods
Ethics and biosafety statement
Twenty-four mature male Cynomolgus macaques (Macaca fascicularis) aged 3.5–7 years with a body weight of 4–14.6 kg and originating from Mauritian AAALAC (Association for Assessment and Accreditation of Laboratory Animal Care International)-certified breeding centers were used in this study. All animals were housed in the IDMIT infrastructure facilities (CEA, Fontenay-aux-Roses) under Biosafety Level 3 containment (animal facility authorization E92-032-02, Prefecture des Hauts de Seine, France) and in compliance with European Directive 2010/63/EU, French regulations, and the Standards for Human Care and Use of Laboratory Animals of the Office for Laboratory Animal Welfare (OLAW, assurance number F22-00556, United States). The protocols were approved by the institutional ethics committee “Comité d’Ethique en Expérimentation Animale du Commissariat à l’Energie Atomique et aux Energies Alternatives” (CEtEA n° 44) under statement number A22_037. The study was authorized by the ‘Research, Innovation and Education Ministry under registration number (APAFIS#38039–2022072015031466 v2).
Virus production
Monkeypox virus (MPXV) IIb strain MPXV/France/IRBA2211i/2022 (Genbank access number ON755039) used for infections and the neutralization assays was produced in Vero cells (African green monkey kidney, ATCC CCL-81) grown in Dulbecco’s modified Eagle medium (DMEM) and 10% fetal calf serum (FCS) at 37 °C in a 5% CO2 atmosphere. Supernatants and lysed cells from MPXV-infected Vero cells were frozen/thawed three times. The virus was pelleted by two rounds of ultracentrifugation (30,000 x g, 2 h) through a 40% sucrose cushion. MPXV was titrated on Vero cell monolayers using plaque-forming assays in 24-well plates. The MPXV strain MSF#10 2001 Zaïre65 used for neutralization assays on clade Ia was kindly provided by Dr Hermann Meyer from the Institute of Microbiology of the Bundeswehr. The strain was produced and titrated in the same way. Vaccinia virus (VACV) strain Lister clone 107 (VACV-107, GenBank access number DQ121394), used for the neutralization assays, was produced and titrated in the same way.
The MVA vaccine used for the efficacy study in NHP is MVATGN33.1 or MVA-N33, a MVA subclone, isolated in Transgene’s laboratories, from the MVA strain provided by Professor A. Mayr in February 1995 (Virus “MVA” II/85, passage 575 on chicken embryo fibroblasts (CEF) (GenBank access number EF675191.1), and was used for immunization. Crude harvests containing infected cells and culture supernatants were recovered and stored at −20 °C until use. Before purification, viral particles were released from the thawed suspension by homogenization using a homogenizing mixer equipped with an in-line chamber. Large cellular debris was then eliminated by depth filtration using filters with 5 µm pores. The clarified viral suspension was subsequently concentrated and subjected to diafiltration in formulation buffer (50 g/L saccharose, 50 mM NaCl, 10 mM Tris, 10 mM glutamate-Na, pH 8.0) using tangential flow and fiber microfiltration filters with 0.2 µm pores. Finally, the purified virus was further concentrated using the same tangential flow filtration system, aliquoted, and stored at −80 °C until use. Titration of MVA was performed on DF-1 cells (ATCC: CRL-3586) monolayers using plaque-forming assays in six-well plates. MVA-GFP, used for the neutralization assays, was produced and titrated in the same way.
DNA and protein sequences analysis
Sequences were extracted from GenBank66. Clades were confirmed using Nextclade67. Nucleic and amino acid sequences of five proteins of interest were extracted from GB files for sequence ON755039.1 and MSF#10. They were generated using Prokka68 using standard parameters and gb file from NC_063383.1 as reference. Both DNA and protein sequences were aligned using MAFFT69 version 7.520 then visualized using Jalview70 version 2.11.3.2 with colors indicating identity percentage. The phylogenetic tree was created using the whole DNA sequences of each sample and reference sequence of VACV Copenhagen as outgroup (OP868847.1). IQ-TREE271 was used to generate the tree with ModelFinder72 and standard parameters. Visualization was produced using a homemade Python script using ETE373 module, available in the following GitHub repository: https://github.com/Mossy-Frog/Phylogeny_visualization.git.
NHP challenge
Non-human primates (NHPs) were split into groups of n = 2 or n = 4 and exposed to MPXV IIb at 1 x 107 plaque-forming unit (pfu)/NHP by the rectal route (n = 4), 1 × 106 pfu/NHP by the intradermal (ID) and rectal routes (ratio 1:1) (n = 2), 1 x 106 pfu/NHP by the ID route (n = 2), or 1 x 106 pfu/NHP by the rectal route (n = 2). Briefly, animals were anesthetized with ketamine (5 mg/kg) associated with medetomidine (0.05 mg/kg) for viral challenge. For the ID challenge, the virus was diluted in 1 mL and administered by 10 injections in the back. For the rectal challenge, animals were placed on their ventral side to raise the rectum. The virus preparation was diluted in 3 mL saline buffer and slowly applied to the rectum using a nasogastric tube. The lower part of the animals was kept elevated for several minutes until no reflux was observed. For the MVA efficacy study, eighteen NHPs were similarly challenged by the IR route at 1 × 107 pfu/NHP.
MVA immunization
For the efficacy study, MVATGN33.1 (Transgene) was administered at a dose of 1 x 108 pfu in 0.5 mL by the subcutaneous route. The MVA pre-exposure prophylaxis group (MVA-PrEP) (n = 4) received two doses 28 days apart, with the first dose received three months before the viral challenge. The post-exposure prophylaxis (MVA-PEP) group (n = 4) received one dose of MVA vaccine four days after the challenge.
MVA-BN vaccine has been administered at the human clinical dose of 0.5 mL containing a minimum of 5 x 107 IU (Infectious Unit). The two animals used for immunogenicity study received two doses 28 days apart.
Clinical follow-up
Animals were observed every day, and clinical exams were performed at baseline and each blood draw, first when awake and then following anesthetization using ketamine (5 mg/kg) and medetomidine (0.05 mg/kg). Behavior was observed and qualified with and without human positive (alimentary reward distribution) or negative reinforcement (squeeze-back mobilization). Before handling, the animals were monitored and scored extensively, and food and water consumption were recorded, as well as behavioral abnormalities. Anorexia was scored at two levels according to fruit or pellet consumption. General observations were recorded using a dedicated grid adapted to the monitoring of general behavior, skin lesions, and mucosal lesions (mouth, eyes, and anorectal). Detected lesions were identified and scored depending on their location, severity, and number. Rectal bleeding and exudate were also reported and scored. Body weight, lymphadenomegaly, and rectal temperature were also recorded. The compilation of these observations was graded as a longitudinal follow-up. Blood cell counts, hemoglobin, and hematocrit were determined from EDTA blood using a DXH800 analyzer (Beckman Coulter).
IgG and IgA antibody quantification assay
Cynomolgus macaque serum and seminal plasma samples were screened for quantitative measurement of IgG antibodies to antigens from MPXV and VACV using the V-PLEX Orthopoxvirus Panel 1 (IgG) Kit (Meso Scale Discovery, Rockville, USA: MSD) according to the manufacturer’s instructions. The V-PLEX Orthopoxvirus Panel 1 (IgG) Kit contains MPXV antigens A29, A35, B6, E8, and M1 and VACV antigens A27, A33, B5, D8, and L1. The plates were blocked with 50 μL blocker A (1% BSA in MilliQ water) solution for at least 30 min at room temperature (RT) with shaking at 700 rpm using a digital microplate shaker. During blocking, heat-inactivated serum samples were diluted 1:500 or 1:50,000 in diluent buffer, and heat-inactivated seminal plasma samples were diluted at 1:10, 1:50, or 1:250. Each plate contained duplicate wells of a seven-point calibration curve with serial dilutions of a reference standard and a blank well. Plates were then washed three times with 150 μL MSD kit wash buffer and blotted dry. 50 μL of the diluted samples was added, and the plates were incubated at RT for at least 2 h with shaking at 700 rpm. Plates were again washed three times, 50 μL SULFO-Tagged anti-human IgG antibody were added to each well, and the plates were incubated at RT for at least 1 h with shaking at 700 rpm. Plates were then washed three times, and 150 μL MSD GOLD Read Buffer B was added to each well. The plates were read immediately using a MESO QuickPlex SQ 120 machine. The electro-chemiluminescence (ECL) signal was recorded, and the results were expressed as arbitrary units (AU)/mL. For measurement of IgA, heat-inactivated sera were diluted 1:100 in diluent buffer, and heat-inactivated rectal fluid samples were used undiluted. The same protocol as for IgG quantification was followed with detection done using a SULFO-tagged anti-human IgA antibody. Analyses were performed using Discovery Workbench 4.0.12.
Evaluation of the MVA-specific neutralizing antibody response
MVA-neutralizing antibodies in serum samples were titrated according to the standard plaque reduction neutralization test (PRNT)74. Briefly, serum samples were subjected to serial two-fold dilutions in PBS in a total volume of 1 mL. The samples were mixed with 50 µL MVA-GFP (MVA expressing green fluorescent protein) to contain 1750 pfu/mL in the final mix, which was incubated for 1 h at 37 °C. The mixture was then diluted 10-fold, and 250 µL of the mixture was added in triplicate to DF1 cell (ATCC: CRL-3586) monolayers in six-well plates. Plates were incubated for 30 min at RT, and 2 mL of DMEM containing 5% FCS, 40 µg/L gentamicin, 2 mM glutamine, and 10 g/L agarose was then added. After solidification, plates were incubated at 37 °C in 5% CO2. Seventy-two hours later, GFP-positive plaques were counted. The neutralization titer is expressed as the reciprocal serum dilution that led to a 50% reduction in the number of plaques compared to the negative control (serum from naïve NHP). Vaccinia immune globulin (CNJ-016) was used in each experiment as a positive control.
Evaluation of VACV-specific and MPXV-specific neutralizing antibody responses
VACV-neutralizing antibodies in serum samples were titrated according to this protocol75. Serum samples were first incubated at 56 °C for 1 h to inactivate complement and virus and then subjected to two-fold serial dilutions in DMEM containing 0.5% FCS and ATB (100 IU penicillin/ml and 100 IU/ml streptomycin). The samples were mixed with an equal volume of VACV-107 containing approximately 35 pfu in 0.1 ml and incubated for 1 h at 37 °C. The mixture was then added in quadruplicate to Vero cell monolayers in DMEM containing 0.5% FCS and ATB. Forty-six hours later, viral plaques were counted. The neutralization titer is expressed as the reciprocal serum dilution that led to a 50% reduction in the number of plaques compared to the negative control (pool of inactivated sera from naïve NHPs). The threshold of the titration was 10. Standardized serum from smallpox-vaccinated humans (EDQM Y0000502 human vaccinia immunoglobulin) was used in each experiment as a positive control.
For the quantification of MPXV-neutralizing antibodies without complement, serum samples were first incubated at 56 °C for 1 h to inactivate complement and the virus and then subjected to two-fold serial dilutions in DMEM containing 0.5% FCS and ATB. Five hundred microliters of each dilution of the samples was mixed with 500 µL MPXV containing approximately 35 PFU in 0.1 ml and the mixture was incubated for 1 h at 37 °C. Then, 200 µL of each dilution was added in quadruplicate to Vero cell monolayers in 24-well plates. Plates were incubated for 2 h at 37 °C in 5% CO2, and then 600 µL DMEM containing 2.5% FCS, 1% ATB, and 0.8% carboxymethyl cellulose was added. Plates were incubated for 72 h at 37 °C in 5% CO2, and the viral plaques were counted. The neutralization titer is expressed as described for VACV neutralization.
Virus quantification by PCR in fluids and organs
Rectal, nasal, and seminal fluid and cutaneous swab samples were extracted using the QIAamp DNA Blood mini kit (Qiagen) with small modifications. Briefly, pre-extraction inactivation was performed in a BSL-3 facility by adding 200 µl of each sample to a tube containing 200 µl Qiagen buffer AL and 10 µL extraction/inhibition control DNA SPC 10-2 (Yakima Yellow-BHQ-1, Eurogentec), followed by 20 µL protease. The tubes were vortexed and incubated for 10 min at 70 °C to also inactivate the virus. Extraction was then performed as recommended, with elution in less than 100 µL of AE buffer.
Organ samples were extracted using the QIAamp DNA mini kit (Qiagen). Less than 25 mg of each organ (10 mg for spleen) was added to 80 µL PBS with two 3 mm tungsten balls (Qiagen), and the tissue was dissociated using a Tissue Lyser II® (Roche Diagnostics) with a 4 min 30 Hz cycle. One hundred microliters ATL buffer, 10 µL extraction and inhibition/control DNA SPC 10-2 (Yakima Yellow-BHQ-1, Eurogentec), and 20 µL proteinase K were added. Samples were vortexed and incubated at 56 °C, with the duration depending on the dissolution of the organs (1–12 h). Extraction was then performed as recommended, with elution in less than 100 µL AE buffer.
For the pan-MPXV PCR assays, each reaction consisted of 5 μl extracted DNA and 15 μl iTaq Universal Probes Supermix (BioRad), the Supermix containing 0.4 µM of each primer (Eurogentec: F: GGA-AAA6TGT-AAA-GAC-AAC-GAA-TAC-AG; R: GCT-ATC-ACA-TAA-TCT-GGA-AGC-GTA), and 0.2 µM probe (Eurogentec: Quasar 705 - AAG-CCG-TAA-TCT-ATG-TTG-TCT-ATC-GTG-TCC - BHQ®-3) in the pan-MPXV PCR and 1X SPC Mix (Yakima Yellow-BHQ®-1, Eurogentec). All assays were performed on a CFX96 thermocycler (BioRad). The data and results were analyzed and reported using BioRad CFX Maestro v2.3.
Detection and titration of the virus in cell culture
Samples were frozen/thawed three times and centrifuged at 1,500 x g for 5 min. All rectal fluids were homogenized and then passed through a 1.2 µm filter (Sartorius Ministart 17593 K). Filtered rectal fluid, nasal and seminal fluid, and cutaneous swab samples were diluted to various serial five-fold dilutions (from pure to 1/12,500, depending on the DNA titer measured for each sample) in DMEM containing 0.5% FCS, antibiotics, and antifungals (gentamycin: 2.5 µg/ml, Mycostatin: 10 U/mL, penicillin: 100 UI/ml, streptomycin: 100 µg/ml) to inhibit bacterial and fungal contamination. Monolayers of Vero cells in 24-well plates were inoculated with 200 μl diluted supernatants in quadruplicate for isolation and titration. Plates were incubated at 37 °C in 5% CO2 for 2 h, and then 600 µL DMEM containing 2.5% FCS, 1% ATB (100 IU penicillin/mL, and 100 IU/mL streptomycin), and 1.6% carboxymethyl cellulose was added. Plates were incubated at 37 °C in 5% CO2 and observed daily for cytopathic effects from days 3 to 7. Samples were considered negative for infectious virus in the absence of the appearance of lytic plaques by day 14.
Organs were dissociated in DMEM containing 0.5% FCS and ATB (100 IU penicillin/mL, and 100 IU/mL streptomycin) with two 3 mm tungsten balls (Qiagen) in a Tissue Lyser II® (Roche Diagnostics) with a 4 min, 30 Hz cycle. Dissociated samples were frozen/thawed three times and centrifuged at 1500 x g for 5 min. Monolayers of Vero cells in 24-well plates were inoculated with 200 µL of the diluted supernatants in quadruplicate for isolation and titration. The plates were incubated at 37 °C in 5% CO2 for 2 h, and then 600 µL DMEM containing 2.5% FCS, 1% ATB (100 IU penicillin/mL, and 100 IU/mL streptomycin), and 1.6% of carboxymethyl cellulose was added. Plates were incubated at 37 °C in 5% CO2 and observed daily for cytopathic effects from days 3 to 7. Samples were considered negative for infectious virus in the absence of the appearance of lytic plaques by day 14.
Histopathology
At necropsy, organs were fixed by immersion in 10% formalin solution for 48 h. Formalin-fixed samples were paraffin-embedded (FFPE) using a vacuum inclusion processor (Excelsior, ThermoScientific), cut into 4 µm (Microtome RM2255, Leica) slices, mounted on coated glass slides (Superfrost + , ThermoScientific), and stained with hematoxylin and eosin (H&E) using an automated staining processor (Autostainer ST5020, Leica). Each slide was then scanned using Axioscan microscope scanner (Zeiss) and observed using Zen software version 3.7 (Zeiss) by a certified veterinary pathologist (DVM, DESV-AP).
Immunohistochemistry
Serial sections of rectal mucosa and skin tissue were stained for CD3, CD20, CD68, calprotectin, and vaccinia virus. Briefly, the slides were deparaffinized and stained using a Ventana Ultra instrument (Roche) with CC1 antigen retrieval and 32 min incubation with the primary antibody. See the following Table 2 for the references.
In situ hybridization
Serial sections were stained for monkeypox, UBC, and DapB using a Ventana Ultra device and the following probes with the RNAScope® 2.5 Assay (ACDTM Bio), see Table 3.
Briefly, slides were deparaffinized and pretreated at 97 °C for 24 min in Cell Conditioning Buffer (Roche), followed by six amplification cycles, and then stained with purple chromogen (Discovery Purple Kit, Roche). Slides were then counterstained with Hematoxylin II (Roche).
Intracellular staining of PBMCs
T-cell responses were characterized by measuring the proportion of Peripheral Blood Mononuclear Cells (PBMCs) expressing IL-2, IL-17a, IFN-γ, TNF-α, CD137, and CD154 upon stimulation with MPXV IIb virus (see above) or MVATGN33.1 (Transgene). CD3, CD4, and CD8 antibodies were used as lineage markers. The Table 4 below recapitulates the references of the antibodies used.
One million PBMCs were cultured in complete medium (RPMI1640 Glutamax+, [Gibco], supplemented with 10% FBS and 5% penicillin-streptomycin) supplemented with co-stimulatory antibodies (FastImmune CD28/CD49d, Becton Dickinson). Then, cells were stimulated with the virus at a final concentration of 0.3 pfu/cell. Brefeldin A was added to each well 5 hours later to a final concentration of 10 μg/mL, and the plate was incubated at 37 °C in 5% CO2 for an additional 13 h. Cells were then washed, stained with a viability dye (LIVE/DEAD Fixable Blue Dead Cell Stain Kit, Thermo Fisher), and fixed and permeabilized with BD Cytofix/Cytoperm reagent. Permeabilized cells were stored at −80 °C before the staining procedure. Antibody staining was performed in a single step following thawing. After 30 minutes of incubation at 4 °C in the dark, cells were washed in BD Perm/Wash buffer, and the data were acquired using the ZE5 flow cytometer (Bio-Rad) and analyzed using FlowJo v10 software. The gating strategy used to quantify each cytokine production in CD4 and CD8 cells is described (Fig. S18).
Data and statistical analysis
Data were analyzed using Prism v10 (GraphPad). Comparisons were performed using a Kruskal-Wallis test, followed by a non-parametric two-sided Mann-Whitney test. For the statistical analysis of the area under the curve for the virus in rectal fluid, the value of 0 was replaced by 1 for representation and statistics. Correlation analysis was done using a two-tailed non-parametric Spearman correlation test.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data that support the findings of this study are provided a a source data Excel file. All the data generated in this study have been deposited in the Figshare database with the DOI: 10.6084/m9.figshare.29402057. Source data are provided with this paper.
References
Gessain, A., Nakoune, E. & Yazdanpanah, Y. Monkeypox. N. Engl. J. Med. 387, 1783–1793 (2022).
World-Health-Organization. WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. https://www.who.int/azerbaijan/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern, (2022).
Ward, T. et al. Understanding the infection severity and epidemiological characteristics of mpox in the UK. Nat. Commun. 15, 2199 (2024).
Girometti, N. et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect. Dis. 22, 1321–1328 (2022).
Thornhill, J. P., Antinori, A. & Orkin, C. M. Monkeypox virus infection across 16 countries - April-June 2022. Reply. N. Engl. J. Med. 387, e69 (2022).
Ogoina, D. et al. Clinical course and outcome of human monkeypox in Nigeria. Clin. Infect. Dis. 71, e210–e214 (2020).
Huhn, G. D. et al. Clinical characteristics of human monkeypox, and risk factors for severe disease. Clin. Infect. Dis. 41, 1742–1751 (2005).
Bogacka, A. et al. Mpox unveiled: global epidemiology, treatment advances, and prevention strategies. One Health 20, 101030 (2025).
Musumeci, S., Laflamme, J., Kaiser, L., Segeral, O. & Calmy, A. Characteristics of possible mpox reinfection cases: literature review. J. Travel Med. 30, taad136 (2023).
Hazra, A. et al. Mpox in people with past infection or a complete vaccination course: a global case series. Lancet Infect. Dis. 24, 57–64 (2024).
Ahmed, Z. L. & Islam, M. R. The emergence of a novel mpox virus strain (clade Ib) in Central Africa: a global public health concern. J. Infect. Public Health 18, 102781 (2025).
Vakaniaki, E. H., et al. Sustained human outbreak of a new MPXV clade I lineage in eastern Democratic Republic of the Congo. Nat. Med. 30, 2791–2795 2024).
Allan-Blitz, L. T. et al. A position statement on Mpox as a sexually transmitted disease. Clin. Infect. Dis. 76, 1508–1512 (2023).
Hazra, A. & Cherabie, J. N. Is Mpox a sexually transmitted infection? Why narrowing the scope of this disease may be harmful. Clin. Infect. Dis. 76, 1504–1507 (2023).
Low, N. et al. Mpox virus and transmission through sexual contact: defining the research agenda. PLoS Med. 20, e1004163 (2023).
Mitjà, O. et al. Mpox in people with advanced HIV infection: a global case series. Lancet 401, 939–949 (2023).
Angelo, K. M. et al. Epidemiological and clinical characteristics of patients with monkeypox in the GeoSentinel Network: a cross-sectional study. Lancet Infect. Dis. 23, 196–206 (2023).
Philpott, D. et al. Epidemiologic and clinical characteristics of monkeypox cases—United States, May 17-July 22, 2022. MMWR Morb. Mortal. Wkly. Rep. 71, 1018–1022 (2022).
Silva, M. S. T. et al. Mpox, sexually transmitted infections and combination prevention: insights from a major cohort in Rio de Janeiro, Brazil. Aids 38, 1845–1849 (2024).
World-Health-Organization. Vaccins et vaccination contre la variole simienne: orientations provisoires, 16 novembre 2022. https://www.who.int/fr/publications/i/item/WHO-MPX-Immunization, (2022).
Prevention, C.f.D.C.a. Mpox Vaccine Recommendations. https://www.cdc.gov/poxvirus/mpox/vaccines/vaccine-recommendations.html, (2024).
European-Center-for-Disease-Prevention-and-Control. Public health considerations for mpox in EU/EEA countries. https://www.ecdc.europa.eu/en/publications-data/public-health-considerations-mpox-eueea-countries, (2023).
Verheust, C., Goossens, M., Pauwels, K. & Breyer, D. Biosafety aspects of modified vaccinia virus Ankara (MVA)-based vectors used for gene therapy or vaccination. Vaccine 30, 2623–2632 (2012).
Nave, L. et al. Immunogenicity and safety of modified vaccinia Ankara (MVA) vaccine—a systematic review and meta-analysis of randomized controlled trials. Vaccines 11, 1410 (2023).
Frey, S. E., Goll, J. B. & Beigel, J. H. Erythema and induration after Mpox (JYNNEOS) vaccination Revisited. N. Engl. J. Med. 388, 1432–1435 (2023).
Hillus, D. et al. Safety and effectiveness of MVA-BN vaccination against mpox in at-risk individuals in Germany (SEMVAc and TEMVAc): a combined prospective and retrospective cohort study. Lancet Infect. Dis. 25, 775-787 (2025).
Haverkate, M. R. et al. Factors potentially contributing to the decline of the mpox outbreak in the Netherlands, 2022 and 2023. Eur. Surveill. 29, 2300608 (2024).
Yeganeh, N., et al. Effectiveness of JYNNEOS vaccine against symptomatic mpox disease in adult men in Los Angeles County, August 29, 2022 to January 1, 2023. Vaccine 42, 125987 (2024).
Deputy, N. P. et al. Vaccine effectiveness of JYNNEOS against Mpox disease in the United States. N. Engl. J. Med.388, 2434–2443 (2023).
Dalton, A. F. et al. Estimated effectiveness of JYNNEOS vaccine in preventing Mpox: a multijurisdictional case-control study—United States, August 19, 2022-March 31, 2023. MMWR Morb. Mortal. Wkly. Rep. 72, 553–558 (2023).
Charles, H. et al. Mpox epidemiology and vaccine effectiveness, England, 2023. Emerg. Infect. Dis. 30, 2145–2148 (2024).
Rosenberg, E. S. et al. Effectiveness of JYNNEOS vaccine against diagnosed Mpox infection—New York, 2022. MMWR Morb. Mortal. Wkly. Rep. 72, 559–563 (2023).
Rao, A. K. et al. Use of JYNNEOS (Smallpox and Mpox Vaccine, Live, Nonreplicating) for persons aged ≥18 years at risk for Mpox during an Mpox outbreak: recommendations of the advisory committee on immunization practices—United States, 2023. MMWR Morb. Mortal. Wkly. Rep. 74, 385–392 (2025).
Berry, M. T. et al. Predicting vaccine effectiveness for mpox. Nat. Commun. 15, 3856 (2024).
Fontán-Vela, M. et al. Effectiveness of modified vaccinia Ankara-Bavaria nordic vaccination in a population at high risk of Mpox: a Spanish cohort study. Clin. Infect. Dis. 78, 476–483 (2024).
Mazzotta, V. et al. Immunogenicity and reactogenicity of modified vaccinia Ankara pre-exposure vaccination against mpox according to previous smallpox vaccine exposure and HIV infection: prospective cohort study. EClinicalMedicine 68, 102420 (2024).
Guagliardo, S. A. J. et al. Monkeypox virus infections after 2 preexposure doses of JYNNEOS vaccine—United States, May 2022-May 2024. MMWR Morb. Mortal. Wkly Rep. 73, 460–466 (2024).
Phipps, K., et al. Short-lived neutralizing antibody responses to monkeypox virus in smallpox vaccine-naive persons after JYNNEOS vaccination. Emerg. Infect. Dis. 31, 237-245 (2025).
Collier, A. Y. et al. Decline of Mpox antibody responses after modified vaccinia Ankara-Bavarian nordic vaccination. Jama 332, 1669–1672 (2024).
Selverian, C. N., et al. MPXV infection stimulates a more robust and durable neutralizing antibody response compared to MVA-BN vaccination. J. Infect. Dis. 231, 1069-1073 (2024).
Wiedemann, A. et al. Characterization and comparison of immunity against MPXV for individuals infected with MPXV or vaccinated with modified vaccinia Ankara vaccines. J. Immunol. 214, 211–222 (2025).
Jacob-Dolan, C. et al. Comparison of the immunogenicity and protective efficacy of ACAM2000, MVA, and vectored subunit vaccines for Mpox in rhesus macaques. Sci. Transl. Med. 16, eadl4317 (2024).
Aid, M. et al. Mpox infection protects against re-challenge in rhesus macaques. Cell 186, 4652–4661.e4613 (2023).
Li, Q. et al. Mpox virus Clade IIb infected Cynomolgus macaques via mimic natural infection routes closely resembled human Mpox infection. Emerg. Microbes Infect. 13, 2332669 (2024).
Frenois-Veyrat, G. et al. Tecovirimat is effective against human monkeypox virus in vitro at nanomolar concentrations. Nat. Microbiol. 7, 1951–1955 (2022).
Otter, A. D. et al. Monkeypox virus-infected individuals mount comparable humoral immune responses as Smallpox-vaccinated individuals. Nat. Commun. 14, 5948 (2023).
Shen-Gunther, J., Cai, H. & Wang, Y. Genomic and antigenic differences between monkeypox virus and vaccinia vaccines: insights and implications for vaccinology. Int. J. Mol. Sci. 26, 1428 (2025).
Pittman, P. R. et al. Phase 3 efficacy trial of modified vaccinia ankara as a vaccine against smallpox. N. Engl. J. Med. 381, 1897–1908 (2019).
Bravo-Vázquez, L. A., Bernal-Vázquez, D., Duttaroy, A. K. & Paul, S. Current status of next-generation vaccines against mpox virus: a scoping review. Front. Pharm. 16, 1533533 (2025).
Ravanello, M. P. & Hruby, D. E. Characterization of the vaccinia virus L1R myristylprotein as a component of the intracellular virion envelope. J. Gen. Virol. 75, 1479–1483 (1994).
Davies, D. H. et al. Antibody profiling by proteome microarray reveals the immunogenicity of the attenuated smallpox vaccine modified vaccinia virus ankara is comparable to that of Dryvax. J. Virol. 82, 652–663 (2008).
He, Y. et al. Recombinant A27 protein synergizes with modified vaccinia Ankara in conferring protection against a lethal vaccinia virus challenge. Vaccine 28, 699–706 (2010).
Grifoni, A. et al. Defining antigen targets to dissect vaccinia virus and monkeypox virus-specific T cell responses in humans. Cell Host Microbe 30, 1662–1670.e1664 (2022).
Edghill-Smith, Y. et al. Smallpox vaccine does not protect macaques with AIDS from a lethal monkeypox virus challenge. J. Infect. Dis. 191, 372–381 (2005).
Mucker, E. M. et al. Comparison of protection against mpox following mRNA or modified vaccinia Ankara vaccination in nonhuman primates. Cell 187, 5540–5553.e5510 (2024).
Thornhill, J. P. et al. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet 400, 1953–1965 (2022).
Antinori, A. et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Eur. Surveill. 27, 2200421 (2022).
Alcamí, A. Pathogenesis of the circulating mpox virus and its adaptation to humans. Proc. Natl. Acad. Sci. USA 120, e2301662120 (2023).
World-Health-Organization. WHO Director-General declares mpox outbreak a public health emergency of international concern. https://www.who.int/news/item/14-08-2024-who-director-general-declares-mpox-outbreak-a-public-health-emergency-of-international-concern, (2024).
Golden, J. W. & Hooper, J. W. Heterogeneity in the A33 protein impacts the cross-protective efficacy of a candidate smallpox DNA vaccine. Virology 377, 19–29 (2008).
Raccagni, A. R. et al. Two individuals with potential monkeypox virus reinfection. Lancet Infect. Dis. 23, 522–524 (2023).
Martínez-Sanz, J. et al. Description of mpox reinfection by whole genome sequencing. Int J. Infect. Dis. 137, 111–113 (2023).
World-Health-Organization. Mpox (monkeypox). https://www.who.int/news-room/fact-sheets/detail/monkeypox, (2022).
Centers-for-Disease-Control-and-Prevention. Mpox Vaccine Recommendations. https://www.cdc.gov/poxvirus/mpox/vaccines/vaccine-recommendations.html, (2024).
Olson, V. A. et al. Real-time PCR system for detection of orthopoxviruses and simultaneous identification of smallpox virus. J. Clin. Microbiol. 42, 1940–1946 (2004).
Sayers, E. W. et al. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res. 50, D20–d26 (2022).
Aksamentov, I., Roemer, C., Hodcroft, E. & Neher, R. Nextclade: clade assignment, mutation calling and quality control for viral genomes. J. Open Source Softw. 6, 3773 (2021).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068–2069 (2014).
Katoh, K. & Standley, D. M. MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol. Biol. Evol. 30, 772–780 (2013).
Waterhouse, A. M., Procter, J. B., Martin, D. M., Clamp, M. & Barton, G. J. Jalview Version 2-a multiple sequence alignment editor and analysis workbench. Bioinformatics 25, 1189–1191 (2009).
Minh, B. Q. et al. IQ-TREE 2: new models and efficient methods for phylogenetic inference in the genomic era. Mol. Biol. Evol. 37, 1530–1534 (2020).
Kalyaanamoorthy, S., Minh, B. Q., Wong, T. K. F., von Haeseler, A. & Jermiin, L. S. ModelFinder: fast model selection for accurate phylogenetic estimates. Nat. Methods 14, 587–589 (2017).
Huerta-Cepas, J., Serra, F. & Bork, P. ETE 3: reconstruction, analysis, and visualization of phylogenomic data. Mol. Biol. Evol. 33, 1635–1638 (2016).
Cosma, A. et al. Neutralization assay using a modified vaccinia virus Ankara vector expressing the green fluorescent protein is a high-throughput method to monitor the humoral immune response against vaccinia virus. Clin. Diagn. Lab. Immunol. 11, 406–410 (2004).
Leparc-Goffart, I. et al. Standardization of a neutralizing anti-vaccinia antibodies titration method: an essential step for titration of vaccinia immunoglobulins and smallpox vaccines evaluation. J. Clin. Virol. 32, 47–52 (2005).
Acknowledgements
This work was funded by the ANRS-MIE through the call for funding “Flash mpox 2022” (R.L.G. and J-N.T.). The IDMIT infrastructure has been supported by the Programme Investissements d’Avenir (PIA), managed by the ANR under reference ANR-11-INBS-0008 and the RESILIENCE-R-2023 project (Grant agreement n. 101168024) of the European Defence Fund. Views and opinions expressed are those of the authors and do not necessarily reflect those of the European Union or the European Defence Fund. Neither the European Union nor the granting authority can be held responsible for them. The National Reference Center for Orthopoxvirus (CNR-LE OPXV) is supported by Santé Publique France. The MVA-N33.1 vaccine was developed and provided by Transgene. We thank Julien Lemaitre, Audrey Bobillier, Claire-Maëlle Fovet, Quentin Sconosciuti, Emma Burban, Victor Magneron, Maxime Potier, Jean-Marie Robert, Eleana Navarre, Flavie Misplon, Eleonore Sizun, Thierry Prot, Antoine Carlotti, and Mallory Lassance for the NHP experiments; Sophie Luccantoni for the histology, immunohistochemistry, and RNAscope experiments; Julie Morin and Laura Junges for the ECL assay and reagent preparation; Matthieu Van Tilbeurgh, Marco Leonec, and Sarah Duquesne for the flow cytometry experiments; Julien Dinh, Alexandre Baillet, Léo Joffroy, and Elodie Guyon for NHP sample processing; Eric Quéméneur, Geneviève Inchauspé, Frédéric Iseni, Thibaut Naninck, Vanessa Contreras, and Romain Marlin for scientific support; Annonciade Molinet, Marc Grandadam, Frédéric Ducancel, Alicia Pouget, Sylvie Legendre, and Yann Gorin for their help with the logistics and safety management; Isabelle Mangeot and Salomé Piault for their help with resource management; and Brice Targat and Karl-Stephan Baczowski for their contribution to the data management.
Author information
Authors and Affiliations
Contributions
C.H. contributed to the project conception and design of the study, contributed to animal work, the coordination of the experiments, data analysis, figure design, and wrote the manuscript. A.F.R.: contributed to the project conception and design of the study, the coordination and realization of the in vitro experiments including qPCR, seroneutralization assay and infectivity assay, data analysis and the writing of the manuscript. F.R. contributed to the project conception and the design of the study, coordinated the animal core facility and contributed to animal work, data analysis and the writing of the manuscript. A.S.G. coordinated the cytometry core facility and contributed to data analysis and the writing of the manuscript. Q.P. contributed to the design of the study and supervised and contributed to histopathology analysis and data analysis, and the writing of the manuscript. H.L contributed to the project conception and design of the study, contributed to the coordination of the experiments, data analysis and the writing of the manuscript. M.C. contributed to antibody response analysis by coordinating experiments and data analysis, and the writing of the manuscript. N.DB. coordinated the immunology and infectiology core facility and contributed to the analysis of the data and the writing of the manuscript. W.G. performed flow cytometry experiments and data analysis. B.D. contributed to the project conception and design of the study, and contributed to animal work and data analysis. S.L. contributed to animal work and data analysis. H.T. and F.J. contributed to qPCR, seroneutralization assay and infectivity assay and data analysis. L.B. performed the MSD data experiments and data analysis. C.L. performed the histopathology experiments. C.B. performed seroneutralization experiments and data analysis. M.L. contributed to sequence data analysis, figure design and the writing of the manuscript. O.F. contributed to writing of the manuscript. N.S. contributed to project conception and the design of the study, seroneutralization assay and data analysis, and the writing of the manuscript. R.L.G. conceived the project, designed the study, coordinated the work, analyzed the data, and wrote the manuscript. J-N.T. conceived the project, designed the study, coordinated the work, analyzed the data, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
Nathalie Silvestre and Catherine Brua are Transgene employees and may hold shares and/or stock options in the company. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Herate, C., Ferrier-Rembert, A., Relouzat, F. et al. Efficacy of modified-vaccinia Ankara vaccine as pre- and post-exposure prophylaxis against monkeypox sexual transmission in non-human primate model. Nat Commun 16, 7306 (2025). https://doi.org/10.1038/s41467-025-62681-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-62681-2